Published on January 10, 2020
Magnesium is an essential nutrient and co-factor for over 600 enzymatic reactions in our body. As an essential co-factor of so many metabolic processes, it is a wonder why nearly half of Americans are deficient in magnesium. It is a mineral naturally present in leafy green vegetables, nuts and seeds, legumes, milk products, and seafood. Magnesium is involved in the absorption and metabolism of essential minerals like calcium and potassium, and is needed for vitamin D activation and glutathione use. Cardiovascular health, bone development, muscle and nerve function, and blood glucose control are all affected by magnesium status.
The Role of Magnesium in Cardiovascular Disease
 Previous posts have highlighted the role of magnesium in cardiovascular health. One study showed how magnesium uses the same pathway as statins to lower LDL cholesterol and raise HDL cholesterol to reduce inflammation, clotting, and plaque formation in the arteries. Another study illustrated how magnesium helps regulate the heartbeat by controlling the sodium potassium pump and extending the relaxation period after contraction, which may help lower the risk of atrial fibrillation, or irregular heartbeat. Adequate intake of magnesium from the diet or supplemental sources is necessary for maintaining cardiovascular health and reducing the risk of cardiac events.
Previous posts have highlighted the role of magnesium in cardiovascular health. One study showed how magnesium uses the same pathway as statins to lower LDL cholesterol and raise HDL cholesterol to reduce inflammation, clotting, and plaque formation in the arteries. Another study illustrated how magnesium helps regulate the heartbeat by controlling the sodium potassium pump and extending the relaxation period after contraction, which may help lower the risk of atrial fibrillation, or irregular heartbeat. Adequate intake of magnesium from the diet or supplemental sources is necessary for maintaining cardiovascular health and reducing the risk of cardiac events.
Is Dietary Magnesium Status Related to Fatal Coronary Heart Disease and Sudden Cardiac Death?
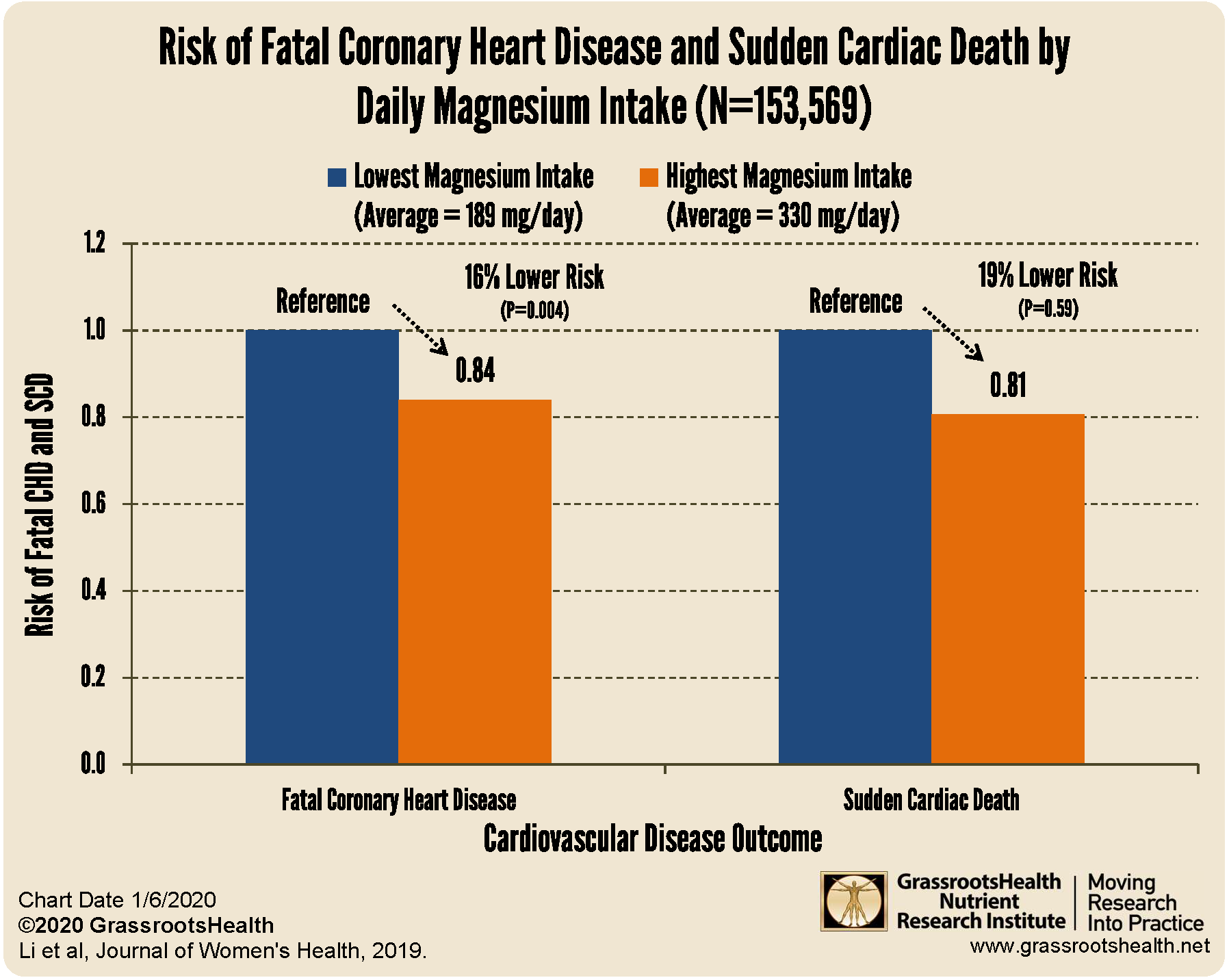
To help answer this question, Li et al. evaluated data from the Women’s Health Initiative, a prospective cohort study. They examined data from a total of 153,569 postmenopausal women ages 50-79 at baseline and calculated their dietary intake of magnesium over the past 3 months using a food-frequency questionnaire. Fatal coronary heart disease (CHD) and sudden cardiac death (SCD) events were recorded over an average follow up time of 10.5 years and analyzed to determine if dietary magnesium intake is a risk factor.
The researchers found that the group with the highest dietary magnesium intake (average = 330 mg/day) had a 16% lower risk of fatal CHD compared to the group with the lowest intake (average = 189 mg/day) adjusted for age, ethnicity, BMI, smoking, and other risk factors (P=0.004). Furthermore, participants with the highest magnesium intake had a 19% lower risk for SCD, but this was not statistically significant (P>0.05).
In conclusion, magnesium appears to have a protective effect against fatal CHD and supports a trend toward lower risk of SCD in postmenopausal women.
Vitamin D, omega-3s, magnesium, and other nutrients are important to measure!
Make sure you know your vitamin D level, and take steps to keep it within a target of 40-60 ng/ml or 100-150 nmol/L! Through GrassrootsHealth Nutrient Research Institute, you can also test your essential elements magnesium, copper, zinc and selenium, toxins such as lead, mercury and cadmium, as well as your omega-3 levels, inflammation levels and thyroid stimulating hormone (TSH) level. Find out your levels today! Log on to the test selection page (click the link below) to get your tests and see for yourself if your levels can be improved.
Make sure you track your results before and after, about every 6 months!
How can I track my nutrient intake and levels over time?
To help you track your supplement use and nutrient levels, GrassrootsHealth has created an online tracking system called myData-myAnswers. For each specific supplement, you can track what days you take it, how much, and many other details. This will help you know your true supplemental intake and what patterns of use work for you to reach and maintain optimum nutrient levels. Check it out today!