Published on July 8, 2024
How randomized controlled trials can lead to false conclusions about the effects of vitamin D, and what must happen to prevent it
Key Points
- In the medical science world, data from randomized controlled trials (RCTs) are considered the “gold-standard” evidence, as these types of studies are designed specifically to determine the cause and effect relationship of an intervention (such as a drug) on a primary outcome. Unfortunately, these costly studies can be difficult to optimize and interpret for nutrients, especially vitamin D.
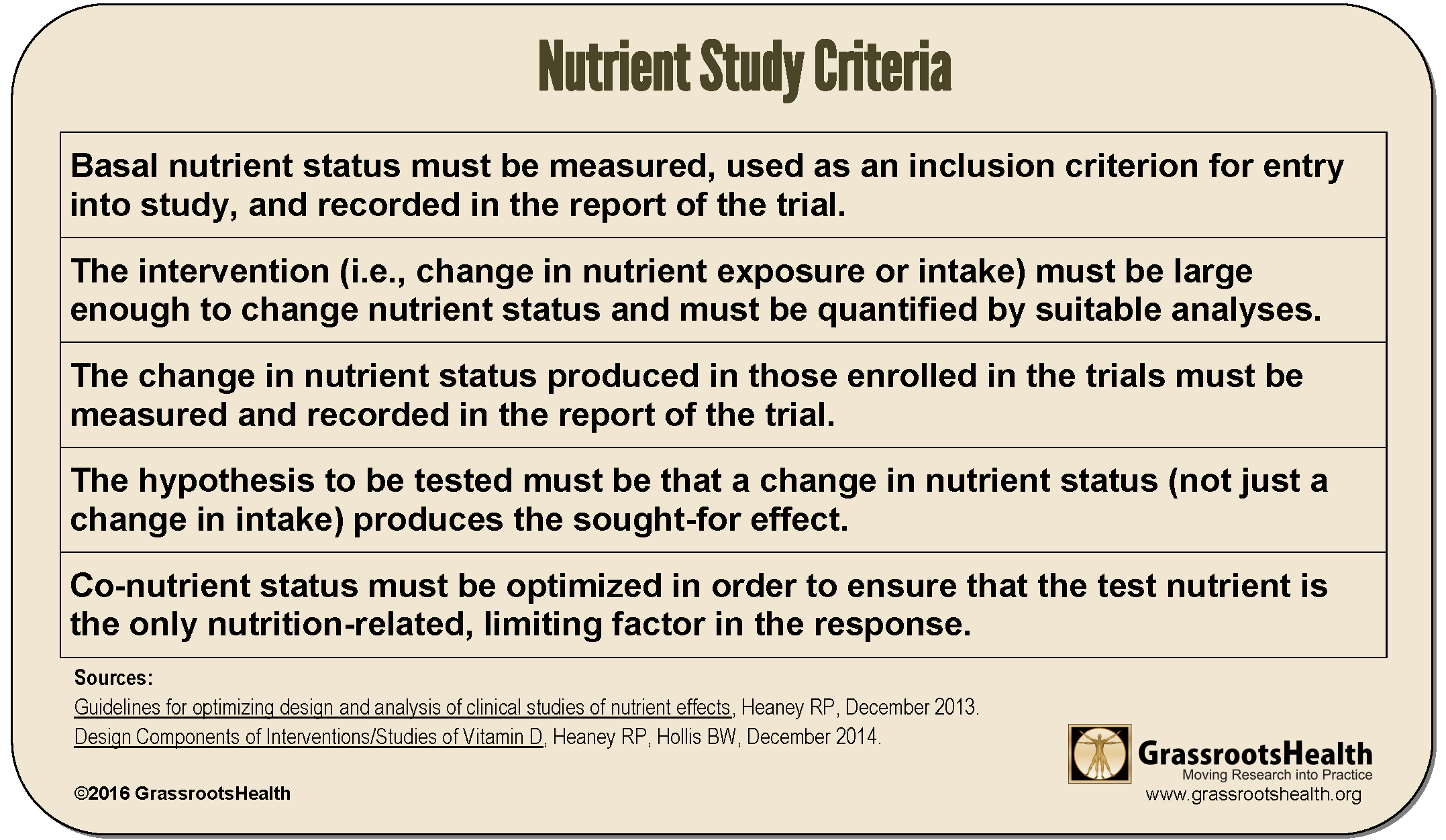
- Dr. Robert Heaney addressed this problem in detail and outlined several important criteria for nutrient study design to follow for the study findings to have the most value
- Before accepting a nutrient research study’s conclusions, it is always important to first evaluate the study to see if it met each of the Heaney Criteria, especially if the study’s results were not what was expected

In the medical science world, randomized controlled trials (RCTs) are considered the “gold-standard” study design to provide solid evidence that “something works.” These types of studies are designed specifically to determine the cause and effect relationship of an intervention on a primary outcome. Unfortunately, while RCTs are efficient ways to evaluate the effects of a drug (something that is not present in the human body unless taken), the RCT design is often not the best-suited study for nutrients.
However, because there has been so much evidence and research (observational studies, etc.) supporting the role of vitamin D in health, researchers took what they thought was the next logical step to further clarify if and how vitamin D did have an effect on certain health outcomes – they designed and executed RCTs for vitamin D.
Conclusion: No obvious overall major health benefits of vitamin D?
A publication by Pilz et al. titled Critical Appraisal of Large Vitamin D Randomized Controlled Trials reviewed some of these large vitamin D RCTs and quotes,
“As none of the (above listed) vitamin D RCTs reported any significant effect on the primary outcomes, it has to be concluded that there are no obvious overall major health benefits of vitamin D supplementation in the setting and in the populations included.”
We know this not to be true!
Human physiology has proven there is a demand for vitamin D within our cells for a multitude of every-day processes. Mechanistic studies have demonstrated how vitamin D works within the cells, tissues, organs, and the body as a whole to directly influence health and the development or regression of many skeletal and non-skeletal diseases. We see the effects of vitamin D demonstrated in observational and epidemiological studies over and over, with disease risk, prevalence, and outcome consistently related to vitamin D levels for many different types of diseases. The fact is that many RCTs of nutrient effects are poorly designed, a reason they can tend to lead to a finding of “no effect,” or a “null” result, when in fact, with a different design, the findings could have told a much different story.
How do we Deal with this Problem in Vitamin D Research?
Dr. Robert Heaney’s Guidelines for optimizing design and analysis of clinical studies of nutrient effects addresses this problem in detail and outlines the following criteria for nutrient studies.
Vitamin D RCTs without these Criteria – Research Waste and Unrealistic Expectations?
These guidelines must be translated into the study design for vitamin D trials. Look closely at the current research to see if they are in place! Without including the criteria in the study design for vitamin D trials, the findings could contribute more to research waste than to something of actual value.
Below are some of the common problems that continue to be implemented in vitamin D research. Taking the following list into consideration, you can see why one might be wary of findings from vitamin D trials designed with these common problems, such as those reviewed by Pilz et al. (which included the VITAL trial, ViDA trial, and Do-Health trial).
Bolus dosing (generally large, intermittent dosing of monthly or longer) – Vitamin D RCTs should give physiological amounts of vitamin D and avoid doses given monthly (or longer), such as those given in the ViDA trial. Vitamin D given on a daily or weekly basis (in the form of vitamin D3) in doses the body can make from the sunshine (not much more than 25,000 – 50,000 IU at any given time) would better match how vitamin D is intended to be ‘received’ in our bodies. It is not possible to make 100,000 IU of vitamin D in a single day, and studies doing so are more likely to have negative findings.
Hypothesis/goal does not mention change in nutrient status – the hypothesis should be that increased vitamin D levels into the therapeutic range will produce the specified effect (less disease, reduced symptoms, etc.), not the dose amount. This premise will often be the core problem; since vitamin D synthesis varies greatly for each person, the hypothesis cannot be by treatment amount (supplement intake) but instead needs to be investigated around achieving a certain serum level.
No initial serum measurement – you can’t measure change if you don’t know the starting value. In fact, baseline vitamin D status should be an inclusion criterion, including only those below the response range (typically <20 ng/ml or <50 nmol/L). This is necessary to be able to “detect” a change in the outcome being measured. If the participants in the study all have high levels to begin with, the signal or change in outcomes is likely to be too small to be detected.
Participants are not deficient (<20 ng/ml) at the start – since an effective study would change nutrient status significantly, the study needs at least one group to start at the low end. Vitamin D RCTs should “target populations who are particularly sensitive to the beneficial effects of the intervention” – for example, enrolling only vitamin D deficient individuals to see what effect correcting the deficiency has on the specific outcomes. Unfortunately, several of the largest vitamin D RCTs recently completed included individuals with “fairly normal” vitamin D levels, such as the VITAL trial. If an individual already has a vitamin D level that is considered optimal for a specific process, giving more will likely not show additional benefit for the effect being considered.
Low dosing (under 2,000 IU/day) – these doses may not move nutrient status significantly for enough of the study participants to observe any effect. Doses should be used to raise vitamin D levels among most treatment group participants into the therapeutic range (40-60 ng/ml or 100-150 nmol/L for many conditions). Often in these trials, the dose of vitamin D given is likely too low to create substantial change in the vitamin D blood level. Both the VITAL and Do-Health trials used only 2000 IU/day without measuring and adjusting dose to ensure a proper vitamin D level was achieved.
Analyzed only by dosage/treatment group, not by serum level – we have seen this mistake made over and over again with trials that associate findings with a dose instead of an achieved vitamin D level. An example of the difference in findings is the Wagner et al. studies on preterm birth, which when re-evaluated by serum level instead of dose, found a much different, positive benefit for vitamin D.
Nutrients such as vitamin D are always present in the human body, so a control group is not feasible, nor is it ethical. Vitamin D can be produced by sun exposure, and can be found in higher amounts in certain foods. Some studies have even not controlled for additional vitamin D supplementation outside of the trial. It is for these reasons that measuring the vitamin D level and evaluating the data based on the level will find much more meaning in vitamin D RCTs than relying only on dose given. As quoted by Pilz et al., “any conclusion that vitamin D supplementation at a given dose is of no health benefit has to refer to the baseline 25(OH)D concentration of the study population and to the achieved vitamin D status after treatment.”
Less than or equal to 6 months testing for chronic conditions and disease prevention – it takes time to change nutrient levels within the body, and for that change to have an effect on disease status. For example, it can take up to 20 years for precancerous cells to develop into detectable cancer. A study that lasts only 3-5 years cannot conclusively determine that vitamin D supplementation does not prevent cancer.
No mention of co-nutrients, no attempt to optimize co-nutrients – this criteria is not a reason to throw out the study, but it would be optimal to optimize co-nutrients.
In Conclusion
As the authors of the Pilz et al. paper state so nicely,
“Overall, future vitamin D research should put more emphasis on a personalized approach. The ‘fire and forget’ concept of recent large vitamin D RCTs with a single vitamin D dose that must fit everyone should be modified for future trial designs… Individual participant baseline and achieved 25(OH)D concentrations should therefore be considered for the design and analysis of RCTs.”
For a better understanding of the ongoing problem with nutrient research, we encourage you to watch the video presentation Nutrition and Medicine: The Troubled Relationship with Dr. Heaney. At around 10:37 he begins to describe why this particular criteria of paying attention to the starting vitamin D serum level is so important for each specific outcome being measured.
Remember, before accepting a nutrient research study’s conclusions, it is always important to first evaluate the study to see if it met each of the Heaney Criteria, especially if the study’s results were not what was expected.
Vitamin D is an Easily Modifiable Factor to Help Improve Disease Outcomes – Are You Getting Enough?
 Having and maintaining healthy vitamin D levels and other nutrient levels can help improve your health now and for your future. Choose which additional nutrients to measure, such as your omega-3s and essential minerals including magnesium and zinc, by creating your custom home test kit today. Take steps to improve the status of each of these measurements to benefit your overall health. You can also track your own intakes, symptoms and results to see what works best for YOU.
Having and maintaining healthy vitamin D levels and other nutrient levels can help improve your health now and for your future. Choose which additional nutrients to measure, such as your omega-3s and essential minerals including magnesium and zinc, by creating your custom home test kit today. Take steps to improve the status of each of these measurements to benefit your overall health. You can also track your own intakes, symptoms and results to see what works best for YOU.
Enroll and test your levels today, learn what steps to take to improve your status of vitamin D (see below) and other nutrients and blood markers, and take action! By enrolling in the GrassrootsHealth projects, you are not only contributing valuable information to everyone, you are also gaining knowledge about how you could improve your own health through measuring and tracking your nutrient status, and educating yourself on how to improve it.