Published on March 1, 2024
How vitamin D, magnesium, and sunshine exposure can affect colorectal cancer incidence and outcomes. Learn and share this information as part of Colorectal Cancer Awareness Month!
Key Points
- Vitamin D has many cancer-fighting functions within the body, and evidence associating vitamin D and cancer is so strong that vitamin D is now thought to be a causal factor in the risk-reduction of most types of cancer.
- A GrassrootsHealth study found that women with a mean vitamin D level of at least 40 ng/ml (100 nmol/L) had a 71% lower risk of all invasive cancers combined, excluding skin cancer, compared to women with levels below 20 ng/ml (<50 nmol/L)
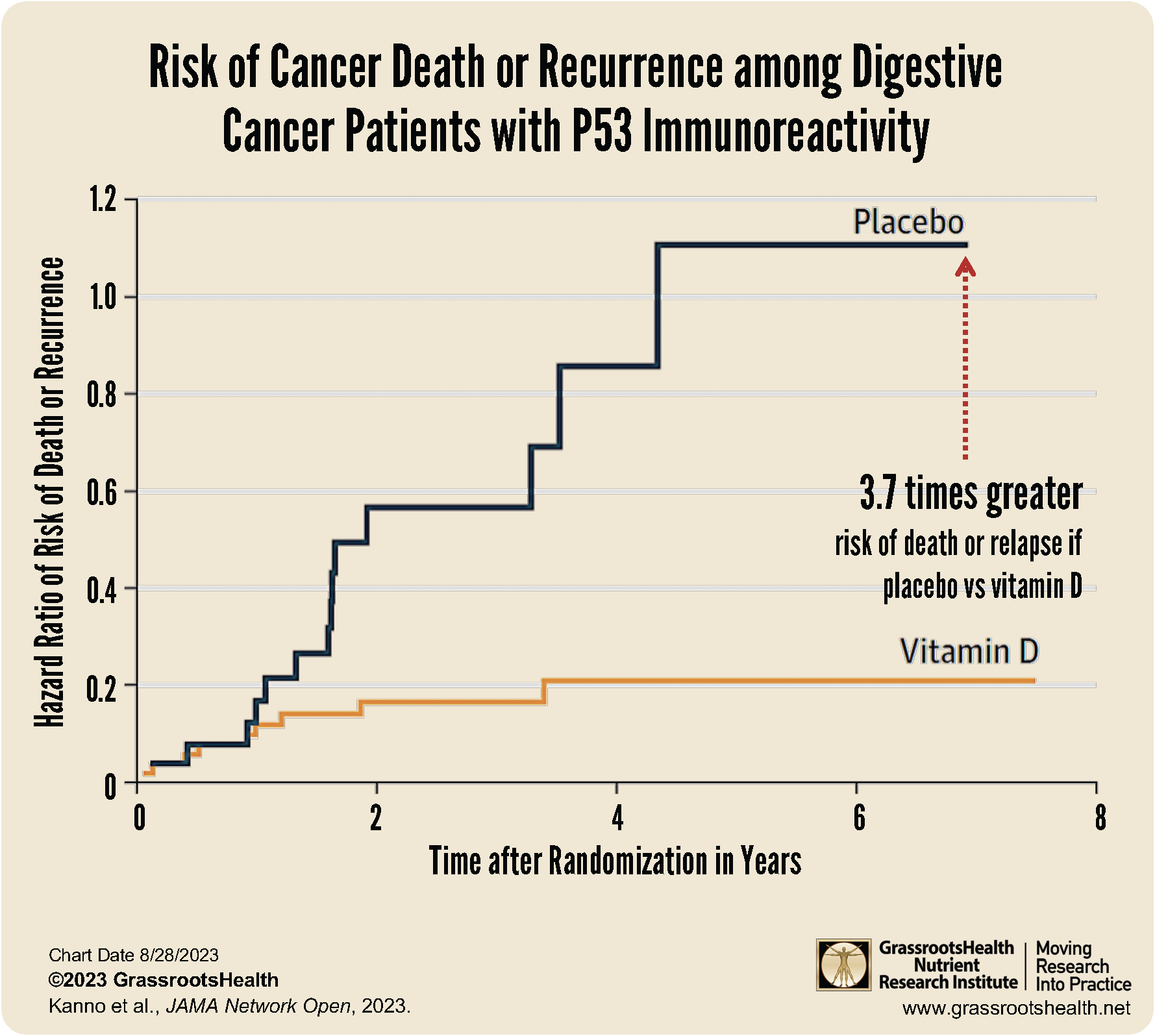
- A 2023 study by Kanno et al. found that vitamin D supplementation improved the chances of survival by more than 2.5 fold among individuals with digestive cancers who were p53-immunoreactive, compared to those not taking vitamin D – a finding that “now proves beyond a doubt the power of vitamin D against cancer recurrence and fatality at the clinical level”
- Several additional studies have shown a significant relationship between vitamin D and the risk of disease progression and death among colorectal cancer patients
Colorectal cancer is a combined term to include cancer of the colon and cancer of the rectum. As the fourth most common cancer world-wide, colorectal cancer affects millions of lives each year, and in the US, is the second leading cause of cancer death.
Colorectal Cancer Statistics
Men are more likely to have colorectal cancer than women. Using US data from 2016-2020 (the most recent available), there were 42.1 new cases each year for every 100,000 men and 32.0 new cases for every 100,000 women.
The median age at the time of diagnosis is 66 years, and a quarter (25.5%) of new cases are diagnosed in those who are between the ages of 65 – 74; 22.8% of new cases are in people aged 55 – 64; and 19.0% in those aged 75 – 84.
How Does Vitamin D Help Fight Cancer?
Vitamin D has many anti-cancer functions, including:
- Inhibits cancer cell growth and proliferation
- Reduces cancer metastasis
- Stimulates maturation of healthy cells (differentiation)
- Induces death of cancer cells (apoptosis or programmed cell death)
- Prevents blood vessel growth in tumors (angiogenesis)
- Prevents inflammation associated with cancer
- Reduces the risk of incidence and/or death due to cancer
Could Vitamin D be a Causal Factor in Cancer Risk?
A 2016 GrassrootsHealth analysis on vitamin D levels among older women (ages 55 years and up) and cancer incidence found that women with a mean vitamin D serum level greater than or equal to 40 ng/ml (100 nmol/L) had a 71% lower risk of cancer than women with serum levels <20 ng/ml (<50 nmol/L; P-value = .02). This was for cancer incidence over a median of 3.9 years for all invasive cancers combined, excluding skin cancer. More details on how vitamin D fights cancer can be found in this post, Anticancer Effects of Vitamin D. You can also download, print and share our Cancer Prevention with Vitamin D brochure here.
The evidence associating vitamin D and cancer is so strong that vitamin D is now thought to be a causal factor in the risk-reduction of most types of cancer. Causation can be determined using a set of scientific guidelines called Hill’s criteria for causality, which looks at data based on the strength of association, consistency between studies, temporality, biological gradient, plausibility, coherence with known scientific facts, experiment, and analogy. Two separate publications (WB Grant and Mohr et al.) have confirmed vitamin D as a causal risk-modifying factor for most cancers using Hill’s criteria.
Vitamin D Improved Survival of Digestive Cancers by More than 2.5 Fold
A new 2023 study found that vitamin D supplementation improved the chances of survival by more than 2.5 fold among individuals with digestive cancers who were p53-immunoreactive, compared to those not taking vitamin D. The post hoc analysis was performed on data from a randomized clinical trial involving patients with stage 1 to stage 3 digestive tract cancers. There were 260 men and 132 women with a mean age of 66 years old. A subgroup of patients was identified as p53-immunoreactive; p53 is a tumor suppressor protein present only in small concentrations in normal cells that when mutated becomes an oncogene (promotes cancer). The mutated p53 oncogene is over-expressed in 40-50% of digestive system cancers, often triggering an immune response against the cancerous cells that destroys them.
Data from the p53 immunoreactive patients was analyzed, including 54 patients who had received 2,000 IU vitamin D3 supplementation daily and 26 who received placebo. Those getting vitamin D experienced a significantly higher chance of 5-year relapse-free survival compared to those receiving a placebo; specifically, those getting the placebo had a 3.7 times greater risk of death or relapse compared to those receiving vitamin D3. Read more about these findings here.
What Does the Research Say About Vitamin D and Colorectal Cancer?
A meta-analysis is a statistical analysis that combines the results of multiple studies that have investigated the same question. The meta-analysis can be a powerful tool when studies have had conflicting results and when examining diseases that have low rates.
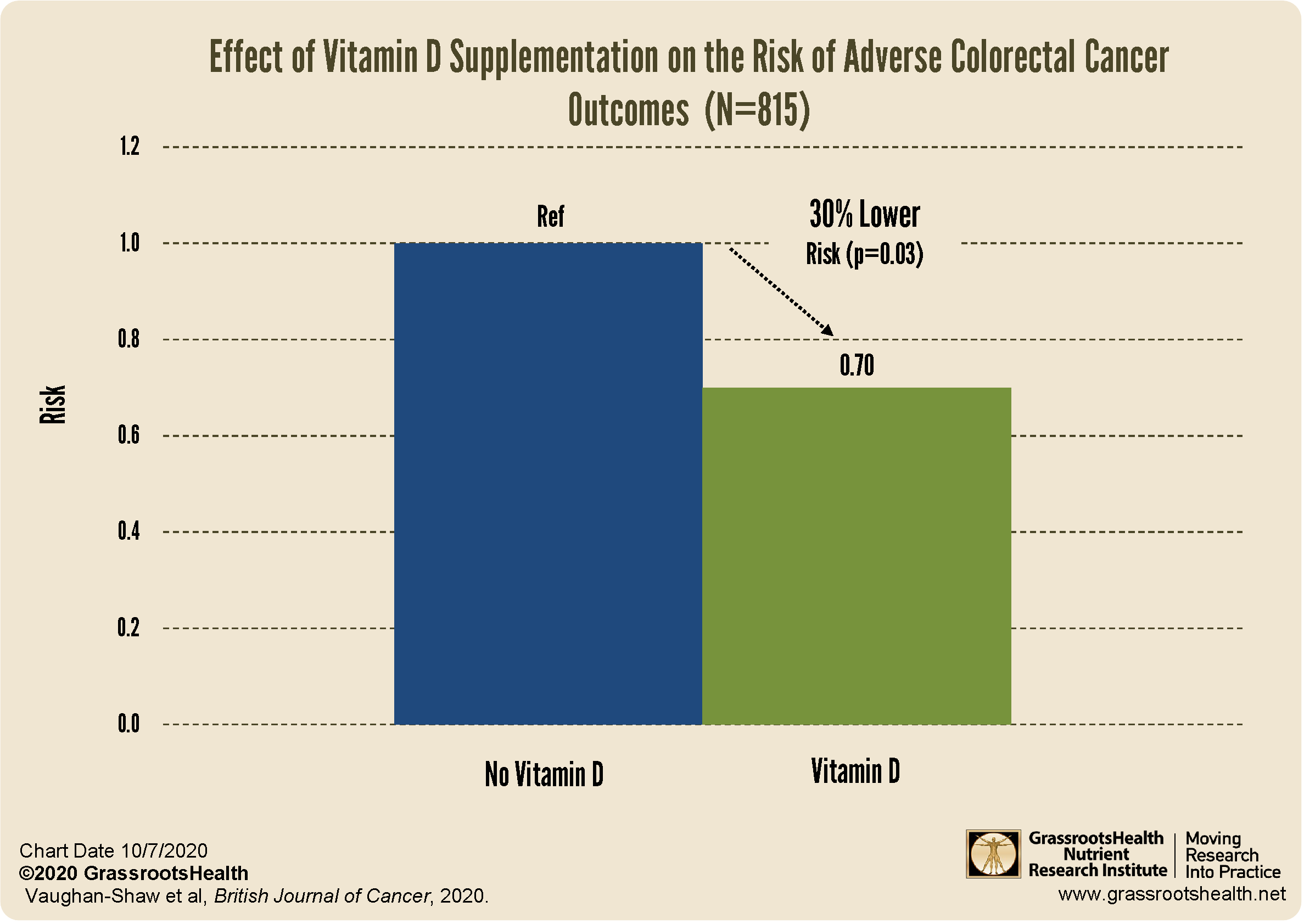
A meta-analysis on colorectal cancer and vitamin D by Vaughan-Shaw et al. looked at data from 7 randomized controlled trials (RCTs), 3 RCTs that included colorectal cancer patients at enrollment, and 4 RCTs that reported on new colorectal cancer cases that occurred during the study. Their goal was to determine the effect of vitamin D supplementation on colorectal cancer survival rates. They found that all trials included in the review showed a beneficial effect of vitamin D supplementation on colorectal cancer outcomes, with an overall 30% reduction in adverse outcomes (worsening or death) from colorectal cancer among those who supplemented with vitamin D. While this is a compelling result, many of the trials included in the meta-analysis provided doses of vitamin D that were too low to achieve the target vitamin D blood levels recommended by GrassrootsHealth scientists (40-60 ng/mL) and did not measure vitamin D levels (the majority of trial doses ranged from 2,000 to 4,000 IU/d). Analysis by vitamin D level may have resulted in an even greater risk reduction results.
(Vaughan-Shaw et al., 2020 Meta-analysis)
The authors of this study concluded,
“this meta-analysis demonstrates a clinically meaningful beneficial effect from vitamin D supplementation on survival outcomes in patients with CRC.”
Additional Research on Vitamin D and Colorectal Cancer
Additional research on vitamin D and colorectal cancer specifically has shown a
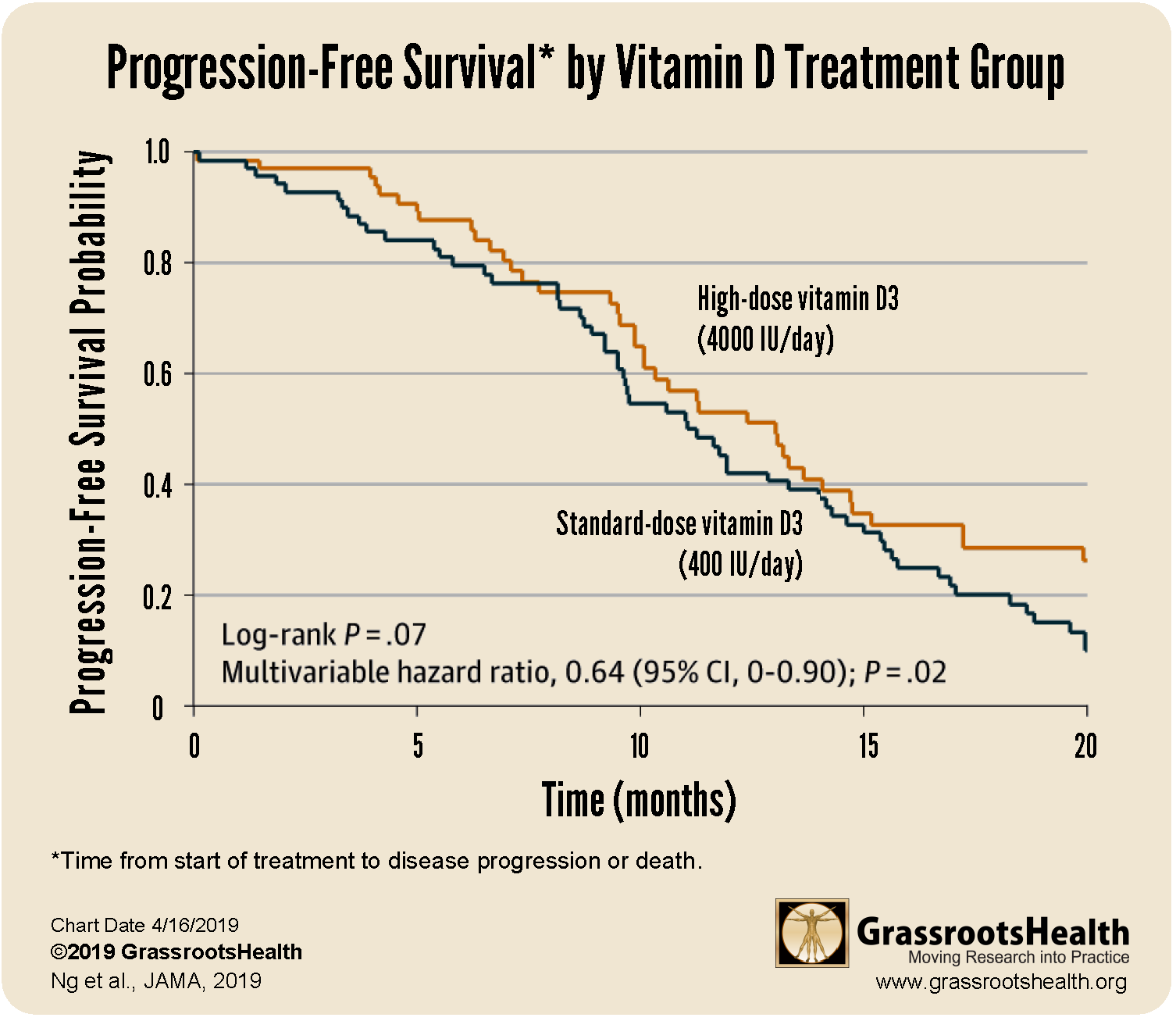
36% Lower Risk of Disease Progression or Death among those taking a higher dose of vitamin D [8,000 IU/day of vitamin D for 14 days then 4,000 IU/day, average vitamin D level of 35 ng/ml (87 nmol/L)] than those in the lower dose group [400 IU/day, average vitamin D level 19 ng/ml (47 nmol/L)]
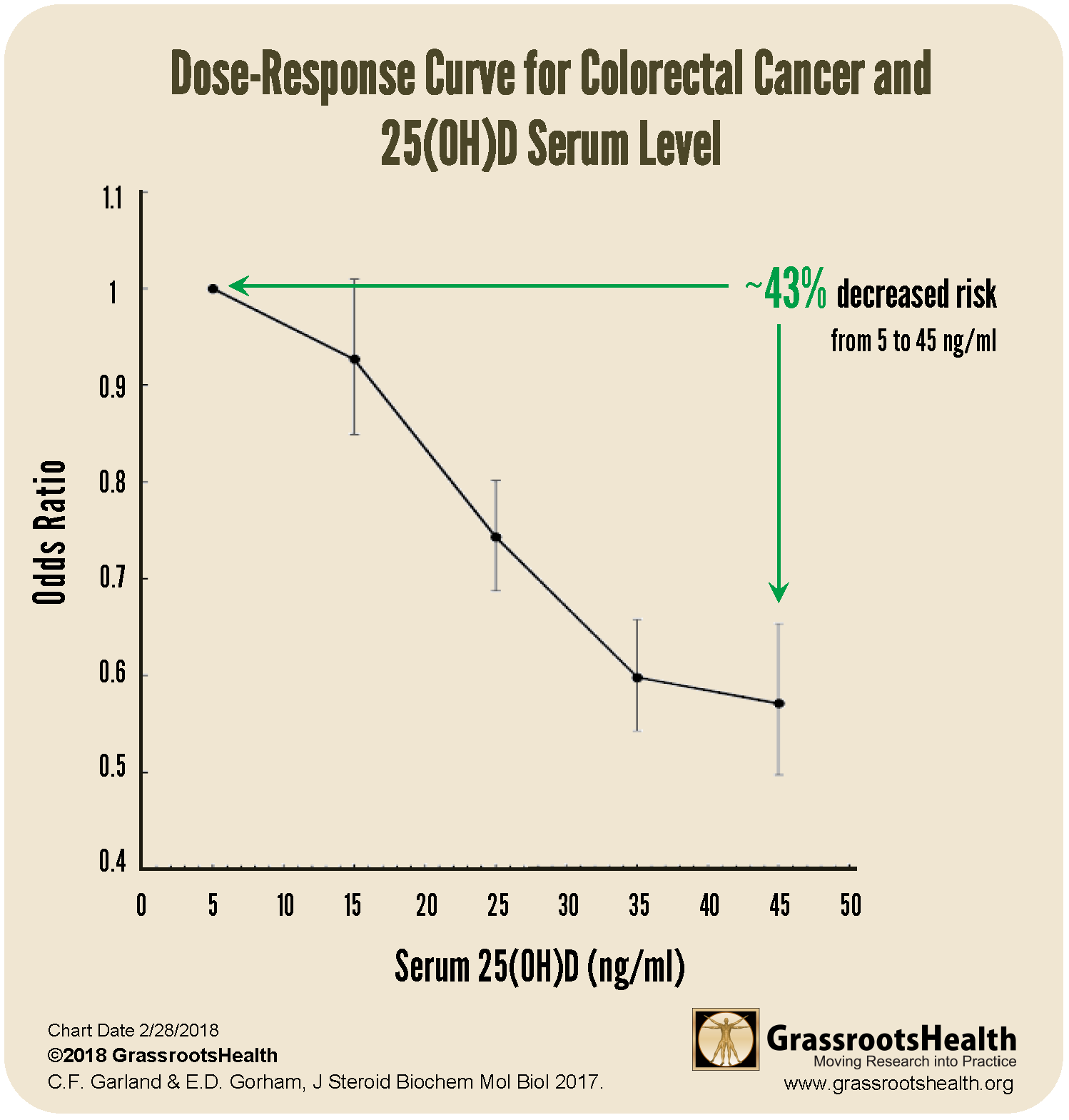
43% Decreased Risk of Colorectal Cancer with a higher vitamin D level [45 ng/ml vs 5 ng/ml (112 nmol/L vs 13 nmol/L)]
(Garland & Gorham, 2017 meta-analysis)
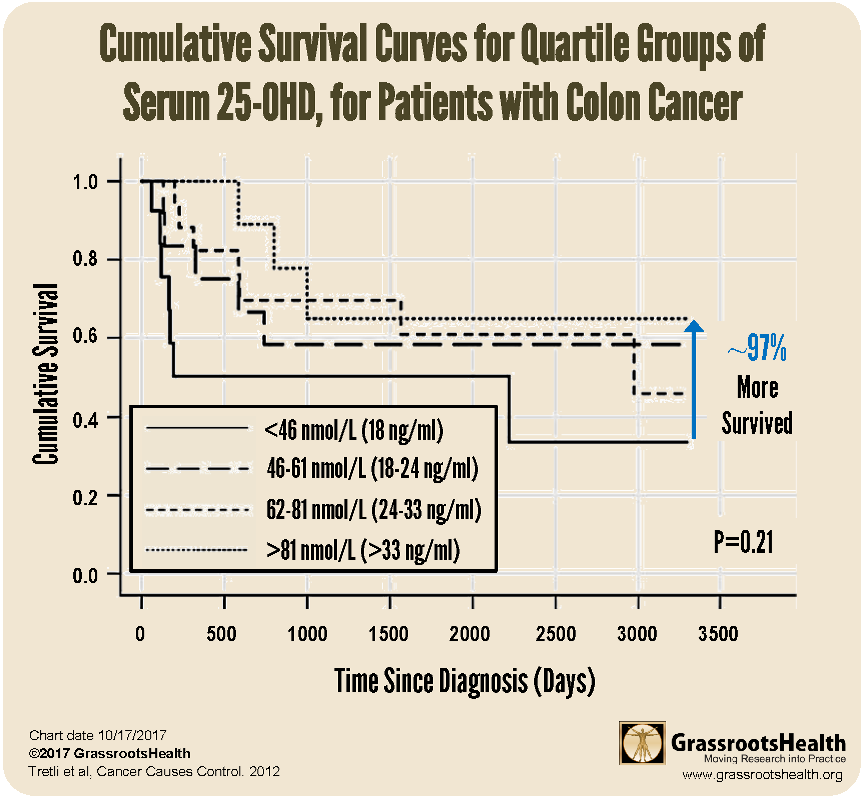
97% More Colorectal Cancer Patients Survived when their vitamin D level was at least 33 ng/ml (81 nmol/L) compared to less than 18 ng/ml (46 nmol/L)
Colorectal Cancer Risk Decreases with Increased Magnesium
Magnesium is an important co-nutrient for vitamin D! Unfortunately, at least half of us do not get enough magnesium on a daily basis which may lead to health effects ranging from fatigue and loss of appetite, to tremors and muscle cramps.
A study by Gorczyca et al. involving 140,601 postmenopausal women found an inverse association between the risk of colorectal cancer and magnesium intake (from both diet and supplements), with a 21% decreased risk between women with the highest magnesium intake compared to the lowest. The greatest decreased risk was seen among women whose total daily magnesium intake was greater than 400 mg/day.
More Sunshine Also Linked to Less Colorectal Cancer
Both inadequate sun exposure and low vitamin D levels have been linked to higher colorectal cancer incidence. A study by Valles et al. found a 19% lower risk of colorectal cancer for participants who reported sun exposure of 2 or more hours per day compared to 1-2 hours per day. Upon additional analysis, they found both independent and cooperative effects of sun exposure and dietary vitamin D plus calcium on lower colorectal cancer risk, indicating that sun exposure and dietary vitamin D, both separately and together, could reduce colorectal cancer risk and be key to cancer prevention.
Do You Need More Vitamin D or Other Important Nutrients? Find Out with Your Home Test!
 Having and maintaining healthy vitamin D levels and other nutrient levels can help improve your health now and for your future. Choose which additional nutrients to measure, such as your omega-3s and essential minerals including magnesium and zinc, by creating your custom home test kit today. Take steps to improve the status of each of these measurements to benefit your overall health. With measurement you can then determine how much is needed and steps to achieve your goals. You can also track your own intakes, symptoms and results to see what works best for YOU.
Having and maintaining healthy vitamin D levels and other nutrient levels can help improve your health now and for your future. Choose which additional nutrients to measure, such as your omega-3s and essential minerals including magnesium and zinc, by creating your custom home test kit today. Take steps to improve the status of each of these measurements to benefit your overall health. With measurement you can then determine how much is needed and steps to achieve your goals. You can also track your own intakes, symptoms and results to see what works best for YOU.
Enroll in D*action and Test Your Levels Today!