Published on February 21, 2023
With the many reports on the VITAL Randomized Controlled Trial of vitamin D and omega-3s, here are some initial findings on heart disease, cancer and death that did not make major headlines
Key Points
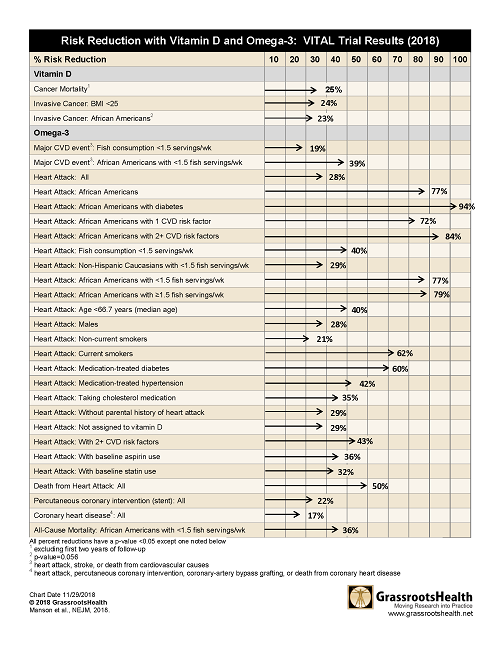
- Based on initial results publications from the VITAL trial, you may have heard that the study showed that neither vitamin D nor omega-3s prevent cancer (all kinds of cancer analyzed together) or heart disease (a composite of all types); however, when the separate types of heart disease or death from cancer were analyzed, there were 30 different very significant results
- Additional findings from VITAL have included a significant reduction of metastatic or fatal cancer was seen among those with a normal BMI, with a decreased risk of 38% among those taking vitamin D compared to placebo, and a 22% reduction in the incidence of autoimmune disease among the participants taking vitamin D
- Given the significant positive effects of vitamin D on cancer death and omega-3s on cardiovascular health found in the VITAL trial (which is supported by many other studies), and the fact that these supplements are safe and inexpensive, daily supplementation is beneficial; due to the wide variability in dose response among individuals for both of these nutrients, testing vitamin D and omega-3 levels is the only way to tell if one is getting enough
 What choices would you make about your omega-3 and vitamin D intake given the following results which showed
What choices would you make about your omega-3 and vitamin D intake given the following results which showed
- 50% reduction in death from heart attack for all
- 77% reduction in heart attack for African Americans
- 25% reduction in risk of cancer mortality
- ….many others, see below
Overview of the VITAL Trial
The VITAL trial, which was primarily focused on cancer and cardiovascular health, was a recent, randomized, double blind, placebo-controlled clinical trial conducted in multiple centers around the United States. It included 25,871 participants who were free of cancer and cardiovascular disease diagnoses at baseline. Participants were either male, ages 50 years and older, or female, ages 55 years and older. Participants were given 2000 IU vitamin D per day and 1 gram of marine omega-3 fatty acids per day, or placebo.
The VITAL trial has published several papers since its conclusion, including two initial papers: one paper comparing those assigned to vitamin D (2000 IU/day) vs. placebo and another paper comparing those assigned to omega-3s (1000 mg/day) vs. placebo. Based on these initial publications, you may have heard that this study showed that neither vitamin D nor omega-3s prevent cancer (all kinds of cancer analyzed together) or heart disease (a composite of all types).
However, when the separate types of heart disease or death from cancer were analyzed, there were 30 different very significant results. See the tables below or download, print and share here.
Statistically Significant Vitamin D Results from Pre-specified Secondary Outcomes and Subgroup Analyses
|
Vitamin D vs. Placebo
|
|
|
Secondary Outcomes
|
|
|
Cancer Mortality
(excluding first two years of follow-up)
|
25% reduced risk (p=0.02)
|
|
Primary Outcomes – Subgroup Analyses
|
|
|
Invasive Cancer
|
|
|
BMI<25
|
24% reduced risk (p=0.003) |
|
African Americans
|
23% reduced risk (p=0.056*) |
Statistically Significant Omega-3 Results from Pre-specified Secondary Outcomes and Subgroup Analyses
|
Omega-3 vs. Placebo
|
|
|
Secondary Outcomes
|
|
|
Heart Attack
|
28% reduced risk (p=0.002)
|
|
Primary Outcomes – Subgroup Analyses
|
|
|
Major CVD event
(heart attack, stroke, or death from cardiovascular cause)
|
|
|
Fish consumption <1.5 servings/wk
|
19% reduced risk (p=0.03)
|
|
African Americans with <1.5 servings of fish/wk
|
39% reduced risk (p=0.049)
|
|
Secondary Outcomes – Subgroup Analyses
|
|
|
Heart Attack
|
|
|
African Americans
|
77% reduced risk (p=<0.0001)
|
|
African Americans with diabetes
|
94% reduced risk (p=0.005)
|
|
African Americans with 1 cardiovascular risk factor
|
72% reduced risk (p=0.047)
|
|
African Americans with 2+ cardiovascular risk factors
|
84% reduced risk (p=0.001)
|
|
Fish consumption <1.5 servings/wk
|
40% reduced risk (p=0.0007)
|
|
Non-Hispanic Caucasians with <1.5 servings of fish/wk
|
29% reduced risk (p=0.04)
|
|
African Americans with <1.5 servings of fish/wk
|
77% reduced risk (p=0.003)
|
|
African Americans with ≥1.5 servings of fish/wk
|
79% reduced risk (p=0.01)
|
|
Age <66.7 years (median age)
|
40% reduced risk (p=0.005)
|
|
Males
|
28% reduced risk (p=0.02)
|
|
Non-current Smokers
|
21% reduced risk (p=0.04)
|
|
Current Smokers
|
62% reduced risk (p=0.02)
|
|
Medication-treated diabetes
|
60% reduced risk (p=0.0003)
|
|
Medication-treated hypertension
|
42% reduced risk (p=0.0002)
|
|
Taking cholesterol medication
|
35% reduced risk (p=0.02)
|
|
Without parental history of heart attack
|
29% reduced risk (p=0.008)
|
|
Not assigned to vitamin D
|
29% reduced risk (p=0.02)
|
|
With 2+ cardiovascular risk factors
|
43% reduced risk (p=0.001)
|
|
With baseline aspirin use
|
36% reduced risk (p=0.007)
|
|
With baseline statin use
|
32% reduced risk (p=0.04)
|
|
All-Cause Mortality
|
|
|
African Americans with <1.5 servings of fish/wk
|
36% reduced risk (p=0.03)
|
Statistically Significant Omega-3 Results from Post-Hoc Outcomes
|
Omega-3 vs. Placebo
|
|
|
Post-Hoc Outcomes
|
|
|
Death from Heart Attack
|
50% reduced risk (p=0.04)
|
|
Percutaneous coronary intervention (PCI; stent)
|
22% reduced risk (p=0.02)
|
|
Coronary heart disease (heart attack, PCI, CVD death)
|
17% reduced risk (p=0.02)
|
A printable version of these results can be downloaded here.
What Are Secondary and Post-Hoc Outcomes?
Most clinical trials examine many outcomes during the course of a study. During the design phase of the study, primary and secondary outcomes are specified along with specific sub-group analyses. The primary outcome is considered the most important measure to evaluate the effect of a particular intervention (this choice is made by the scientists). The primary outcome is used as a guide to determine how many people to enroll in the study and how long it should last.
Secondary outcomes are measures that are of interest, and may support the primary outcome, but because the trial was not designed for these outcomes there may not be the same certainty in results as the primary outcome. Pre-specifying outcomes reduces the risk of finding false-positive results because the more outcomes you test, the more likely you are to find a significant result by chance alone.
Researchers can also publish results on outcomes that were not pre-specified (i.e. post hoc), but these results are considered preliminary because they are typically added once a pattern has been discovered in the data and therefore have a higher false-positive risk. The VITAL trial reported a few statistically significant post hoc tests for those assigned to omega-3 vs. those assigned to placebo.
Additional Findings from VITAL
In these initial findings, the effects from vitamin D were not as prolific as those from omega-3’s likely due to the relatively low dose of vitamin D given (2000 IU/day). To get to a vitamin D serum level of 40 ng/ml (100 nmol/L), our scientists’ panel’s recommendation, it would take 5000 IU/day to get approximately 82% of the population to that level. Also, the data from this study were not analyzed by serum level in these initial papers, so the results of higher and lower levels would be averaged and miss the educational point of the serum level significance. Read more about this and other important criteria that all nutrient studies should follow, and whether the VITAL trial design met those criteria.
Additional findings from VITAL have been published since those included in the first two papers. For example, when taking BMI into consideration the reduction in cancer was more pronounced for those taking vitamin D. A significant reduction of metastatic or fatal cancer was seen among those with a normal BMI, with a decreased risk of 38% among those taking vitamin D compared to placebo (p=0.004); the findings were non-significant among those who were overweight or obese. In other words, the greatest risk reduction was seen among those with the lowest BMI.
Another meaningful and statistically significant finding was a 22% reduction in the incidence of autoimmune disease among the participants taking vitamin D.
Getting Enough Vitamin D and Omega-3s
Given the significant positive effects of vitamin D on cancer death and omega-3s on cardiovascular health found in the VITAL trial (which is supported by many other studies), and the fact that these supplements are safe and inexpensive, daily supplementation is beneficial.
It is important to point out that there is a large amount of variability in the vitamin D level and omega-3 status for different people with the same intake amount. For example, according to our study, the range of response with 1000 mg of omega-3s EPA+DHA per day was 5.7% to 10.2%. This large amount of variability is similar to what we have observed for vitamin D. Therefore, we recommend that individuals measure their vitamin D level and Omega-3 Index and determine personalized doses for each.
To do this, measure your levels using an at home blood spot test. Once you have your results, use the vitamin D calculator and omega-3 calculator to determine an estimated amount of how much vitamin D and EPA+DHA you will need to achieve the minimum recommended levels of these very important nutrients.






