Published on March 21, 2022
70% or more of all infants are not getting the recommended amounts of vitamin D, despite recommendations from the American Academy of Pediatrics
Key Points
- Studies have found no increase in the percent of infants achieving the recommended 400 IU/day intake of vitamin D since the American Academy of Pediatrics revised their guidelines; in fact, only 27% of all infants met the guidelines, with breastfeeding infants being less likely to meet the guidelines than non-breastfeeding infants
- Previous research has found that if a breastfeeding mother was only taking the recommended daily allowance of vitamin D per day, then an infant, solely fed on breast milk, would get the equivalent of 33 – 68 IU vitamin D / liter, which would provide the infant with far less than the recommended 400 IU/day, typically resulting in vitamin D levels less than 5 ng/ml
- RCTs have concluded that giving breastfeeding mothers 6,400 IU vitamin D /day, and no additional supplement for the infant, made sure the mother became sufficient (with an average vitamin D level of around 60 ng/ml) AND infants became sufficient (with an average vitamin D level a little above 40 ng/ml)
 In 2009, the American Academy of Pediatrics (AAP) doubled their recommendation for vitamin D intake among infants and children to 400 IU per day, stressing the importance of beginning supplementation within the first few days of life. Even with this recommendation given to all pediatricians in the United States, studies show a compliance rate of between 2 – 19%. Dr. Bruce Hollis, a vitamin D researcher with multiple publications on pediatric health, calls this “a largely failed initiative.”
In 2009, the American Academy of Pediatrics (AAP) doubled their recommendation for vitamin D intake among infants and children to 400 IU per day, stressing the importance of beginning supplementation within the first few days of life. Even with this recommendation given to all pediatricians in the United States, studies show a compliance rate of between 2 – 19%. Dr. Bruce Hollis, a vitamin D researcher with multiple publications on pediatric health, calls this “a largely failed initiative.”
Current Statistics Show Failure to Improve Despite Updated Recommendations
A 2020 review published by Simon and Ahrens looked at NHANES vitamin D intake amounts among US infants for the years 2009 – 2016. NHANES is the National Health and Nutrition Examination Survey, a program run by the Centers for Disease Control (CDC) to assess health and nutrition status of Americans. The authors found no increase in the percent of infants achieving the recommended vitamin D intake since the American Academy of Pediatrics revised their guidelines. In fact, only 27% of all infants met vitamin D intake guidelines, with breastfeeding infants being less likely to meet the guidelines than non-breastfeeding infants. In other words, 70% or more of all infants are not getting the recommended amounts of vitamin D!
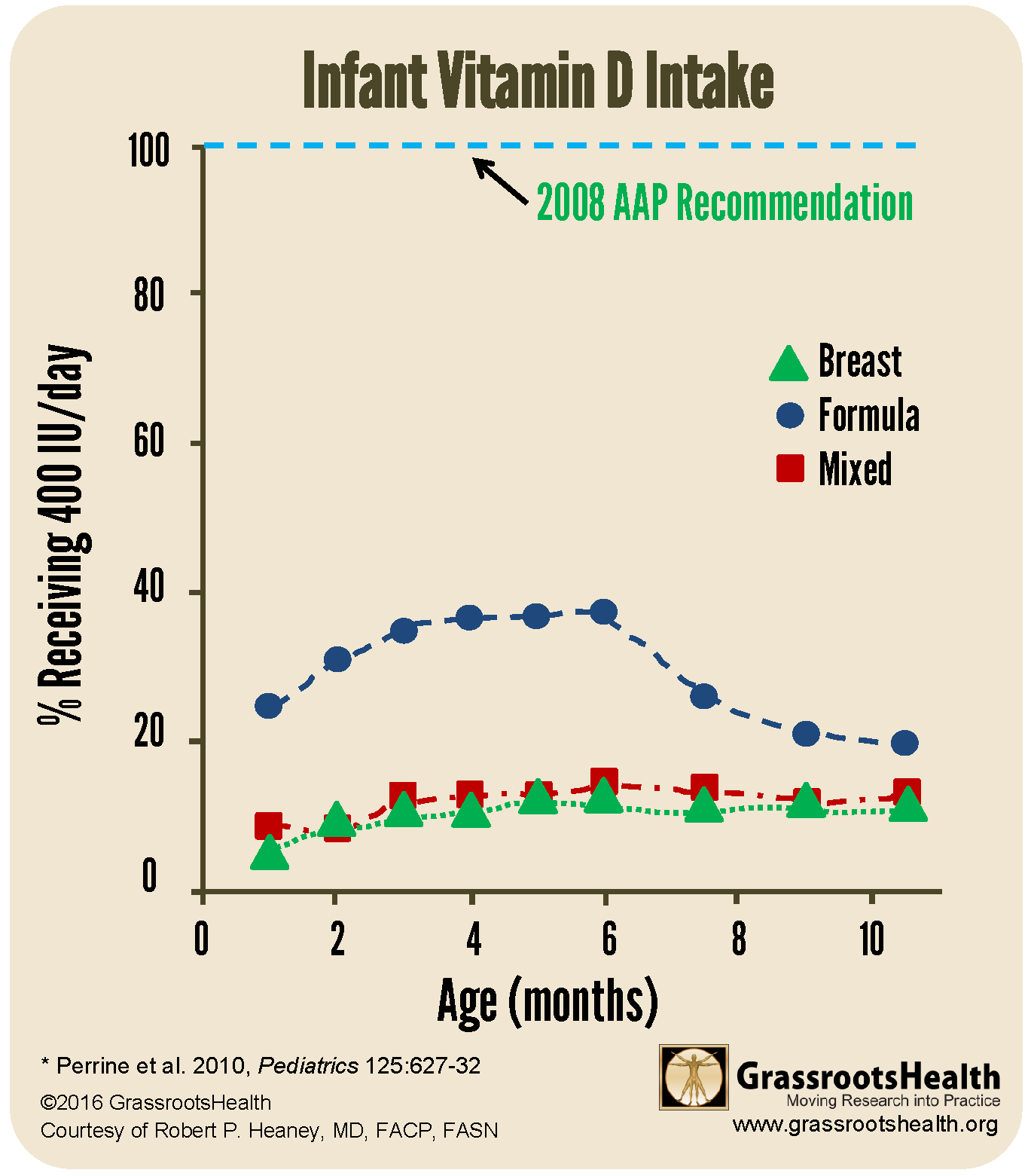
To illustrate the severity of the issue, below is a chart of NHANES data (2009-2012) from the paper, Adherence to Vitamin D Recommendations Among US Infants Aged 0 to 11 Months, NHANES, 2009 to 2012. As can be seen, at best, approximately 40% of formula fed infants and approximately 15% of breast fed and mixed fed infants receive the minimum recommended vitamin D intake on a day to day basis.
Is Breastmilk Broken? How do we get babies the vitamin D they need?
Should the recommendations be for infants to receive vitamin D supplementation? If breastfeeding is nature’s method for feeding babies, has it always been so flawed? Could the problem be that most mothers are lacking in their own vitamin D intake?
WHAT’S KNOWN ON THIS SUBJECT: The vitamin D concentration in breast milk of women taking 400 IU vitamin D per day is relatively low, leading to vitamin D deficiency in breastfeeding infants. As a result, the American Academy of Pediatrics recommends breastfeeding infants supplement with vitamin D within days after birth.
Previous research has found that if a breastfeeding mother was only taking the recommended daily allowance of vitamin D per day, then an infant, solely fed on breast milk, would get the equivalent of 33 – 68 IU vitamin D / liter, which would provide the infant with far less than the recommended 400 IU/day, typically resulting in vitamin D levels less than 5 ng/ml (< 12.5 nmol/L).
A randomized controlled trial (RCT) by Hollis et al. divided the breastfeeding women/infant pairs, at 4-6 weeks post-partum, into one of three groups:
1. Mother takes 400 IU/day vitamin D (placebo and prenatal vitamin with 400 IU), infant supplements with 400 IU/day vitamin D (1 drop liquid suspension).
2. Mother takes 2400 IU/day vitamin D (2000 IU and prenatal), infant takes no vitamin D supplementation (placebo liquid drop). (This group was canceled about 4 years into the study due to an increase in infant vitamin D deficiency (defined as 25(OH)D < 20 ng/ml)).
3. Mother takes 6400 IU/day vitamin D (6000 IU and prenatal), the infant takes no vitamin D supplementation (placebo liquid drop).
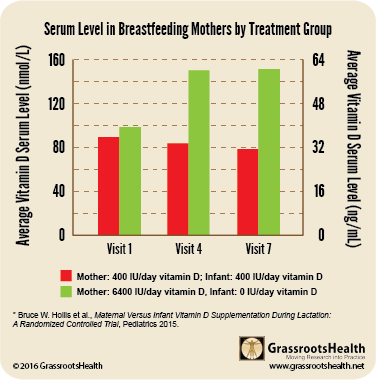
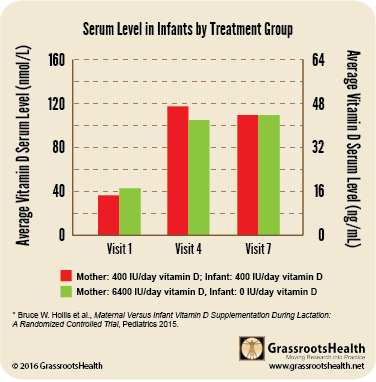
WHAT THIS STUDY FOUND: Maternal vitamin D supplementation alone with 6400 IU/day safely supplies breast milk with adequate vitamin D to satisfy the requirement of her nursing infant and offers an alternate strategy to direct infant supplementation (see charts below)
Summary
The RCT concluded that giving breastfeeding mothers 6,400 IU vitamin D /day, and no additional supplement for the infant, made sure the mother became sufficient (with an average vitamin D level of around 60 ng/ml) AND infants became sufficient (with an average vitamin D level a little above 40 ng/ml). The infants in this group had equivalent vitamin D status to those who received 400 IU/day (and the mother also received 400 IU/day). Many other measurements and blood tests were taken, including weight, length and head circumference of the infant, which were similar for both groups.
6400 IU vit D/day for mom = Sufficient mom AND baby
Daily intake is most important
One of the most important takeaway messages from this research is that breast milk can be an adequate source of vitamin D for the infant if the mother takes enough of a supplement daily! (Adequate daily sun exposure would also have the same result, but that was not part of this research study.)
In earlier research, Hollis analyzed how vitamin D is transferred from the mother to the baby and found that it is transferred primarily in its parent form as vitamin D3 rather than 25(OH)D, the compound that is most commonly measured in blood. Vitamin D3 has a half-life of approximately 12 – 24 hours, and thus has to be replenished daily; 25(OH)D has a half-life of approximately 3 weeks, so while intermittent dosing can maintain high levels of 25(OH)D, it will not be adequate for transferring the daily requirement of vitamin D3 to the breastmilk.
A Better Recommendation for Infants, and Mothers!
In conclusion, Hollis recommends the standard of care for breastfeeding mothers to be 6,400 IU vitamin D per day. This is safe and effective and ensures both mother and baby will be able to achieve recommended levels of vitamin D of 40-60 ng/ml (100-150 nmol/L).
Make Sure You Are Getting Enough Vitamin D
 Having and maintaining healthy vitamin D levels and other nutrient levels can help improve your health now and for your future. Choose which additional nutrients to measure, such as your omega-3s and essential minerals including magnesium and zinc, by creating your custom home test kit today. Take steps to improve the status of each of these measurements to benefit your overall health. With measurement you can then determine how much is needed and steps to achieve your goals. You can also track your own intakes, symptoms and results to see what works best for YOU.
Having and maintaining healthy vitamin D levels and other nutrient levels can help improve your health now and for your future. Choose which additional nutrients to measure, such as your omega-3s and essential minerals including magnesium and zinc, by creating your custom home test kit today. Take steps to improve the status of each of these measurements to benefit your overall health. With measurement you can then determine how much is needed and steps to achieve your goals. You can also track your own intakes, symptoms and results to see what works best for YOU.
Enroll in D*action and Test Your Levels Today!





