Published on August 21, 2020
In a recent post, we introduced the immune system and how it works to protect your body from infection and disease. Your immune system is not one organ like your liver or kidney, but is composed of a group of organs, tissues and cells that work together to defend the body from invaders. There are several levels of this complex system that interact to protect you.
The first line of defense, the “innate” system, forms a protective barrier (physical, chemical and biological) around the body and includes immediate non-specific defense mechanisms. In addition, there are chemical factors (complement, acute-phase proteins and cytokines) and several types of non-specific immune cell types that roam around in the blood and tissues of the body on the look-out for pathogens (bacteria and viruses that cause disease).
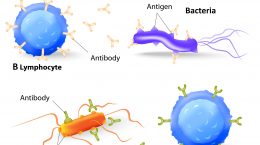
These non-specific immune cells, called “phagocytes,” are a key component of the first line of defense and the focus of this article. Phagocytes, through a process called phagocytosis, gobble up (engulf) and kill (digest) bad bugs (pathogens) when they recognize them. The digested bits, called “antigens,” are then presented to cells of the adaptive immune system – B and T lymphocytes which we will discuss in parts 3 and 4 of this series on immune system function.
What Are Phagocytes?
There are three main groups of cells that act as phagocytes with slightly different functions:
 1. Monocytes and macrophages: Monocytes are phagocytes that travel around in the bloodstream and macrophages (more mature monocytes) live in the tissues. Macrophages then stimulate T cells (part of the adaptive, or learned, immune response) by presenting them with bits of pathogens (antigens) they have broken down (digested). They also secrete chemical signals (cytokines) to initiate inflammation and recruit other immune cells to the area.
1. Monocytes and macrophages: Monocytes are phagocytes that travel around in the bloodstream and macrophages (more mature monocytes) live in the tissues. Macrophages then stimulate T cells (part of the adaptive, or learned, immune response) by presenting them with bits of pathogens (antigens) they have broken down (digested). They also secrete chemical signals (cytokines) to initiate inflammation and recruit other immune cells to the area.
 2. Neutrophils: These are the most prevalent white blood cell in the blood and have an important role in acute inflammation. Neutrophils are often the first immune cells to show up at the site of an infection. Neutrophils have “granules” filled with toxic substances, including antimicrobial peptides, enzymes and reactive oxygen species that are used to kill the pathogen. Neutrophils specialize in killing pathogens that have already gained access to cells of the body and are important for initiating inflammation and calling in other immune cells to deal with the infection.
2. Neutrophils: These are the most prevalent white blood cell in the blood and have an important role in acute inflammation. Neutrophils are often the first immune cells to show up at the site of an infection. Neutrophils have “granules” filled with toxic substances, including antimicrobial peptides, enzymes and reactive oxygen species that are used to kill the pathogen. Neutrophils specialize in killing pathogens that have already gained access to cells of the body and are important for initiating inflammation and calling in other immune cells to deal with the infection.
 3. Dendritic cells*: These cells are the major bridge between the innate (initial response) and adaptive (learned response) immune systems. Dendritic cells travel everywhere throughout the body – in blood, tissues, and lymphoid organs – and their job is to “sample” or check out all the cells they encounter. When they detect a pathogen and phagocytose (engulf) it, they then seek out T cells to present them to, connecting the innate and adaptive immune response. If the T cell recognizes the antigen the adaptive immune response is initiated.
3. Dendritic cells*: These cells are the major bridge between the innate (initial response) and adaptive (learned response) immune systems. Dendritic cells travel everywhere throughout the body – in blood, tissues, and lymphoid organs – and their job is to “sample” or check out all the cells they encounter. When they detect a pathogen and phagocytose (engulf) it, they then seek out T cells to present them to, connecting the innate and adaptive immune response. If the T cell recognizes the antigen the adaptive immune response is initiated.
*Dendritic cells have many projections or arms that they use to sample cells with. These arms look like the dendrites of neurons and the reason why dendritic cells got their name.
How Do Phagocytes Recognize Pathogens?
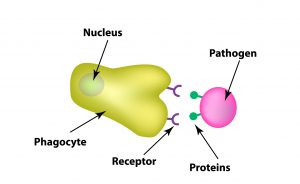 When a phagocyte “samples” a cell (including your own cells, or bacteria and viruses that have invaded the body), it is testing it to see if that cell is a pathogen or not. All cells have unique features like humans do and they look different from one another. Cells have protein markers on their surface that can be thought of as facial features. A liver cell may have blue eyes, an oval face and green hair. An infected liver cell may look very similar to the original, but it also has a wart on it, allowing you to distinguish it as infected. The phagocytes use these features to sample the cell.
When a phagocyte “samples” a cell (including your own cells, or bacteria and viruses that have invaded the body), it is testing it to see if that cell is a pathogen or not. All cells have unique features like humans do and they look different from one another. Cells have protein markers on their surface that can be thought of as facial features. A liver cell may have blue eyes, an oval face and green hair. An infected liver cell may look very similar to the original, but it also has a wart on it, allowing you to distinguish it as infected. The phagocytes use these features to sample the cell.
Pathogens have unique features or “flavors,” called pathogen-associated molecular patterns (PAMPs), that while unique to the pathogen, make it stand out as alien – like the wart above. Phagocytes recognize them as pathogens because they have certain “tasters,” pattern recognition receptors (PRPs), looking out for these features (PAMPs) that our human cells do not have.
Once the PRP has recognized a PAMP it binds the cell, called “adherence,” this begins the process of phagocytosis.
Phagocytosis
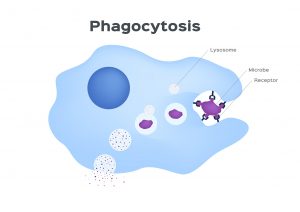 The process of phagocytosis involves the phagocyte engulfing the pathogen, or cell that is infected, and exposing it to toxic chemicals to kill and digest it. This happens in several stages, starting with adherence and new immune cells “migrating” or travelling to the site of inflammation.
The process of phagocytosis involves the phagocyte engulfing the pathogen, or cell that is infected, and exposing it to toxic chemicals to kill and digest it. This happens in several stages, starting with adherence and new immune cells “migrating” or travelling to the site of inflammation.
Once the phagocytes’ PRP has bound to the pathogens’ PAMP it starts to internalize it. It does this by making “arms” that reach out and surround the target cell. The arms create a bubble containing the pathogen within the phagocyte, called a “phagosome.”
Next, an organ within the phagocyte called a lysosome joins together with the phagosome (creating a phagolysosome). The lysosome is important because it is filled with digestive enzymes and toxic chemicals that work to break down the pathogen.
The death blow can occur from the toxic chemicals in the lysosome or through creation of a “respiratory burst” which uses deadly reactive oxygen species (ROS), such as superoxide (O2-), to attack and kill the pathogen.
Antioxidants and Balance
The actions of the innate immune cells are immediate, nonspecific and lack memory (meaning that the same response is mounted regardless of how often the same pathogen is encountered). Because of the lack of specificity though, these actions can also result in damage to the body’s tissues. Antioxidants act to prevent formation of ROS and to neutralize active ROS.
Superoxide dismutase (SOD) is an important enzyme that also helps protect human cells from ROS. SOD converts the superoxide radicals into hydrogen peroxide (H2O2) to prevent damage. It quickly neutralizes any molecule that may develop into a free radical. The function of SOD requires copper, zinc, manganese, iron and nickel.
The generation of reactive oxygen species (ROS) through the respiratory burst are important for killing the pathogen, but the ROS can react with cells of the human body and cause damage. Antioxidants, such as vitamin C and E, scavenge for and neutralize these ROS are important in dealing with ROS that have leaked out before they cause damage to the body.
The Role of Micronutrients in the Process of Phagocytosis
Vitamins A, C, D, E, and B12, zinc, copper, iron and selenium are important for all stages of phagocytosis. These micronutrients are also needed to produce the enzymes needed to digest and kill the pathogen. (1)
In the first stages of phagocytosis, vitamin E is necessary for binding of the PRP to the PAMP. (2) Vitamins A and C are required for migration of immune cells to the site of infection and for engulfing the pathogen. (3) Vitamin D is needed for the process of maturation of monocytes in macrophages. (4) (Learn more about how immune cells rely on vitamin D here.) Zinc deficiency results in impaired immune function in general and reduced monocyte phagocytosis. (5)
Interestingly, neutrophils that are activated have 10X’s higher concentrations of vitamin C than normal neutrophils. (6) Copper deficiency results in decreased numbers of neutrophils and impaired function. (7) Iron deficiency compromises the ability of neutrophils to kill bacteria. (8)
As mentioned above (What Are Phagocytes?), part of the response from phagocytes involves sending inflammation signals and recruiting other immune cells to help kill the pathogen and repair any injury. Cytokines are chemical signals released by immune cells. Some cytokines signal inflammation (e.g. IL-1, TNF-α and IFNγ) while others, called chemokines, direct phagocytes, T cells and other immune cells to the site of infection. The production of cytokines requires vitamin D, zinc and selenium, among other nutrients.
A micronutrient deficiency can inhibit the immune response and result in increased susceptibility to infection.
What can you do with this information?
Learn more about how specific nutrients play direct roles in the various processes of the immune system response to infection and be sure to get enough of each. Do you know your nutrient levels? Do you know your levels of inflammation? Find out by testing your vitamin D, omega-3s, magnesium and other essential elements (including copper and zinc), as well as your inflammation levels, with home test kits offered by GrassrootsHealth. Measuring levels is the only way to know if you are supporting your immune system and whether additional changes should be made, with supplementation, dietary changes, or both.
Are You Getting Enough Vitamin D to Help Yourself?
We’re in a time of great crisis that could be greatly affected by making sure you and everyone you know has a serum level of at least 40 ng/ml. Help us help you.
Do you know what your vitamin D level is? Be sure to test today to find out, and take steps to keep it within a target of 40-60 ng/ml or 100-150 nmol/L! Give your immune system the nutrients it needs to support a healthy you and protect yourself from unnecessary diseases.
GrassrootsHealth Nutrient Research Institute is preparing to do a Community RCT with the use of our myData-myAnswers nutrient health system that over 15,000 people are already using for their health. We will demonstrate how one can use the Nutrient Research Model established by Dr. Robert Heaney to establish the effect of vitamin D serum levels of at least 40 ng/ml (100 nmol/L) on risk reduction with different ethnicities in the population. Please let us know if you’re interested in helping sponsor this project.
CLICK HERE for updates and new information about the project.
Through GrassrootsHealth Nutrient Research Institute, you can also test your essential elements magnesium, copper, zinc and selenium, toxins such as lead, mercury and cadmium, as well as your omega-3 levels, inflammation levels and thyroid stimulating hormone (TSH) level. Find out your levels today! Log on to the test selection page (click the link below) to get your tests and see for yourself if your levels can be improved.
Make sure you track your results before and after, about every 6 months!
Click Here to Access the Test Page
How can I track my nutrient intake and levels over time?
To help you track your supplement use and nutrient levels, GrassrootsHealth has created the Personal Health Nutrient Decision System called
For each specific supplement, you can track what days you take it, how much, and many other details. This will help you know your true supplemental intake and what patterns of use work for you to reach and maintain optimum nutrient levels. Check it out today!