Published on July 7, 2021
Observations from recent studies cause concern for those with high triglycerides and at risk for cardiovascular disease
 Atrial fibrillation (also called Afib or AF), is an irregular, often rapid heart rate that can cause symptoms such as heart palpitations, shortness of breath, and weakness. It affects an estimated 2.7 million Americans and can lead to serious complications such as blood clots, stroke, heart failure, and other cardiovascular diseases, which may be fatal.
Atrial fibrillation (also called Afib or AF), is an irregular, often rapid heart rate that can cause symptoms such as heart palpitations, shortness of breath, and weakness. It affects an estimated 2.7 million Americans and can lead to serious complications such as blood clots, stroke, heart failure, and other cardiovascular diseases, which may be fatal.
Recent Studies Create Concern about Omega-3 Supplementation and AFib
Omega-3 fatty acids are well known to provide healthful benefits for the heart, reduce inflammation and reduce the risk of death. There have been many studies on the benefits of omega-3 fatty acids for cardiovascular health and the prevention of ischemic events. The VITAL trial, which focused on cancer and cardiovascular health, found several significant benefits among those assigned to omega-3s (1000 mg/day) vs. placebo. A meta-analysis of 40 randomized controlled trials that used supplementation of omega-3 fatty acids EPA and DHA found a preventive effect of supplementation on cardiovascular disease (CVD), with a stronger effect associated with higher doses, especially for CVD events and heart attack.
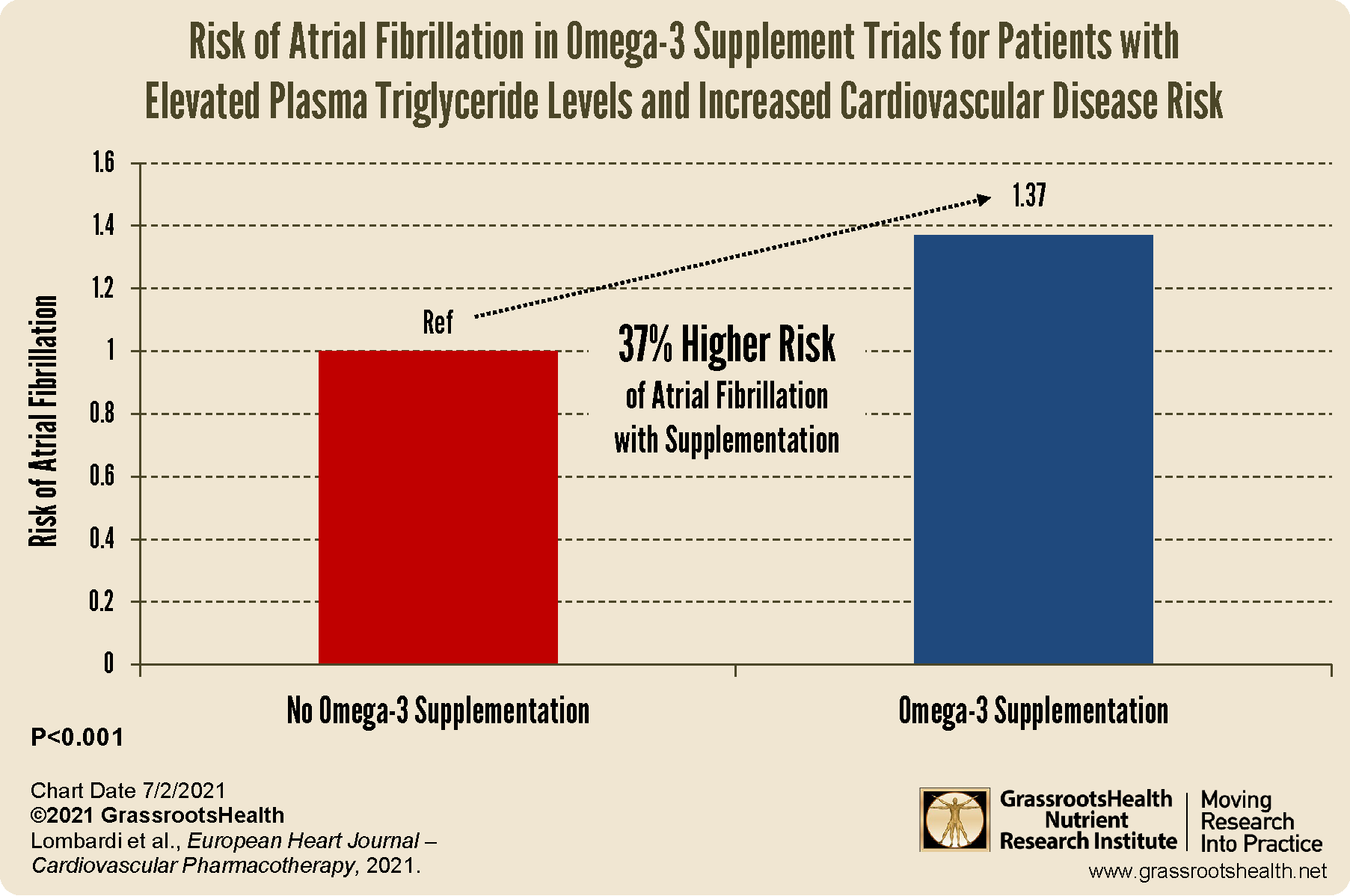
However, with more research now including higher doses of omega-3 fatty acids among supplementation groups, there is a new concern that omega-3 supplements may increase the risk of AFib among certain individuals with elevated CVD risk. A meta-analysis by Lombardi et al. looked at five randomized controlled trials to see if supplementation with omega-3 fatty acids was related to an increased risk of developing AFib. The study did find a 37% higher risk of AFib with supplementation compared to placebo (P<0.001), as illustrated in the chart below.
Based on these findings, the authors concluded that individuals with an increased risk of or current CVD, combined with elevated plasma triglycerides, may be at a higher risk for AFib when supplementing with omega-3 fatty acids.
However, it is important to note that there are significant limitations in these findings. These studies did not include AFib as an outcome measure which means that reports of AFib may be incomplete. Further, the risk of hemorrhage in these patients was unknown.
Could EPA Versus DHA Intake Make a Difference?
There is some evidence that the amount or type of EPA or DHA taken may play a role in the risk of AFib among those supplementing with omega-3 fatty acids. One trial showing a significantly higher risk of AFib, the REDUCE-IT trial, gave a form of EPA called icosapent ethyl without any DHA. Meanwhile, DHA specifically has been shown to lower triglyceride levels and improve heart health via a significant anti-inflammatory effect. A study by Kelley et al. highlighted the effects of DHA supplementation on inflammation in men with high blood levels of triglycerides, who were at high risk of developing heart disease, and found that the reduction in CRP concentrations was comparable to the 15-25% reduction in CRP caused by statins (the frontline pharmaceuticals used to prevent heart attacks and stroke) without any of the adverse effects.
Vitamin D and Magnesium Are Also Related to Afib
A meta-analysis published by Liu et al. looked at 13 studies with 6519 cases of AFib among 74,885 participants in order to identify a dose-specific relationship between vitamin D level and the risk of AFib or postoperative atrial fibrillation (POAF). The authors found that vitamin D levels below 30 ng/ml (75 nmol/L) were associated with an increased risk of AFib, whereas higher vitamin D levels were associated with a reduction in risk by 12% (p=0.03) for each 10 ng/ml (25 nmol/L).
Magnesium also plays several functional roles within cardiac muscle to regulate heart rate and contractions, and in some studies, has even been more effective at restoring the heart’s rhythm than standard pharmaceutical treatments. Magnesium status has been linked to the incidence and development of AFib, as shown in an analysis by Khan et al., which involved more than two decades of data from a total of 3,530 participants, to look at the link between serum magnesium and the development of AFib in those without existing cardiovascular disease. The incidence of AFib was highest in the quartile with the lowest magnesium level (P=0.02).
Could Magnesium be a Missing Link? Magnesium Shown to Lower Triglycerides and Work with Omega-3s for Heart Health
Statin drugs work to lower LDL cholesterol levels and help prevent CVD by blocking an enzyme (HMG CoA Reductase) that your body uses to make cholesterol. Similarly, when there is sufficient magnesium in the body, it works to inactivate this same enzyme though natural control mechanisms. In fact, magnesium has been shown to more reliably lower triglycerides than statin drugs while also raising HDL, with similar effects on clotting, plaque formation, and inflammation without the adverse effects and cost associated with statin drugs.
In addition to its role in activating vitamin D, magnesium activates other enzymes involved in lipid production, such as the conversion of omega-3 and omega-6 into prostaglandins which are important for cardiovascular and general health. In other words, magnesium is an important co-nutrient for omega-3s when it comes to heart health… might it be especially important to ensure adequate magnesium intake and status when supplementing with omega-3 fatty acids for your heart health?
Are You Getting Enough Vitamin D, Magnesium, and Omega-3s?
 Having and maintaining healthy vitamin D levels and other nutrient levels can help improve your health now and for your future. Choose which to measure, such as your vitamin D, omega-3s, and essential minerals including magnesium and zinc, by creating your custom home test kit today. Take steps to improve the status of each of these measurements to benefit your overall health. You can also track your own intakes, symptoms and results to see what works best for YOU.
Having and maintaining healthy vitamin D levels and other nutrient levels can help improve your health now and for your future. Choose which to measure, such as your vitamin D, omega-3s, and essential minerals including magnesium and zinc, by creating your custom home test kit today. Take steps to improve the status of each of these measurements to benefit your overall health. You can also track your own intakes, symptoms and results to see what works best for YOU.
Enroll and test your levels today, learn what steps to take to improve your status of vitamin D (see below) and other nutrients and blood markers, and take action! By enrolling in the GrassrootsHealth projects, you are not only contributing valuable information to everyone, you are also gaining knowledge about how you could improve your own health through measuring and tracking your nutrient status, and educating yourself on how to improve it.
Help everyone Move Research into Practice with vitamin D and other nutrients! As a special birthday gift to everyone, in honor of the science, we have created a special scholarship fund for anyone to donate to that will go towards helping others participate. Your donation will allow anyone to get help with funding their participation when they need it.
Text-to-give: Text Daction to 44321 to add to our Scholarship Fund.