Benefits may be most pronounced for Black women and patients diagnosed with later-stage disease
- Song Yao, PhD, led research effort to be highlighted during ASCO 2021 meeting
- New analysis based on Kaiser Permanente Northern California’s Pathways Study
- Higher vitamin D levels at diagnosis linked to better breast cancer outcomes
 Newswise — BUFFALO, N.Y. — The joint Roswell Park Comprehensive Cancer Center/Kaiser Permanente Northern California team behind a new study to be highlighted at the American Society of Clinical Oncology (ASCO) 2021 virtual annual meeting has found that sufficient vitamin D levels at the time of diagnosis are associated with improved outcomes among people with breast cancer.
Newswise — BUFFALO, N.Y. — The joint Roswell Park Comprehensive Cancer Center/Kaiser Permanente Northern California team behind a new study to be highlighted at the American Society of Clinical Oncology (ASCO) 2021 virtual annual meeting has found that sufficient vitamin D levels at the time of diagnosis are associated with improved outcomes among people with breast cancer.
The new research, presented by first author Song Yao, PhD, is based on Kaiser Permanente Northern California’s Pathways Study — a large prospective study in breast cancer patients that has been underway since 2006 under the direction of Larry Kushi, ScD, who is Senior Author on the new study. Dr. Yao highlighted the team’s findings in a poster discussion session today. The presentation is Clinically sufficient vitamin D levels at breast cancer diagnosis and survival outcomes in a prospective cohort of 3,995 patients after a median follow-up of 10 years (abstract 10510).
“Consistent with results from randomized trials and meta-analyses, our findings from this large, observational cohort of breast cancer survivors with long follow-up provide the strongest evidence to date for maintaining sufficient vitamin D levels in breast cancer patients, particularly among Black women and patients with more advanced stage disease,” notes Dr. Yao, a molecular epidemiologist and Professor of Oncology with the Department of Cancer Prevention and Control at Roswell Park.
“These findings highlight not just the role of vitamin D in breast cancer prognosis, but also the contribution of and need for prospective studies in cancer survivors to complement clinical trials,” says study Senior Author Lawrence Kushi, ScD, Director of Scientific Policy at the Kaiser Permanente Northern California Division of Research.
The research team measured 25-hydroxyvitamin D (25OHD) levels from 3,995 women with breast cancer who were enrolled in the Pathways Study, using blood serum samples collected at the time of diagnosis. They examined potential determinants of 25OHD levels, including polygenic score. Vitamin D supplement intake, BMI, and race/ethnicity were the most influential factors on serum 25OHD levels, while genetic variants had only a limited impact, notes Dr. Yao.
The study categorized vitamin D levels based on clinical cutoffs: deficient (< 20 ng/ml), insufficient (20 to < 30 ng/ml), or sufficient (≥30 ng/ml). Dr. Yao and colleagues then evaluated these levels in relation to overall survival (OS), breast cancer-specific survival (BCSS), recurrence-free survival (RFS), and invasive disease-free survival (IDFS) after a median follow-up time of 9.6 years. The researchers built Cox proportional hazards models adjusting for non-clinical, clinical and treatment factors that were further stratified by stage, estrogen receptor (ER) status and body mass index (BMI).
“Having clinically sufficient vitamin D levels at the time of breast cancer diagnosis is associated with better outcomes,” Dr. Yao notes. “While these results are consistent with our earlier analysis based on a subset of the study population, it’s significant that we saw the same trends in this much larger, longer-term data set — suggesting an ongoing benefit for patients who maintain sufficient levels through and beyond breast cancer treatment.”
The team also observed that associations were similar by ER status, and found that the association between vitamin D levels and breast cancer outcomes appeared to be stronger among study participants diagnosed at more advanced stages or with lower body mass index. Black women had the lowest vitamin D levels, which might contribute to their generally poorer outcomes after breast cancer diagnosis.
“In the context of supportive data from recent randomized trials and meta-analyses, our findings support the use of daily vitamin D supplementation to maintain sufficient vitamin D levels after breast cancer diagnosis, particularly among Black women and patients diagnosed with later-stage disease,” says senior author Christine Ambrosone, PhD, Co-Principal Investigator of the Pathways Study and Senior Vice President of Population Sciences and Chair of Cancer Prevention and Control at Roswell Park.
####
This news release is also available on the Roswell Park website: https://www.roswellpark.org/newsroom/202106-research-roswell-park-kaiser-permanente-supports-vitamin-d-supplementation-breast
Roswell Park Comprehensive Cancer Center is a community united by the drive to eliminate cancer’s grip on humanity by unlocking its secrets through personalized approaches and unleashing the healing power of hope. Founded by Dr. Roswell Park in 1898, it is the only National Cancer Institute-designated comprehensive cancer center in Upstate New York. Learn more at www.roswellpark.org, or contact us at 1-800-ROSWELL (1-800-767-9355) or [email protected].
Dr. Song Yao Discusses Previous Findings on Vitamin D and Breast Cancer
In this brief video, first author, Dr. Song Yao, shares previous findings about the positive link between vitamin D and breast cancer. The new study featured above further supports the findings discussed below.
These Findings Also Support Those of GrassrootsHealth
Previous publications from GrassrootsHealth have included
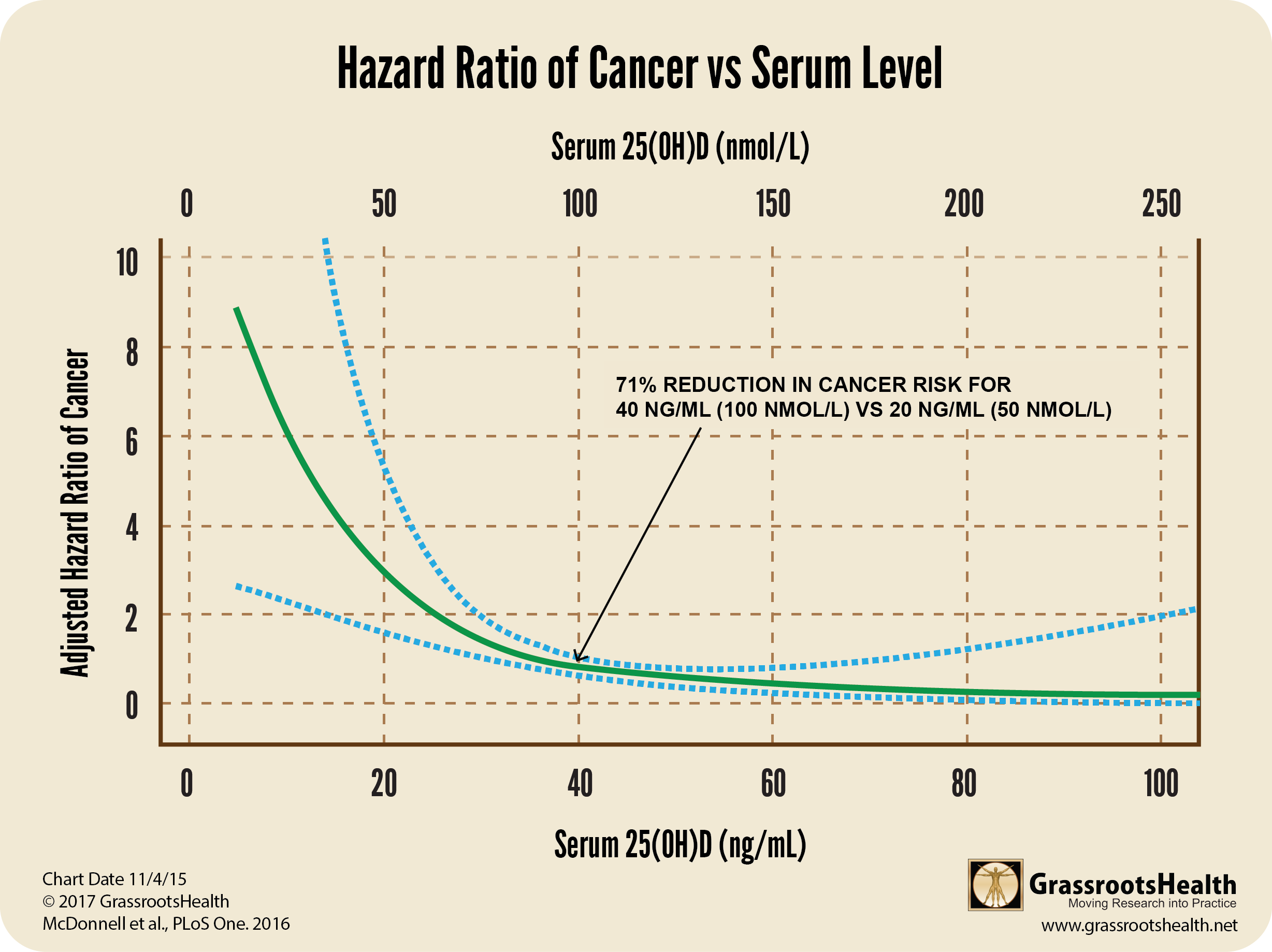
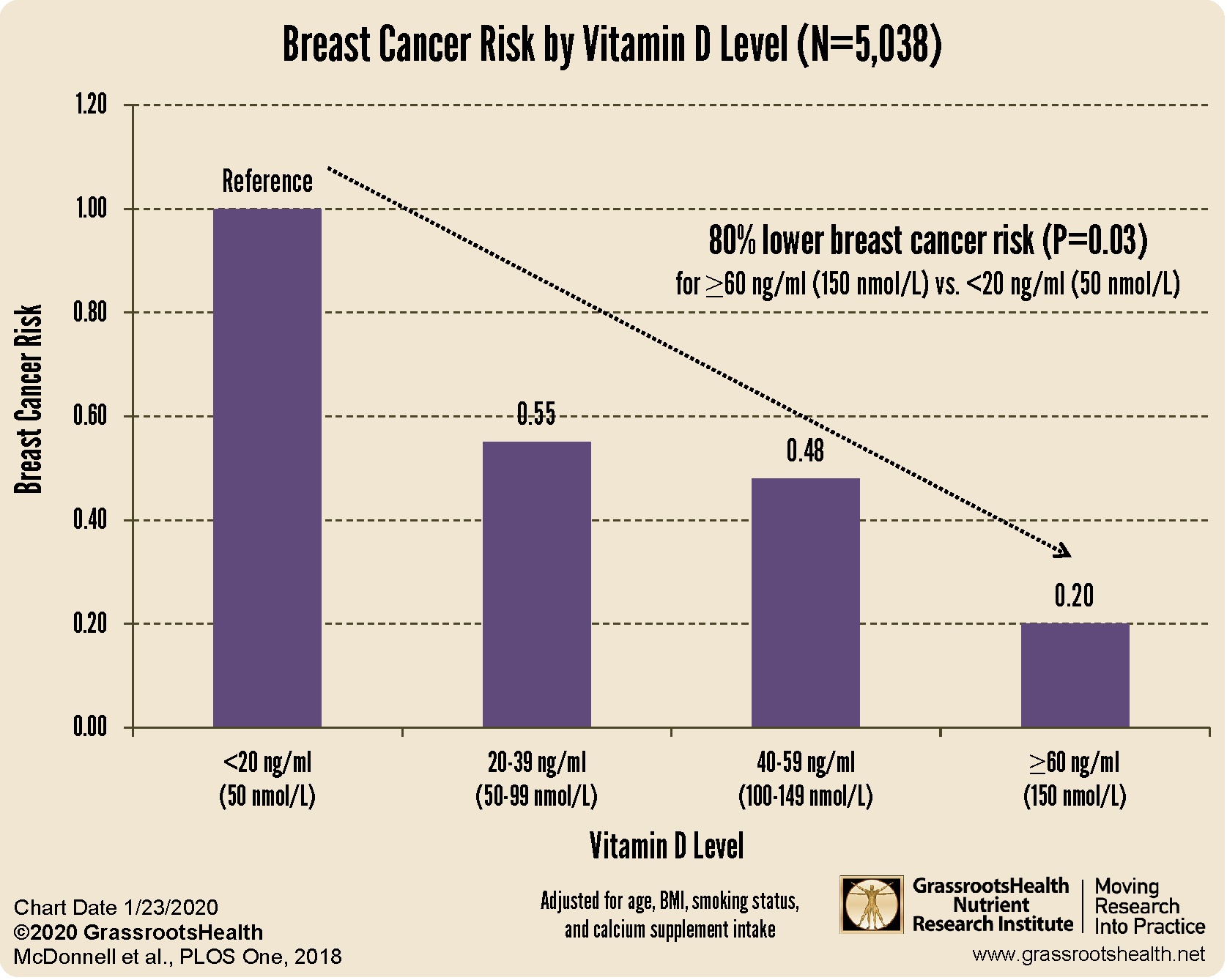
A 71% reduction in Breast Cancer incidence with a vitamin D level of at least 40 ng/ml (100 nmol/L)
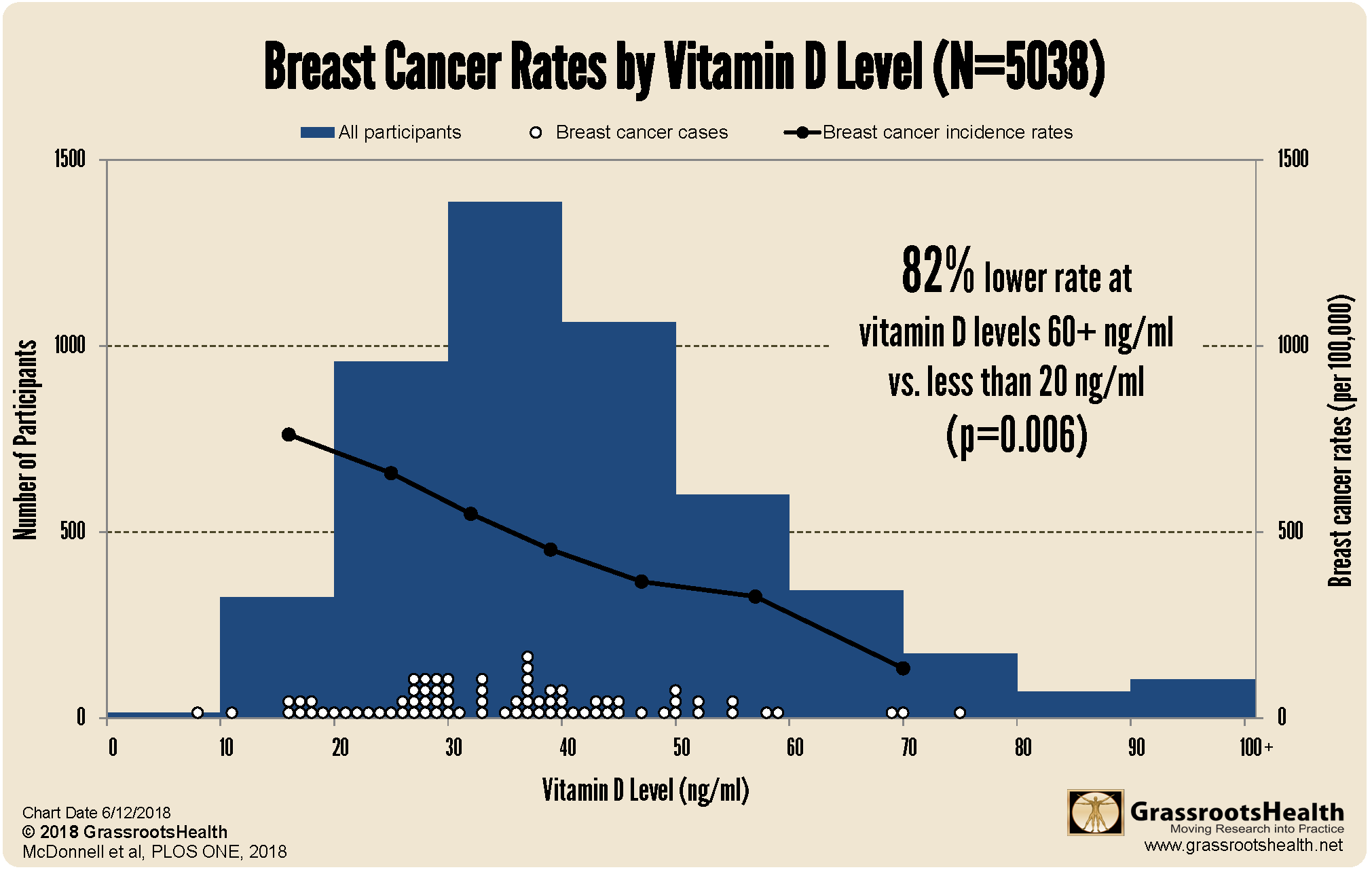
An 82% reduction with a vitamin D level of at least 60 ng/ml (150 nmol/L)
An 80% lower risk of breast cancer with vitamin D levels at or above 60 ng/ml (150 nmol/L)
Additionally, since breast cancers diagnosed in the first year were likely present but undiagnosed at the beginning of the study, we also repeated the analysis with only those without breast cancer at one year. We found that those with vitamin D levels at or above 60 ng/ml had a 93% lower risk of breast cancer compared to women with levels less than 20 ng/ml (P=0.02).
Overall, higher vitamin D levels were associated with decreased breast cancer risk, with levels at or above 60 ng/ml being the most protective.
Measure, Track & Learn Your Vitamin D Levels with the GrassrootsHealth Breast Cancer Prevention Project
Join the GrassrootsHealth Breast Cancer Prevention Project to measure your status of vitamin D and other chosen co-nutrients, learn how to improve and maintain your levels, and contribute your data to further the science.
Check Your Vitamin D Level Today!
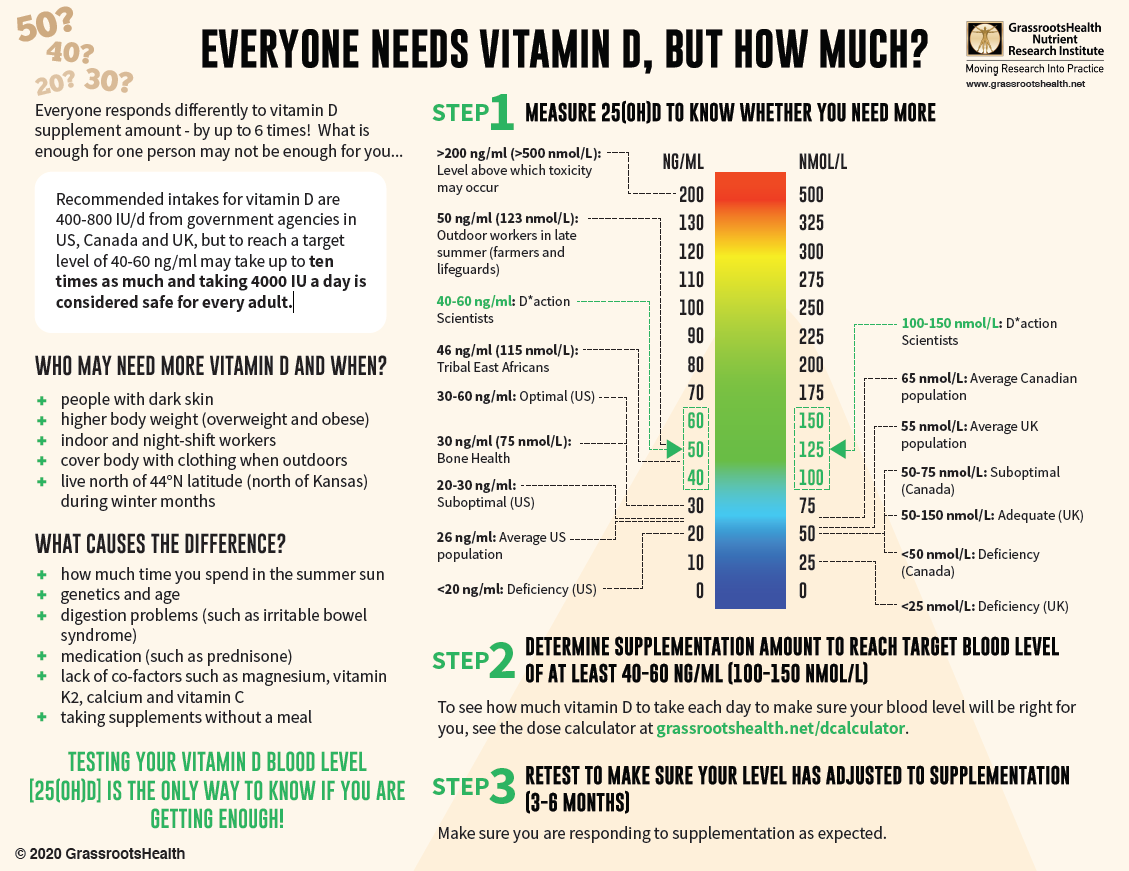
Measuring your vitamin D level is one way to tell if your body is getting enough, and correcting a vitamin D deficiency at any age and any time of life can decrease potential disease severity and improve outcomes. With almost 90% of the general population having vitamin D levels below the recommended 40-60 ng/ml (100-150 nmol/L), it is obvious that most people need more vitamin D. While most of us cannot achieve a vitamin D level of 40-60 ng/ml from sun alone, either due to our lifestyle, where we live, or other circumstances, we can certainly reach those levels with the right amount of supplementation.
Below is a guide for how much you might need, and who may need more. Your levels can be tested safely at home – order your home test kit today.
By joining the GrassrootsHealth projects, you are not only contributing valuable information to our study, but you are also gaining knowledge about how you could improve your own health through measuring and tracking your nutrient status, and educating yourself on how to improve it. Do you know what your status of vitamin D, omega-3s, and other essential nutrients is? Could your levels be improved? Test now to find out!