Published on November 11, 2019
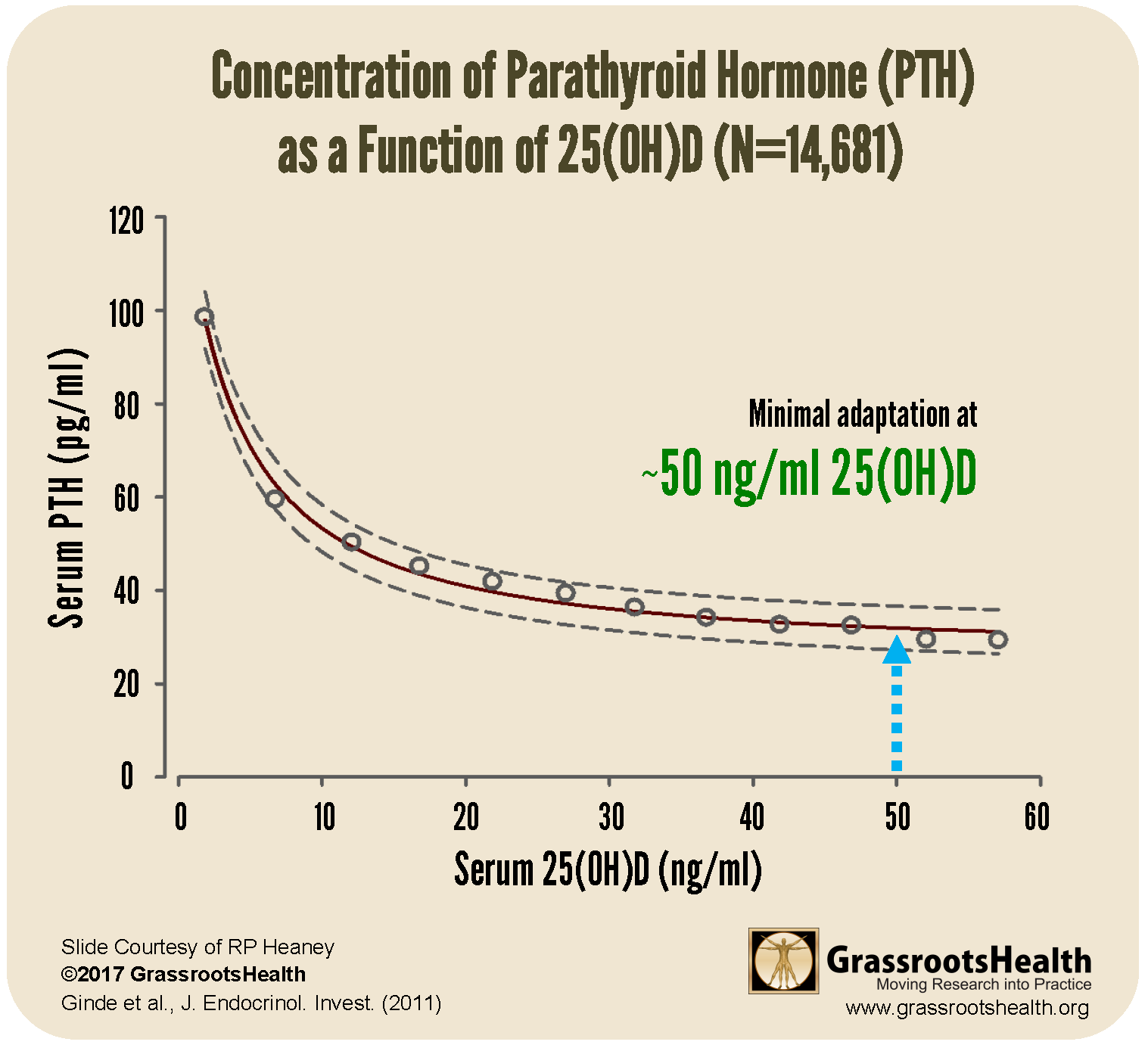
A physiological function of vitamin D is to help regulate the absorption of calcium. Low calcium absorption (caused by either low calcium or vitamin D) causes parathyroid hormone (PTH) levels to rise, which increases the activation of vitamin D to then increase calcium absorption.
As illustrated in the chart above, PTH varies inversely with vitamin D status when 25(OH)D concentration is inadequate. The point at which increased levels of 25(OH)D no longer result in decreased levels of PTH (PTH level remains stable) is around 50 ng/ml 25(OH)D. Therefore, from a physiological perspective, ‘normal’ vitamin D status would be a 25(OH)D concentration that requires little or no compensatory PTH response under standard conditions, at around 50 ng/ml.
Low Magnesium Shown to Alter the Vitamin D-PTH Relationship
Magnesium status has also been shown to influence PTH in previous studies, and magnesium is a well-known co-factor of vitamin D; when magnesium status is deficient, vitamin D metabolism becomes affected.
 A recent study by Cheung et al. observed the effect of varying intake levels of magnesium on the relationship between PTH and vitamin D in overweight and obese adults, with the hypothesis that poor magnesium status potentially impairs vitamin D metabolism enough to limit the PTH response. They divided a total of 57 participants with a BMI between 25 – 45 into 3 groups according to magnesium intake and measured levels of 25(OH)D and PTH. Each group had an average BMI of approximately 28 and an average vitamin D level of approximately 26 ng/ml. What they found was that only the high magnesium intake group, with intakes of 283 to 852 mg per day, displayed the expected inverse relationship between vitamin D and PTH levels; the low magnesium intake (45 – 167 mg/day) and medium magnesium intake (177 – 281 mg/day) groups showed no association between vitamin D and PTH levels.
A recent study by Cheung et al. observed the effect of varying intake levels of magnesium on the relationship between PTH and vitamin D in overweight and obese adults, with the hypothesis that poor magnesium status potentially impairs vitamin D metabolism enough to limit the PTH response. They divided a total of 57 participants with a BMI between 25 – 45 into 3 groups according to magnesium intake and measured levels of 25(OH)D and PTH. Each group had an average BMI of approximately 28 and an average vitamin D level of approximately 26 ng/ml. What they found was that only the high magnesium intake group, with intakes of 283 to 852 mg per day, displayed the expected inverse relationship between vitamin D and PTH levels; the low magnesium intake (45 – 167 mg/day) and medium magnesium intake (177 – 281 mg/day) groups showed no association between vitamin D and PTH levels.
These findings validated their hypothesis that low magnesium may hinder the ability of vitamin D to regulate PTH and calcium absorption in overweight and obese adults, emphasizing the importance of maintaining sufficient magnesium intake in order to optimize the function of vitamin D.
How are your nutrient levels responding to supplementation?
Make sure you know your vitamin D level (with a target of 40-60 ng/ml or 100-150 nmol/L) and Omega-3 Index (with a target of 8% or higher) levels, as well as your levels of essential nutrients, such as magensium. Through GrassrootsHealth Nutrient Research Institute, you can also test your inflammation levels, including your level of hsCRP. Find out your levels today! Log on to the shop (click the link below) to get your tests and see for yourself if your level can be improved.
Make sure you track your results before and after, about every 6 months!
How can I track my nutrient intake and levels over time?
To help you track your supplement use and nutrient levels, GrassrootsHealth has created an online tracking system called myData-myAnswers. For each specific supplement, you can track what days you take it, how much, and many other details. This will help you know your true supplemental intake and what patterns of use work for you to reach and maintain optimum nutrient levels. Check it out today!