Published on June 9, 2021
CRP, a biomarker for inflammation linked to many diseases, can be greatly influenced by nutrients including vitamin D, omega-3s, and magnesium
 Chronic, low-level inflammation has been linked to a number of chronic diseases ranging from cardiovascular disease and diabetes to mental health disorders and cancer. The higher the inflammation levels, the higher the risk of developing chronic disease.
Chronic, low-level inflammation has been linked to a number of chronic diseases ranging from cardiovascular disease and diabetes to mental health disorders and cancer. The higher the inflammation levels, the higher the risk of developing chronic disease.
Sometimes an individual will experience symptoms such as pain or fatigue due to inflammation, but often times there will be no symptoms until disease occurs. However, certain markers exist in the blood that can be measured as an indicator of chronic inflammation – one of the most important being C-reactive protein (CRP).
What is C-reactive Protein?
CRP is a protein produced by the liver in response to a very broad range of causes, such as infection from hepatitis and cancer. Elevated CRP levels have been linked to metabolic syndrome, future heart attacks, stoke, peripheral arterial disease, and the development of diabetes. CRP has been used for decades as a general marker of inflammation that can be measured in your blood. Included as an optional addition to the home blood spot tests offered by GrassrootsHealth, the CRP test uses a high sensitivity assay, hs-CRP where “hs” means high sensitivity, to detect small elevations in CRP. Evidence suggests that levels below 1.0 mg/L indicate low risk of cardiovascular disease, levels between 1.0 and 3.0 mg/L indicate average risk, and levels between 3.1 and 10 mg/L indicate increased risk (levels above 10 mg/L most likely indicate an acute infection or injury). Lifestyle changes such as increasing exercise, losing weight, and quitting smoking can lower CRP levels in the long term.
Nutrient Intake and Status can Greatly Affect Inflammation and CRP Levels
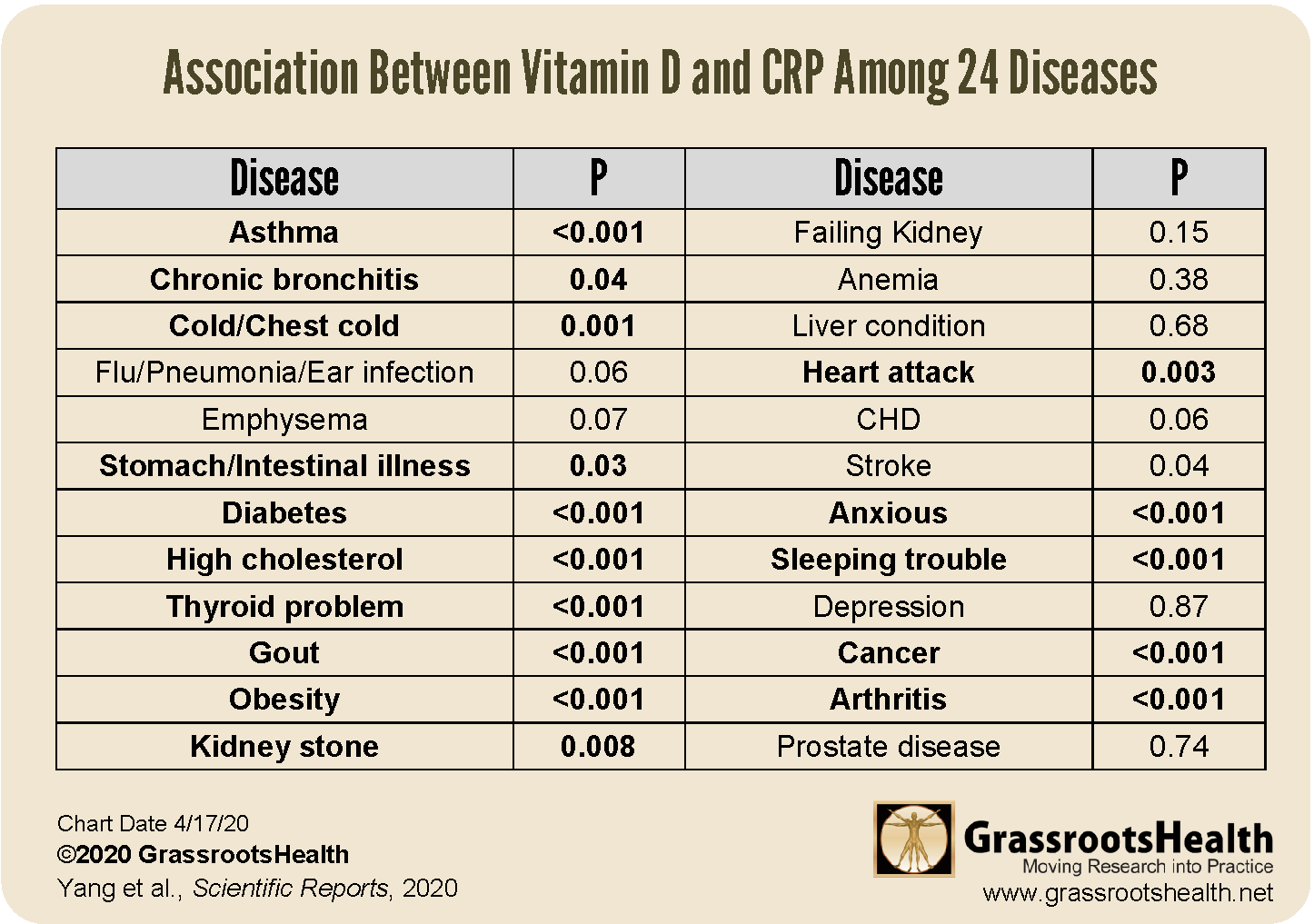
Studies have also associated CRP levels with the intake and status of specific nutrients, including vitamin D, omega-3s, and magnesium. For example, a study by Yang et al. highlighted the relationship between CRP and vitamin D levels in 24 different diseases. The authors discovered a negative association between CRP and vitamin D levels overall, with higher levels of vitamin D associated with lower levels of CRP. The strength of associations varied among diseases, with a steady linear relationship for some (such as respiratory, gastrointestinal, and mental diseases), and a non-linear relationship for others (such as diabetes and cancer), meaning the effect of vitamin D on CRP levels was greater at lower levels but slowed at higher levels of vitamin D, with an eventual plateau. Cancer had a higher cut-off value of vitamin D than other diseases, meaning that after other diseases reached a plateau with vitamin D, cancer still showed a reduced risk from higher levels.
The table below further outlines the association between CRP and vitamin D among the 24 different diseases. Diseases in bold are those that had a statistically significant relationship between vitamin D and CRP levels.
Cardiovascular Disease (CVD), CRP, and Vitamin D
Inflammation is a risk factor for heart disease and stroke much the same as factors like smoking, high blood pressure and high blood triglycerides increase risk. A series of studies have shown that CRP is a better predictor of cardiovascular risk than other blood tests such as cholesterol. CRP levels can be used by your doctor to assess your risk of developing coronary artery disease and heart attack. In fact, measuring CRP allows doctors to predict your risk of having a heart attack over the next 5 to 10 years if you have risk factors for heart disease.
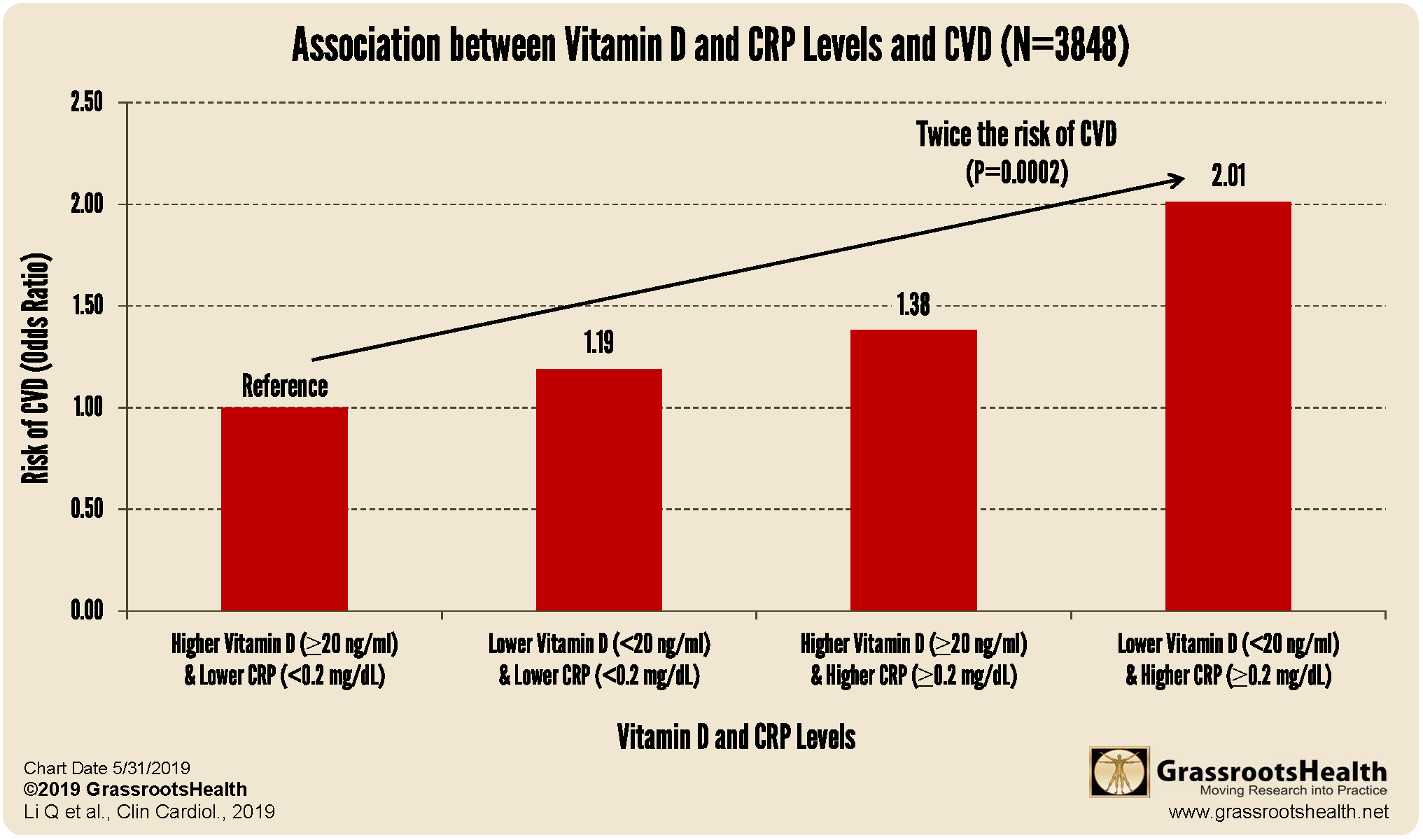
Results from a study assessing the association between CRP, vitamin D levels and CVD found that participants with vitamin D levels less than 10 ng/ml (25 nmol/L) had a 90% increased risk of CVD compared to those with levels at or above 30 ng/ml (75 nmol/L). Also, those with CRP levels at 0.2 mg/dL or higher had a 47% increased risk of CVD compared to those with levels less than 0.2 mg/dL. The chart below shows that when both vitamin D and CRP are considered together, participants with vitamin D levels below 20 ng/ml and CRP levels at or above 0.2 mg/dL had twice the risk of CVD compared to participants with vitamin D levels at or above 20 ng/ml and CRP levels less than 0.2 mg/dL.
In a separate analysis, when the association between vitamin D and CVD was assessed for those with CRP at or above versus below 0.2 mg/dL, a significant association was only observed for the higher CRP group. These findings indicate that improving vitamin D status is particularly important in relation to CVD risk for those with higher CRP levels.
Are Omega-3s Comparable to Statins for Heart Health?
Omega-3 fatty acids are also well known to provide healthful benefits for the heart, reduce inflammation and reduce the risk of death.
A study by Kelley et al. investigated the effects of supplementation with 3 grams per day of DHA on levels of inflammation in men with high blood lipid levels in comparison with those receiving placebo (olive oil) over 3 months. Those receiving the DHA had significantly lower levels of several markers of inflammation (including CRP and IL-6) after 3 months than the placebo group, with a 15% reduction in CRP levels at 90 days. Of note, the reduction in CRP concentrations found in this study was comparable to the 15-25% reduction in CRP caused by statins (the frontline pharmaceuticals used to prevent heart attacks and stroke) without any of the adverse effects.
Cancer Risk, CRP, and Magnesium
CRP has been associated with the risk of certain cancers, such as colorectal cancer, lung cancer, and breast cancer. According to Huang et al., chronic low-grade inflammation is linked to the development of approximately 20% of all cancers. These authors looked at magnesium intake and the risk of breast cancer and found a significant inverse relationship, with higher intakes being associated with lower risk. Overall, there was a 22% reduction in breast cancer risk associated with those whose magnesium intake was at least 280 mg/day compared to those whose magnesium intake was lower than 280 mg/day. There was also a significant increase in breast cancer risk when comparing participants with higher CRP levels; those with higher CRP and more chronic inflammation had a 1.43 times higher breast cancer risk compared to those with lower CRP levels and less chronic inflammation. (Note that the CRP units used by GrassrootsHealth are mg/L, so these values would be equivalent to >3 mg/L and <=3 mg/L.)
Mental Health, CRP, and Vitamin D
Multiple studies have found a direct correlation between levels of inflammation and mental health. In a previous blog, we reviewed a study assessing the effects of chronic inflammation on cognitive health, where higher levels of CRP were related to an increase in cognitive decline. A meta-analysis by Jamilian et al. reviewed the research available on inflammation, mental health, and vitamin D in patients diagnosed with psychiatric disorders. The review found a significant reduction in depression, improved quality of sleep, and a significant reduction in CRP following vitamin D supplementation.
Additional Relationships between CRP, Nutrients, and Disease Outcomes
Other diseases related to increased CRP levels which may be improved with certain nutrients include
- Multiple Sclerosis (with Vitamin D and Omega-3s)
- Gestational Diabetes and Neonatal Outcomes (with Vitamin D and Omega-3s)
- Pregnancy Outcomes among Pregnant Women with Gestational Diabetes (with Magnesium, Zinc, Calcium and Vitamin D)
- Liver Health (with Vitamin D)
Could Your Levels of Inflammation and CRP Improve with Vitamin D, Omega-3s, and Other Nutrients?
Reducing chronic inflammation can improve overall health and decrease the risk of many diseases. Add the hsCRP blood spot test to any GrassrootsHealth test kit to measure your level of inflammation, while also measuring your vitamin D, omega-3s, and essential minerals such as magnesium and zinc, by creating your custom home test kit today. Take steps to improve the status of each of these measurements to benefit your overall health. You can also track your own intakes, symptoms and results to see what works best for YOU.
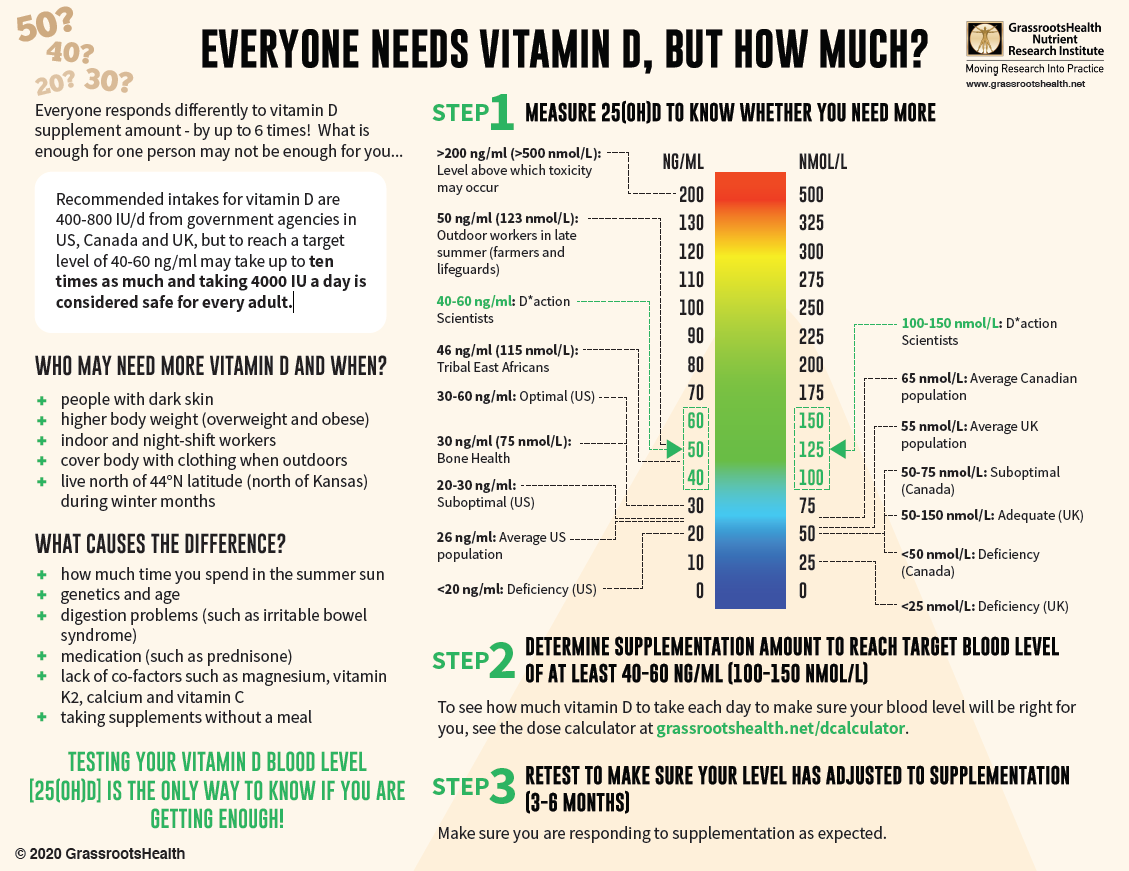
When it comes to vitamin D especially, correcting a deficiency at any age and any time of life can decrease potential disease severity and improve outcomes. With almost 90% of the general population having vitamin D levels below the recommended 40-60 ng/ml (100-150 nmol/L), it is obvious that most people need more vitamin D. While most of us cannot achieve a vitamin D level of 40-60 ng/ml from sun alone, either due to our lifestyle, where we live, or other circumstances, we can certainly reach those levels with the right amount of supplementation.
Below is a guide for how much you might need, and who may need more. Your levels can be tested safely at home – order your home test kit today.
By joining the GrassrootsHealth projects, you are not only contributing valuable information to our study, but you are also gaining knowledge about how you could improve your own health through measuring and tracking your nutrient status, and educating yourself on how to improve it. Do you know what your status of vitamin D, omega-3s, and other essential nutrients is? Could your levels be improved? Test now to find out!
 We now have a NEW GIFTING SERVICE that allows you to quickly send ‘Gift Cards’ to friends, family and coworkers who you consider might need immediate access to testing, and to Claim the Joy of Your Health TODAY. Give the gift today!
We now have a NEW GIFTING SERVICE that allows you to quickly send ‘Gift Cards’ to friends, family and coworkers who you consider might need immediate access to testing, and to Claim the Joy of Your Health TODAY. Give the gift today!