Published on October 11, 2022
A secondary analysis of the VITAL trial results found a 38% decreased risk of metastatic cancer among participants with a normal BMI who supplemented with vitamin D
Key Points
- Data from the VITAL study showed a significant reduction of metastatic or fatal cancer among those with a normal BMI, with a decreased risk of 38% among those taking vitamin D compared to placebo; in those who were overweight (BMI above 30), average vitamin D levels did not reach 40 ng/ml with supplementation, and the findings among that group were non-significant
- Evidence shows that vitamin D levels are greatly affected by obesity; the more fat a person has on their body (the higher the BMI), the more likely they are to have vitamin D deficiency, and their need for vitamin D increases. In fact, the amount of vitamin D needed on a daily basis to achieve a vitamin D level of 40 ng/ml (100 nmol/L) can vary by as much as 3 times the amount, depending on BMI.
- Other nutrients are also important for reducing the risk of breast cancer and improving outcomes among women who get breast cancer, including omega-3s, magnesium, selenium, and vitamin C
 October 13th is Metastatic Breast Cancer Awareness Day. Metastatic cancer (also known as Stage 4 cancer) is a cancer that has spread from its primary location to other tissues or organs in the body. According to breastcancer.org, approximately 30% of early-stage breast cancers will eventually become metastatic breast cancer.
October 13th is Metastatic Breast Cancer Awareness Day. Metastatic cancer (also known as Stage 4 cancer) is a cancer that has spread from its primary location to other tissues or organs in the body. According to breastcancer.org, approximately 30% of early-stage breast cancers will eventually become metastatic breast cancer.
Vitamin D has known anticancer effects, and much research has been published over the last several decades showing a link between vitamin D levels and cancer risk. The VITAL trial was a recent, randomized, double blind, placebo-controlled clinical trial conducted in multiple centers around the United States. It included 25,871 participants who were free of cancer and cardiovascular disease diagnoses at baseline. Participants were either male, ages 50 years and older, or female, ages 55 years and older. Participants were given 2000 IU vitamin D per day and 1 gram of marine omega-3 fatty acids per day, or placebo. The average vitamin D level at baseline among all participants was about 30 ng/ml (75 nmol/L).
Initial findings from the VITAL trial were published in November of 2018; one paper compared cancer outcomes between those assigned to vitamin D (2000 IU/day) vs. placebo. When cancer outcome results were analyzed excluding the first two years after study initiation (allowing time for vitamin D to have an effect), there was a 25% reduced risk of cancer mortality among those taking vitamin D (p=0.02). However, the paper concluded that there was only a possible reduction in fatal cancer with vitamin D supplementation, noting a potential effect modification by body mass index (BMI).
Vitamin D Supplementation Analysis by BMI
A secondary analysis of the VITAL randomized clinical trial data by Chandler et al. was completed to determine the effect of daily 2,000 IU vitamin D supplementation on the development of advanced, metastatic cancer and cancer death with BMI (grouped as below 25, 25 to under 30, and above 30) included to see if it modified the effects of supplementation.
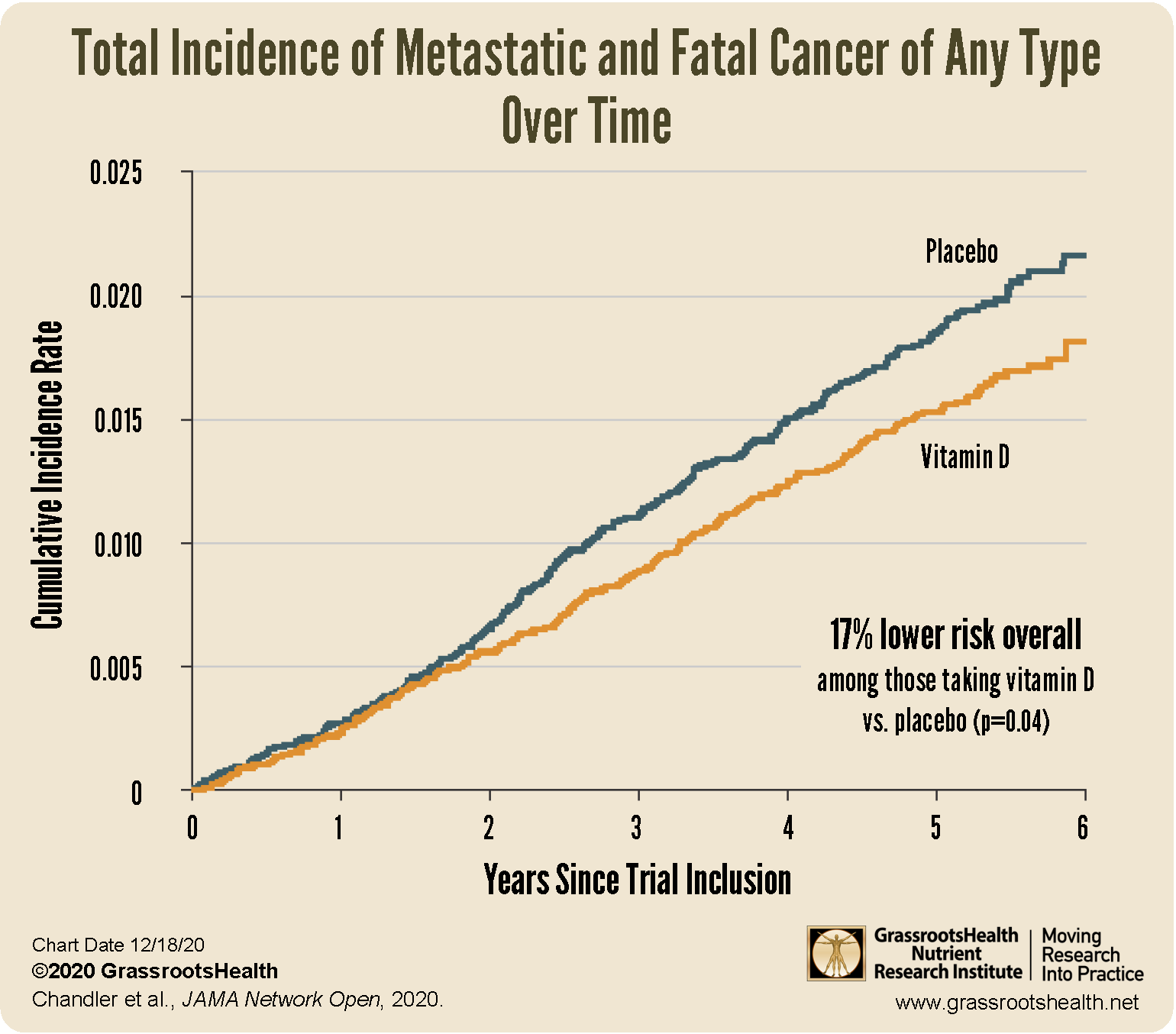
A total of 1,617 participants were diagnosed with invasive cancer, with an average follow up time of 5.3 years. Supplementation with vitamin D did reduce the incidence of metastatic or fatal cancer in the overall cohort. Of those diagnosed, 226 (1.7%) had been receiving vitamin D and 274 (2.1%) had been receiving a placebo. Overall, there was a 17% reduced risk of metastatic or fatal cancer among the vitamin D group versus the placebo group (p=0.02).
When taking BMI into consideration the reduction in cancer was more pronounced. A significant reduction of metastatic or fatal cancer was seen among those with a normal BMI, with a decreased risk of 38% among those taking vitamin D compared to placebo (p=0.004); the findings were non-significant among those who were overweight or obese. In other words, the greatest risk reduction was seen among those with the lowest BMI.
Why is BMI Important to Consider with Vitamin D Research?
Evidence shows that vitamin D levels are greatly affected by obesity. The more fat a person has on their body (the higher the BMI), the more likely they are to have vitamin D deficiency, and their need for vitamin D increases. This is one reason suggesting the same daily intake of vitamin D for all adults simply does not make sense. In fact, the amount of vitamin D needed on a daily basis to achieve a vitamin D level of 40 ng/ml (100 nmol/L) can vary by as much as 3 times the amount, depending on BMI.
In the VITAL trial, vitamin D levels varied significantly by BMI at baseline and after one year of supplementation, and participants in the vitamin D group received only 2,000 IU per day. In participants with a normal BMI (25 to 30) average vitamin D levels increased from 29.5 ng/ml at baseline to 41.4 ng/ml at follow-up – meaning that only half of the participants achieved levels above 40 ng/ml (100 nmol/L) with 2,000 IU of vitamin D supplementation. In comparison, in those who were overweight (BMI above 30), average vitamin D levels did not reach 40 ng/ml, only increasing from 26.7 ng/ml at baseline to 38.6 ng/ml at one year.
Making Conclusions Based on Vitamin D Level, Not Intake
Due to the large range of variability in the response to a particular dose, vitamin D testing should be used to personalize the intake amount. Therefore, the above conclusion leaves us to ponder, since BMI is a major factor affecting the dose response of vitamin D, what would an analysis by vitamin D level instead of intake have shown us?
While the conclusions from the VITAL study based on intake are promising, the optimal methodology for making such conclusions would have been to look at the results based on vitamin D levels at the start of the study and after supplementation. This would show what effect supplementation had on the serum level, and if it raised the level enough to make a difference for the outcome being measured. This is just one of the guidelines from Dr. Robert Heaney’s Guidelines for optimizing design and analysis of clinical studies of nutrient effects.
Since many factors affect the dose response to supplementation (including BMI and various co-nutrients such as magnesium), testing is absolutely essential. Without this information, it is difficult to make a solid conclusion about the effect of vitamin D on any particular health outcome.
Additional Vitamin D Outcomes Among Women with Breast Cancer
Research demonstrates that it is not too late to affect breast cancer outcomes with vitamin D, even after a diagnosis.
- Yao et al. (2021) found a 27% Lower Risk of Breast Cancer Death, a 21% Lower Risk of Recurrence-Free Death, and an 18% Lower Risk of Invasive Disease-Free Death with Vitamin D Levels of 30 ng/ml vs. 20 ng/ml or Lower at the Time of Diagnosis
- Madden et al. (2018) found a 49% Lower Risk of Breast Cancer Death with Vitamin D Supplementation Initiated within 6 Months of Diagnosis
- Mohr et al. (2014) found a 44% Lower Risk of Breast Cancer Related Death with Vitamin D Levels of 30 ng/ml vs.17 ng/ml among Breast Cancer Patients…
…in fact, the vitamin D level accounted for 97% of the variance of the relationship between vitamin D level and breast cancer fatality (meaning it made almost all the difference)!
Omega-3s, Magnesium, Selenium, and Vitamin C are Among Other Nutrients That Can Affect Breast Cancer Risk and Outcomes
Other nutrients are also important for reducing risk of breast cancer and improving outcomes among women who get breast cancer. Studies have shown
- an approximately 40% lower breast cancer risk with higher omega-3 intake (Zheng et al. 2013)
- 40% lower breast cancer risk among women with a higher magnesium intake vs a lower magnesium intake (Huang et al. 2019)
- 58% lower risk of breast cancer death with higher levels of selenium (Demircan et al. 2021)
- 15% lower breast cancer mortality with vitamin C (Harris et al. 2014)
Don’t Blindly Supplement – Test Your Nutrient Levels Today!
 Based on the findings presented above, measuring your levels of vitamin D, magnesium, selenium, and omega-3s may help determine if more of these nutrients might be needed to provide the greatest risk reduction for breast cancer and improve outcomes in the case of a breast cancer diagnosis.
Based on the findings presented above, measuring your levels of vitamin D, magnesium, selenium, and omega-3s may help determine if more of these nutrients might be needed to provide the greatest risk reduction for breast cancer and improve outcomes in the case of a breast cancer diagnosis.
Create your custom home blood spot kit with the following measurements to help determine if you are getting enough of the following nutrients shown to benefit your current or future breast health:
- Vitamin D
- Omega-3 Index
- Magnesium PLUS Elements
- Add hsCRP as a marker of inflammation
Having and maintaining healthy vitamin D levels and other nutrient levels can help improve your health now and for the future. Enroll and test your levels today, learn what steps to take to improve your status of vitamin D (see below) and other nutrients and blood markers, and take action! By enrolling in the GrassrootsHealth projects, you are not only contributing valuable information to everyone, you are also gaining knowledge about how you could improve your own health through measuring and tracking your nutrient status, and educating yourself on how to improve it.