Published on August 3, 2022
A review describes the bi-directional links between diabetes and COVID-19; could vitamin D and magnesium affect this relationship and help protect from both?
Key Points
- Studies have revealed the possibility of a reverse association between diabetes and COVID-19 – meaning new onset diabetes is increasingly being diagnosed among COVID-19 patients who had no previous history of diabetes
- Magnesium and vitamin D have been shown to help reduce the risk and progression of type 2 diabetes and the severity of COVID-19 infection
- A recent study found that higher vitamin D levels were significantly associated with a decreased incidence of type 2 diabetes only among those with a higher intake of magnesium, and the effect was greater among those who got more magnesium; it is important to get enough magnesium with your vitamin D!
 Increased COVID-19 disease severity has been linked to several independent risk factors, including vitamin D deficiency, obesity, high blood pressure, and diabetes. Magnesium may also help manage the effects of COVID-19 disease, both during and after infection. Studies have demonstrated an association between low magnesium intake and levels, and increased levels of inflammation and oxidative stress. Low magnesium is also associated with a higher incidence of diseases associated with chronic inflammation, such as diabetes, metabolic syndrome, and cardiovascular disease.
Increased COVID-19 disease severity has been linked to several independent risk factors, including vitamin D deficiency, obesity, high blood pressure, and diabetes. Magnesium may also help manage the effects of COVID-19 disease, both during and after infection. Studies have demonstrated an association between low magnesium intake and levels, and increased levels of inflammation and oxidative stress. Low magnesium is also associated with a higher incidence of diseases associated with chronic inflammation, such as diabetes, metabolic syndrome, and cardiovascular disease.
Diabetes specifically affects more than 400 million people around the world, and leads to complications such as cardiovascular disease, neuropathy, kidney damage, and diabetic ketoacidosis (DKA), which is a life-threatening situation. In the past, diabetes has also been associated with a greater risk of infection during the SARS-CoV-1 epidemic, H1N1 pandemic, and the MERS-CoV epidemic.
New-Onset Diabetes Increasingly Diagnosed Among COVID-19 Patients
More recent studies are revealing the possibility of a reverse association between diabetes and COVID-19 – meaning new onset diabetes is increasingly being diagnosed among COVID-19 patients who had no previous history of diabetes. Could COVID-19 infection cause a patient to become diabetic, and if so, how? A review by Viswanathan et al. set out to answer this question, as well as identify the possible roles of vitamin D.
How Could Diabetes Increase Susceptibility to COVID-19?
The following are several pathways that may contribute to increased COVID-19 susceptibility among patients with diabetes.
- Medications that increase ACE-2 expression. Many diabetes patients also suffer from increased blood pressure and cardiovascular disease, which are often treated using medications that have been shown to increase the expression of ACE2 receptors in the epithelial cells of the lung, intestines, kidneys, and heart, which in turn facilitates entry of the SARS-CoV-2 virus into human cells.
- Impaired immunity leads to easier infection. Diabetics have an impaired immune response leading to greater risk of infections due to higher blood sugar and increased oxidative stress, which allows for the virus to proliferate at a much easier, faster rate than a non-diabetic individual.
- Furin, a molecule that is increased in diabetics, has been shown to facilitate SARS-CoV-2 entry into human cells as well as viral replication.
Indications that COVID-19 Might Cause Diabetes
DKA is a severe, life-threatening complication of diabetes that is a result of the blood sugar being too high for too long. This condition that is a result of not having enough insulin (the key diagnosing factor for diabetes) is seen in patients infected with COVID-19, even in the absence of pre-diagnosed diabetes.
Other indications that COVID-19 infection could possibly cause new-onset diabetes or worsen pre-existing diabetes include the following:
- Certain respiratory viruses have been identified as a potential trigger and cause of type 1 diabetes.
- SARS-CoV-2 causes problems with the blood supply to the pancreas, which may impair insulin secretion.
- The increase in systemic inflammation and pro-inflammatory cytokines can directly result in decreased insulin sensitivity, and worsen insulin resistance, leading to diabetes.
Vitamin D is Linked to Metabolic Syndrome and Diabetes
Vitamin D deficiency has been linked to the increased incidence of
Vitamin D supplementation has been found to
- increase beta cell function and insulin sensitivity
- reduce insulin resistance by 15%
- reduce the risk of type 2 diabetes by 40-60%, with achieved vitamin D blood levels of 40-60 ng/ml (100-150 nmol/L)
Magnesium Intake Affects Association between Vitamin D and Risk of Type 2 Diabetes
Magnesium is an important co-nutrient for vitamin D, and is involved in the biosynthesis, transport, and activation of vitamin D. Magnesium is the fourth most abundant mineral in the human body, however, an estimated 42% of young adults have ongoing magnesium deficiency. This can lead to problems with energy metabolism, muscle function, blood pressure regulation, insulin metabolism, cardiovascular function, nerve transmission, neuromuscular contraction, and more.
Studies have shown that poor magnesium status potentially impairs vitamin D metabolism, and an existing magnesium deficiency may result in a vitamin D level that does not increase as much as expected in response to vitamin D supplementation. As illustrated by Deng et al., without sufficient magnesium, the amount of vitamin D that can be metabolized and used by the body is limited and may result in a lack of conversion of vitamin D into its other active forms.
Not Getting Enough Magnesium Can Modify Vitamin D’s Effect on Diabetes
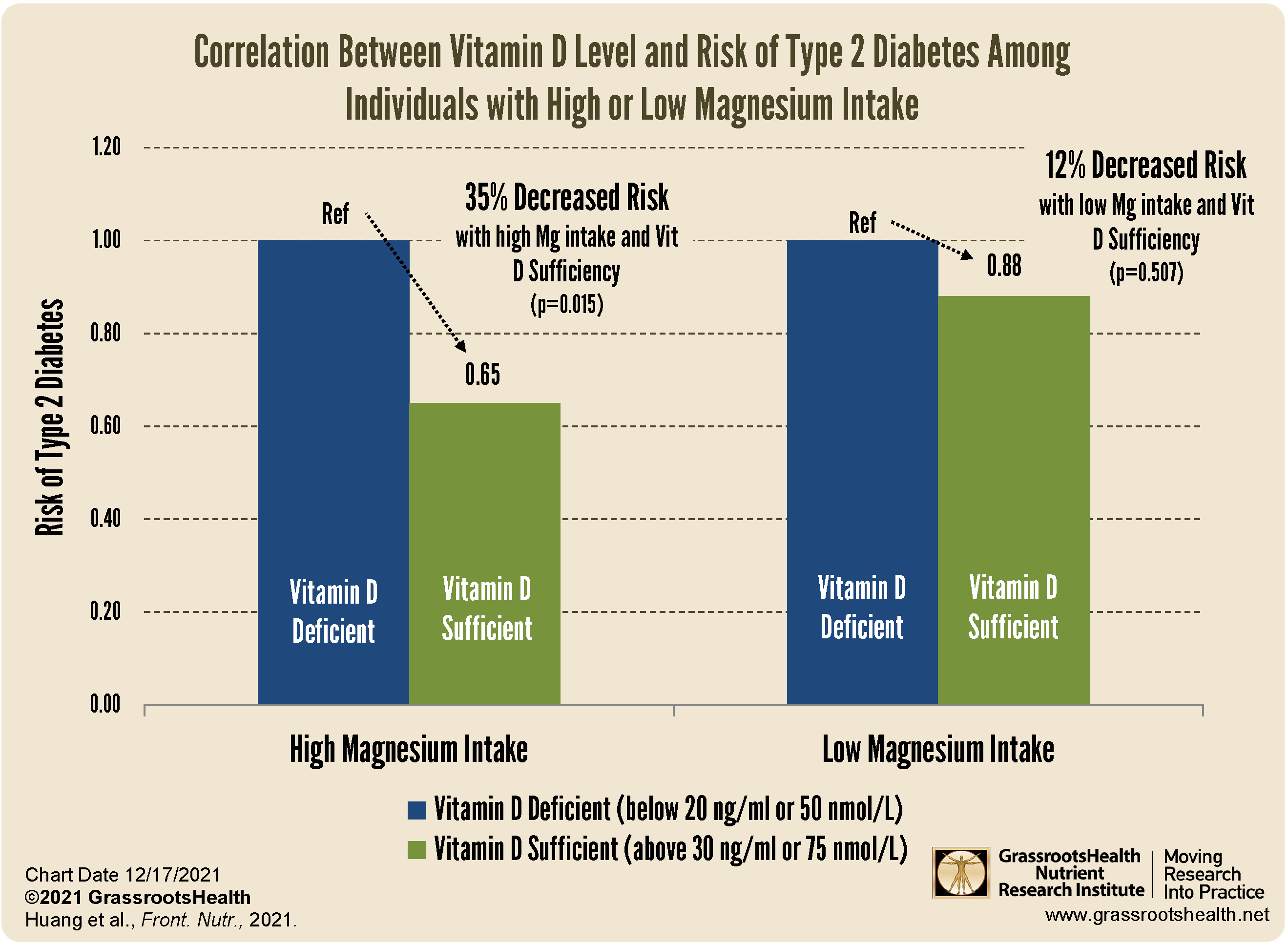
To see if magnesium intake affected the relationship between vitamin D and type 2 diabetes risk, Huang et al. completed a study that looked at whether the effect of vitamin D on the risk of type 2 diabetes differed based on a low versus a high magnesium intake. The authors found that magnesium intake affected the association between vitamin D level and the incidence of type 2 diabetes, where the distribution of vitamin D levels between participants with or without type 2 diabetes was not significantly different in the low magnesium intake group, but was in the high magnesium intake group.
In the group with high magnesium intake, there was a 35% significantly decreased risk of type 2 diabetes among the participants with vitamin D sufficiency compared to those with vitamin D deficiency, compared to the group with low magnesium intake, which only had a 12% decreased risk among those with vitamin D sufficiency, and the finding was not significant.
In other words, higher vitamin D levels were associated with a decreased incidence of type 2 diabetes, and the significance of the effect was greater among those who got more magnesium.
Reduce the Risk of Severe COVID-19 AND Diabetes with Healthy Levels of BOTH Vitamin D and Magnesium
 Having and maintaining healthy vitamin D, magnesium, and other nutrient levels can help improve your health now and for your future. Choose which to measure, such as your vitamin D, omega-3s, and essential minerals including magnesium and zinc, by creating your custom home test kit today. Take steps to improve the status of each of these measurements to benefit your overall health. You can also track your own intakes, symptoms and results to see what works best for YOU.
Having and maintaining healthy vitamin D, magnesium, and other nutrient levels can help improve your health now and for your future. Choose which to measure, such as your vitamin D, omega-3s, and essential minerals including magnesium and zinc, by creating your custom home test kit today. Take steps to improve the status of each of these measurements to benefit your overall health. You can also track your own intakes, symptoms and results to see what works best for YOU.
Enroll and test your levels today, learn what steps to take to improve your status of vitamin D (see below) and other nutrients and blood markers, and take action! By enrolling in the GrassrootsHealth projects, you are not only contributing valuable information to everyone, you are also gaining knowledge about how you could improve your own health through measuring and tracking your nutrient status, and educating yourself on how to improve it.