Published on January 22, 2025
Maternal Health Awareness Day is January 23rd – It’s easy to improve maternal health outcomes NOW with something as simple, effective, and inexpensive as vitamin D and omega-3s
Key Points
- Pregnancy may be the most important time during the lifecycle that adequate vitamin D status should be ensured; studies continue to demonstrate health benefits extending to both the pregnant mother and the baby when enough vitamin D is given during the prenatal period
- One study found a vast majority of prenatal patients (89%) had vitamin D levels less than 40 ng/ml on their first vitamin D test and almost one-third (31%) had vitamin D levels less than 20 ng/ml; black women had particularly low vitamin D levels; almost all (99%) were less than 40 ng/ml and approximately two-thirds (65%) were less than 20 ng/ml
- Omega-3s are also important; so important that in 2021, the Australian Government officially added omega-3 fatty acid supplementation to their list of recommendations for pregnant women, with a warning issued that low omega-3 levels could increase the chance of preterm birth
 Tomorrow is Maternal Health Awareness Day with a goal of improving maternal health outcomes. What kind of an impact could be made NOW for all women if the focus was on improving prenatal vitamin D levels?
Tomorrow is Maternal Health Awareness Day with a goal of improving maternal health outcomes. What kind of an impact could be made NOW for all women if the focus was on improving prenatal vitamin D levels?
Pregnancy may be the most important time during the lifecycle that adequate vitamin D status should be ensured. Studies continue to demonstrate health benefits extending to both the pregnant mother and the baby when enough vitamin D is given during the prenatal period. Vitamin D levels in the range of 40-60 ng/ml (100-150 nmol/L) have been shown to be especially protective during pregnancy, reducing the risk of complications such as preterm birth, hypertensive disorders of pregnancy (preeclampsia) and gestational diabetes.
Recent studies have added strength to the evidence of benefits due to adequate prenatal vitamin D to the child as well, including a reduced risk of asthma and improved lung function, better neurodevelopmental outcomes, and a reduced risk for immune function impairment. Health conditions in the child that have been associated with prenatal vitamin D deficiency also include ear and lung infections, autism, type 1 diabetes and other autoimmune conditions, and an increased risk for certain cancers and cardiovascular disease later in life.
Key Point: Changes in Vitamin D Metabolism During Pregnancy Indicate its Extreme Importance
Pregnancy initiates a unique change to vitamin D metabolism that happens at no other time during the lifecycle. During pregnancy, conversion of 25(OH)D to the hormonal form, 1,25(OH)2D, increases so that by 12 weeks, levels in the blood are triple that of normal, non-pregnant female and normal male subjects. In a non-pregnant person, these levels would alter calcium concentrations in the blood and result in toxicity and potential death, but these are perfectly normal levels during pregnancy. Furthermore, the rise in 1,25(OH)2D is independent of the calcium system, nor is it controlled by parathyroid hormone, which is the only time in the lifecycle that this un-coupling occurs. Further observation has revealed that the direct influence of 25(OH)D (up to ~40 ng/ml) on 1,25(OH)2D levels is also unique to pregnant women.
Other studies have demonstrated how vitamin D levels (as 25(OH)D) naturally increase during pregnancy when there is an adequate supply of vitamin D3 or sunshine, as clearly illustrated by Luxwolda et al.. This study investigated the vitamin D status across the life cycle in various East African populations to determine what serum 25(OH)D level represents sufficient status among populations whose lifestyle closely matches that of our ancestors; the average serum 25(OH)D level of this population as a whole was at least 40 ng/ml. However, 25(OH)D levels in pregnancy were far higher than in non-pregnant individuals, indicating the higher vitamin D need for the mother during pregnancy.
 Learn More: A Time Especially Sensitive to Vitamin D – When Deficiency Can Result in Life-Long Consequences
Learn More: A Time Especially Sensitive to Vitamin D – When Deficiency Can Result in Life-Long Consequences
Read about some of the most compelling evidence of the need for a minimum vitamin D level of 40 ng/ml (100 nmol/L) and how fulfilling the unique need for vitamin D during pregnancy can impact prenatal, newborn & lifelong health
Most Women of Childbearing Age are Vitamin D Deficient; Black Women Have the Highest Risk
The Medical University of South Carolina (MUSC) implemented routine vitamin D testing for all pregnant patients as part of a project in collaboration with GrassrootsHealth. MUSC Health is a comprehensive, urban medical center treating a large, diverse population of women. A vast majority of prenatal patients (89%) had vitamin D levels less than 40 ng/ml on their first vitamin D test and almost one-third (31%) had vitamin D levels less than 20 ng/ml. Black women had particularly low vitamin D levels; almost all (99%) were less than 40 ng/ml and approximately two-thirds (65%) were less than 20 ng/ml. These vitamin D levels are representative of prenatal vitamin D levels across the United States.
 Learn More: United States Receives D+ Grade, Highest Preterm Birth Rate in 15 Years
Learn More: United States Receives D+ Grade, Highest Preterm Birth Rate in 15 Years
The March of Dimes has been reporting a worsening health crisis for pregnant women and their babies, yet preterm birth risk can be reduced drastically, simply by incorporating nutrients such as vitamin D and omega-3s into the prenatal care routine
Black women have a 15-20 fold higher prevalence of severe vitamin D deficiency, putting them at much higher risk for preterm birth. According to NHANES data, approximately 68% of Black women have vitamin D levels below 20 ng/ml (50 nmol/L) and at these levels, would be expected to have a 20% preterm birth rate; this is a problem that must be addressed especially for mothers within these groups of darker skin! Research has shown that the gap in preterm birth outcomes between White and Black mothers virtually disappears when vitamin D deficiency is corrected.
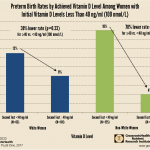
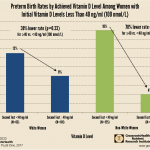
A greatest impact on maternal and infant health could be made simply by addressing vitamin D deficiency among Blacks; in fact, approximately 68% of Black women have vitamin D levels below 20 ng/ml (50 nmol/L) and at these levels, would be expected to have a 20% preterm birth rate
Maternal Health Outcomes Affected by Vitamin D
The following are just a few more of the many studies demonstrating the effects of vitamin D on prenatal health:
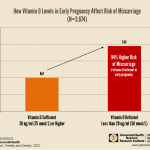
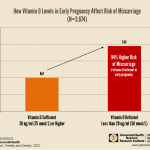
Vitamin D deficiency was found to increase risk of miscarriage by 94% and increase risk of recurrent miscarriage 4 times; vitamin D deficiency among male partners can also contribute to risk
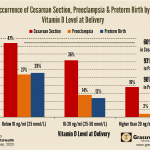
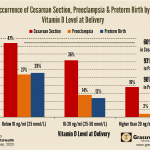
New study finds 60% reduction in cesarean section, 93% reduction in preeclampsia, and 96% reduction in preterm birth among women whose vitamin D level was higher than 20 ng/ml vs below 10 ng/ml at birth
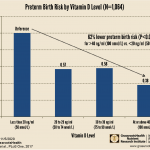
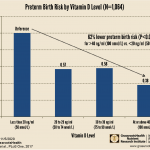
Researchers found that women with vitamin D levels at or above 40 ng/ml (100 nmol/L) had a 62% lower risk of preterm birth compared to women with levels less than 20 ng/ml (50 nmol/L) (p<0.0001). This lower risk remained after adjusting for socioeconomic variables.
Study shows women with higher vitamin D levels at the beginning stage of labor reported less pain during labor and after birth; higher vitamin D levels have also been associated with a reduced risk of cesarean section
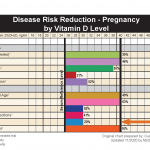
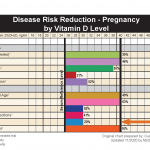
Numerous studies have found that higher vitamin D levels among pregnant women reduce the risk of adverse maternal and infant outcomes. We reviewed and compiled many of these findings to create an updated version of the Pregnancy Disease Risk Reduction Chart, found here.
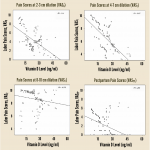
Omega-3 Fatty Acids are also Important for Prenatal and Newborn Health
Omega-3s are so important, in fact, that in 2021, the Australian Government officially added omega-3 fatty acid supplementation to their list of recommendations for pregnant women, with a warning issued that low omega-3 levels could increase the chance of preterm birth. Several studies have demonstrated this effect, such as a study by Carlson et al., in which a higher intake of EPA and DHA resulted in an approximate decrease of 70% for early preterm birth, 85% for very low birth weight, and 60% for low birth weight. Additionally, when combining data from 9 different randomized controlled trials on omega-3 supplementation and preterm birth, Kar et al. found that omega-3 intake was associated with a 58% reduced risk of early preterm delivery, while a 17% decreased risk of any preterm birth was seen among women who supplemented with omega-3s.
Other studies have shown a relationship between omega-3 intake or status during pregnancy and outcomes such as infant immunity and the incidence of postpartum depression. In fact, Markhus et al. showed that a higher Omega-3 Index at the end of pregnancy greatly reduced the risk of postpartum depression.
Ensuring Adequate Levels of Vitamin D and Omega-3s are an Easy Way to Improve Many Aspects of Prenatal Health


What impact could improving levels of these essential nutrients make for the health of pregnant women and their babies?
Find out if you or a loved one are getting enough vitamin D and omega-3s. Save 15% when measuring both with your home blood spot test kit!
Check Now and Save 15% with Code OMEGA3S
Create Your Custom Home Test Kit


You can also measure your:
- Vitamin D
- Magnesium PLUS Essential and Toxic Elements
- Omega-3 Fatty Acids
- hsCRP
- HbA1c
- TSH
- Type 1 Diabetes Autoantibodies
Did you know that each of the above can be measured at home using a simple blood spot test? As part of our ongoing research project, you can order your home blood spot test kit to get your levels, followed by education and steps to take to help you reach your optimal target levels. Start by enrolling and ordering your kit to measure each of the above important markers, and make sure you are getting enough of each to support better mood and wellbeing!
Create your custom home test kit today. Take steps to improve the status of each of these measurements to benefit your overall health. With measurement you can then determine how much is needed and steps to achieve your goals. You can also track your own intakes, symptoms and results to see what works best for YOU.