Published on February 19, 2024
For all nutrients for which we can define a plateau, the determination of the nutrient requirement follows directly from these behaviors; an intake sufficient to get 97.5% of a healthy population up onto the effect plateau is, manifestly, a defensible estimate of the requirement.
Key Points
- Another way of determining a nutrient requirement is the effect plateau – if you start from a state of nutrient deficiency, increasing intake of the nutrient concerned produces a measurable, beneficial change in some function or outcome that expresses the nutrient’s activity, until the body’s need for that nutrient is met and a plateau is reached. Beyond this point no additional response is seen.
- For all nutrients for which we can define a plateau, the determination of the nutrient requirement – the “recommended” intake – follows directly from these behaviors. An intake sufficient to get 97.5% of a healthy population up onto the effect plateau is, manifestly, a defensible estimate of the requirement.
- In its 2011 intake recommendations, the Institute of Medicine (IOM) used the plateau effect as a part of the basis for its recommendation for vitamin D; unfortunately, the IOM panel relied on absorption studies that did not use a nutritionally relevant calcium load. As a result they greatly underestimated the vitamin D status needed to guarantee optimal regulation of calcium absorption.
- Vitamin D affects much more than calcium absorption, by virtue of regulating nearly 3000 protein coding genes. How much vitamin D intake is required, on a daily basis, to ensure that enough 25OHD is in the blood to satisfy the needs of all of the genes regulated by vitamin D when they require vitamin D? Read the additional comments by Dr. Patrick McCullough
 Written by Robert P. Heaney, M.D., review and comments by Patrick McCullough, M.D.
Written by Robert P. Heaney, M.D., review and comments by Patrick McCullough, M.D.
In this post we pursue yet another way of determining a nutrient requirement.
A feature common to most (if not all) nutrients is the effect plateau. If you start from a state of nutrient deficiency, increasing intake of the nutrient concerned produces a measurable, beneficial change in some function or outcome that expresses the nutrient’s activity. For example, if you have iron deficiency anemia and you start taking iron supplements, your hemoglobin and red blood cell count will increase. Your anemia will be treated and, in most cases, cured entirely. But there is a clear limit. Once your hemoglobin reaches normal values (about 14 g/100 mL of blood), no further increases can be produced by taking more iron – even if you double or triple or quadruple the dose. You have reached a plateau. If you’re losing iron (as with heavy menstrual flow), you’ll need to take a maintenance dose of iron. A dose (actually, better: an iron intake) that is just sufficient to keep your hemoglobin up on its plateau is the intake that satisfies your body’s need for iron. It is your “iron requirement”. This behavior of hemoglobin in response to iron intake is depicted in the figure, in which “intake” refers to iron status and “response” to blood hemoglobin concentration. The actual value of the requirement will vary from person to person and from time to time in an individual, depending on how much iron one’s body is losing every day.
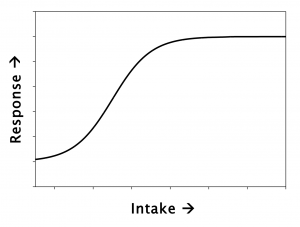 Because iron is a building block of the hemoglobin molecule, if you don’t have enough iron you won’t have enough hemoglobin – i.e., you will be anemic. The same is true for calcium and bone. A newborn human baby’s body contains 25–30 grams of calcium. That mass will increase to 1000–1500 grams by the time the child reaches full adult status. All that additional calcium has to come in by mouth. If after weaning you rear experimental animals on diets with varying calcium contents, and measure how much bone they have when fully grown, you will get a curve that’s exactly the same as the one shown above. And like iron, once you’re on the plateau, extra calcium will produce no more bone.
Because iron is a building block of the hemoglobin molecule, if you don’t have enough iron you won’t have enough hemoglobin – i.e., you will be anemic. The same is true for calcium and bone. A newborn human baby’s body contains 25–30 grams of calcium. That mass will increase to 1000–1500 grams by the time the child reaches full adult status. All that additional calcium has to come in by mouth. If after weaning you rear experimental animals on diets with varying calcium contents, and measure how much bone they have when fully grown, you will get a curve that’s exactly the same as the one shown above. And like iron, once you’re on the plateau, extra calcium will produce no more bone.
This behavior is relatively intuitive for bulk nutrients such as iron and calcium. But it’s also true for nutrients that are not so much accumulated by the body as utilized in helping the body perform some key function. Vitamin D, for example, helps the body regulate intestinal absorption of calcium from the foods in our diets. When a person is vitamin D deficient, calcium absorption will be impaired – i.e., it will fall somewhere along the ascending limb of the curve in the figure. But once you’ve raised your vitamin D status and have absorbed as much calcium as your body needs, increasing vitamin D status has no further effect. You’ve reached the absorptive plateau.
[Actually, vitamin D doesn’t raise calcium absorption at all – as we once used to think. Instead, what it does is enable the body to increase calcium absorption when the body needs more calcium – but has no effect when the body has enough. That’s why, once you’re up on the absorptive plateau, no further absorption occurs. Knowledgeable readers will recall that there is a derivative of vitamin D, called calcitriol, which the body makes when it needs to augment calcium absorption and which does, indeed, increase calcium absorption directly (and essentially without limit). If you were to administer calcitriol – sometimes referred to as “active” or “activated” vitamin D – you would definitely increase calcium absorption, whether the body needed the calcium or not. But it’s not the native vitamin D that’s producing this effect. Dosing with calcitriol effectively bypasses the body’s regulatory controls. The reason why normally the body does not increase calcium absorption as vitamin D intakes rise is precisely because the body reduces its production of calcitriol once calcium absorption is adequate for the body’s needs.]
While, as noted at the outset, this plateau effect appears to be common to most or all nutrients, there are some for which there isn’t an easily measurable effect, and therefore no direct way to get at defining the effect plateau. Protein, for example, is necessary for growth and for increasing muscle mass during growth. Like other nutrients, once a person reaches the amount of muscle that’s just right for his or her hereditary constitution and physical activity, more protein will not make more muscle. But muscle mass is difficult and expensive to measure – unlike hemoglobin (for iron). However, there is a potentially very useful substitute measure – plasma insulin-like growth factor-1 [IGF-1] – a member of the class of compounds called “biomarkers”. IGF-1 concentration in blood does reflect protein intake and follows the rising limb of the curve above, just as does hemoglobin with iron. The IGF-1 plateau is not as well studied nor quite as precisely nailed down as some of the other relationships I’ve just reviewed. However the basic pattern – the plateau – seems to be the same as for other nutrients. More research is clearly needed. But available data indicate the IGF-1 concentrations begin to plateau at protein intakes in the range of 1.2–1.3 grams protein/kilogram/day, a figure that is about 50% higher than the current recommendation for protein intake.
For all nutrients for which we can define a plateau, the determination of the nutrient requirement – the “recommended” intake – follows directly from these behaviors. An intake sufficient to get 97.5% of a healthy population up onto the effect plateau is, manifestly, a defensible estimate of the requirement (specifically, it would be the RDA).
Interestingly, in its 2011 intake recommendations, the Institute of Medicine (IOM) used the plateau effect as a part of the basis for its recommendation for vitamin D. The IOM asserted that a 25(OH)D level of 20 ng/mL was sufficient to ensure that most individuals would be on the calcium absorptive plateau. Unfortunately, the IOM panel relied on absorption studies that did not use a nutritionally relevant calcium load. As a result they greatly underestimated the vitamin D status needed to guarantee optimal regulation of calcium absorption. This is seen immediately when we recall that absorption is a load phenomenon, i.e., how many ions of calcium can be carried across the intestinal mucosa during the short time during which the digested food is in contact with the absorptive mucosa. Vitamin D (actually calcitriol in this instance) causes the intestinal lining cells to manufacture calcium transporters. Clearly, if you have fewer calcium ions to transport, you can max out with fewer transporters. It’s just that straightforward. As a consequence, it follows that if you want to optimize absorptive regulation for nutritionally relevant calcium sources (e.g., a glass of milk), you’ve got to do your testing using nutritionally relevant calcium loads. And when you do that, the absorptive plateau begins at 25(OH)D concentrations of 32–35 ng/mL, not 20 as the IOM declared.
Previous Posts by Dr. Heaney
Nutrition Doesn’t Know What “Normal” Is
Thermostats, Feedback, and Adaptation
Comments from Patrick McCullough, MD
Vitamin D affects much more than calcium absorption, by virtue of regulating nearly 3000 protein coding genes. We don’t yet know what all the gene products are and what the resulting effects are that they have. One question that immediately comes to mind is how much vitamin D intake is required, on a daily basis, to ensure that enough 25OHD is in the blood to satisfy the needs of all of the genes regulated by vitamin D when they require vitamin D.
This question was partially addressed in the 2019 dose-response study by Shirvani and Holick, et al. In this study, daily intake of 600 IU, 4000 IU and 10,000 IU for 6 months resulted in a graded increase in the number of vitamin D regulated genes detected at the 6 month time point. The numbers were 162, 320, and 1289 in the 3 groups. The dose-response study needs to be continued with higher daily intakes to see where the number of genes plateaus, and what that number is. Will it be 3000 genes? More? The minimum daily intake that results in maximum vitamin D gene regulation, reflected by flattening of the dose response curve, needs to also be determined. The argument could then be made that this dose should be considered the new minimum RDA for vitamin D, as it will assure sufficient vitamin D availability for all vitamin D regulated protein coding genes.
The data from the Shirvani and Holick study clearly shows that 600 IU per day is not sufficient for the needs of the body, contrary to the assertions made by the IOM in 2011, as many genes remain quiescent due to lack of adequate supply with this daily intake. This study also makes a strong argument to test these and higher doses in treating diseases known to be associated with vitamin D deficiency to determine the dose-response curve.
The minimum RDA calculated in the manner suggested above is likely to vary by age group, and other factors may also influence it. Vitamin D intakes higher than the minimum RDA based on gene activation data will likely increase the risk for the development of hypercalcemia. But this can be easily monitored by checking serum calcium concentrations periodically.
Many diseases that would otherwise respond to vitamin D remain uncontrolled when insufficient amounts of vitamin D are present in the blood. Patients with autoimmune diseases especially may need a higher daily vitamin D intake to keep the disease under control compared to other diseases. This is because the metabolism of vitamin D is likely very high and stays high in autoimmune diseases. In other words, the vitamin D gets used up quickly when combating an autoimmune disease, and a steady supply must be provided to keep the disease controlled.
Vitamin D doesn’t cure autoimmune diseases, but controls them.
The mechanism of action of vitamin D in controlling autoimmune diseases is likely two fold.
- There is good evidence that vitamin D regulates genes that control the formation of regulatory T lymphocytes (Tregs), which are known as the master regulators of the immune system. Tregs have been shown to control autoimmune diseases through a number of mechanisms. (C Mattozzi, 2013, Importance of regulatory T cells in the pathogenesis of psoriasis.)
- There is also very good evidence that topical and oral vitamin D, sunshine, and UVB phototherapy can all restore the functional status of dysfunctional Tregs. Without sufficient vitamin D, Tregs become dysfunctional, and control of autoimmune diseases is lost. See a discussion of this concept in my 2021 review paper: Oral and topical vitamin D, sunshine, and UVB phototherapy safely control psoriasis in patients with normal pretreatment serum 25OHD concentrations.
In the 1930s and 1940s reports first began to appear describing the successful use of vitamin D in curing rickets and tuberculosis infections, as well as in controlling asthma, psoriasis, and rheumatoid arthritis. Daily intake of doses ranging from 60,000 to 300,000 IU were used to control asthma, 100,000 to 150,000 IU per day for 2 to 3 months were used to cure tuberculosis, and 150,000 to 600,000 IU were used to control rheumatoid arthritis. Much lower doses were used to cure rickets.
The high doses used for controlling psoriasis, asthma, and rheumatoid arthritis, and for curing tuberculosis infections often resulted in symptomatic hypercalcemia, which caused the use of these high doses to be abandoned. Studies using lower dosing ranges to treat these diseases were not reported during that era. A daily dose of 400 IU per day was ultimately recommended for everyone, as this was effective in treating rickets and thought to be sufficient for the general population. However, it was ineffective at treating tuberculosis, asthma, psoriasis, or rheumatoid arthritis. This fits the concept expressed by Dr. Heaney very nicely. The intake of vitamin D needs to be greater than 400 IU per day to see a response in these diseases. This research has been done partially with asthma. Asthma has been shown not to respond to daily intake of 4000 IU of vitamin D a day over several months in at least 3 clinical trials since 2014. But there has been at least one case report showing that 25,000 IU per day resulted in markedly improved asthma control without complications in an individual with long-term asthma. More research needs to be done with daily vitamin D intakes ranging from at least 10,000 to 50,000 IU per day. These studies can be performed safely in a controlled clinical trial setting with IRB oversight and approval.
The doses used that resulted in hypercalcemia in the 1930s and 1940s were obviously in the plateau region; effective treatments but with adverse reactions. The range of vitamin intakes resulting in an effective response before plateauing needs to be determined for each disease. Interestingly, a review of tuberculosis clinical trials performed in the 1940s shows that the doses used to treat tuberculosis infections were tolerated well without adverse reactions and with complete cure of the infection. These trials need to be repeated today to see if they can be replicated. Would a lower amount, such as 50,000 IU per day over a period of time also be effective? How low can you go before vitamin D becomes ineffective at curing tuberculosis infections? Unlike the autoimmune disease psoriasis, a maintenance dose is not required, because the microorganism causing the disease is eradicated.
Vitamin D reproducibly causes psoriasis plaques to disappear, and a maintenance dose is required to keep the plaques from reforming. The same is true with UVB phototherapy. The daily intake of vitamin D needed to achieve remission needs to be determined. Anything beyond this amount is not required due to the plateau effect and is likely to increase the risk of adverse reactions. The daily intake of vitamin D that is more than enough to control psoriasis needs to be determined, and the daily intake of vitamin D needed once the effect is seen to keep the plaques from reappearing also needs to be determined.
The resulting serum 25OHD concentration needed to see an effect is also going to vary depending on the effect. Much more is likely going to be needed to control and maintain control of an autoimmune disease such as psoriasis than will be necessary to enable calcium absorption in the gut during a meal. The serum 25OHD concentrations need to be determined, and they are going to be much higher than what the IOM thinks is safe, or what is currently considered normal. See my psoriasis review paper here.
There is good evidence that vitamin D induced hypercalcemia does not occur until the serum 25OHD concentration gets above 400 ng/ml. This comes from the 2011 paper from Araki and Holick, et al, and is what I have observed in my clinical practice. See my 2019 paper, “Daily oral dosing of vitamin D3 using 5000 TO 50,000 international units a day in long-term hospitalized patients: Insights from a seven year experience.”
Learn more about Dr. Patrick McCullough here.
About Dr. Robert P. Heaney
 Dr. Heaney was a full time professor at Creighton University who also donated his time and energy, starting in 2012 until his passing in 2016, as Research Director at GrassrootsHealth. In this capacity Dr. Heaney consulted on studies, methodologies, and how to best change public health direction. Dr. Heaney provided nearly 50 years of advancements in our understanding of bone biology, osteoporosis, and human calcium and vitamin D physiology. He is the author of three books and has published over 400 original papers, chapters, monographs, and reviews in scientific and educational fields. At the same time, he has engaged nutritional policy issues and has helped redefine the context for estimating nutrient requirements. Dr. Heaney was presented a lifetime achievement award in the US House of Representatives on November 10, 2015 (Watch the video here). He was an inspiration to researchers everywhere – his intellect, dedication, integrity, and caring was unsurpassed.
Dr. Heaney was a full time professor at Creighton University who also donated his time and energy, starting in 2012 until his passing in 2016, as Research Director at GrassrootsHealth. In this capacity Dr. Heaney consulted on studies, methodologies, and how to best change public health direction. Dr. Heaney provided nearly 50 years of advancements in our understanding of bone biology, osteoporosis, and human calcium and vitamin D physiology. He is the author of three books and has published over 400 original papers, chapters, monographs, and reviews in scientific and educational fields. At the same time, he has engaged nutritional policy issues and has helped redefine the context for estimating nutrient requirements. Dr. Heaney was presented a lifetime achievement award in the US House of Representatives on November 10, 2015 (Watch the video here). He was an inspiration to researchers everywhere – his intellect, dedication, integrity, and caring was unsurpassed.
Read more about Dr. Heaney and a few of his accomplishments here.
How Are Your Levels of Important Nutrients?
Do you know what your vitamin D level is? Check yours along with omega-3s, magnesium, and other levels today as part of the vitamin D*action project; add the Ratios for more about how to balance your Omega-3s and 6s!
Measure your:
- Vitamin D
- Magnesium PLUS Elements
- Omega-3 Fatty Acids
- hsCRP (for Inflammation)
- HbA1c (for Blood Sugar)
- and more
Did you know that each of the above can be measured at home using a simple blood spot test? As part of our ongoing research project, you can order your home blood spot test kit to get your levels, followed by education and steps to take to help you reach your optimal target levels. Start by enrolling and ordering your kit to measure each of the above important markers, and make sure you are getting enough of each to support better mood and wellbeing!
Build your custom kit here – be sure to include your Omega-3 Index along with your vitamin D.
Start Here to Measure Your Levels