Published on February 13, 2023
What can you do to address inflammation and immune dysregulation? Use this 10% Off Offer to help manage inflammation and boost your immune system
Key Points
- An estimated 10-30% of people who have been infected with SARS-CoV-2 experience symptoms of Long COVID, which affects multiple organ systems and often includes brain fog, shortness of breath, and chronic fatigue; Long COVID has also been shown to increase the risk of worsening existing health problems and inducing new onset conditions
- A new review lists the main contributors to Long COVID as inflammation, autoimmunity, and immune dysregulation; in fact, high levels of multiple autoantibodies that target different tissues and organ systems have been found in patients with COVID-19 and Long COVID
- Several markers could be measured and optimized to address potential underlying factors contributing to ongoing inflammation and immune dysregulation; several of these markers are included in the Inflammation Panel test kit, which measures levels of vitamin D, omega-3s (including the AA:EPA Ratio), C-reactive protein, and Hemoglobin A1c (HbA1c)

The World Health Organization (WHO) has defined Long COVID as “a condition that occurs in individuals with a history of probable or confirmed SARS-CoV-2 infection, usually 3 months from the onset of COVID-19 with symptoms that last for at least 2 months and cannot be explained by an alternative diagnosis.” An estimated 10-30% of people who have been infected with SARS-CoV-2 experience symptoms of Long COVID. The highest percentage of cases occur in individuals between 36 and 50 years of age who experienced mild COVID-19 symptoms during their acute phase.
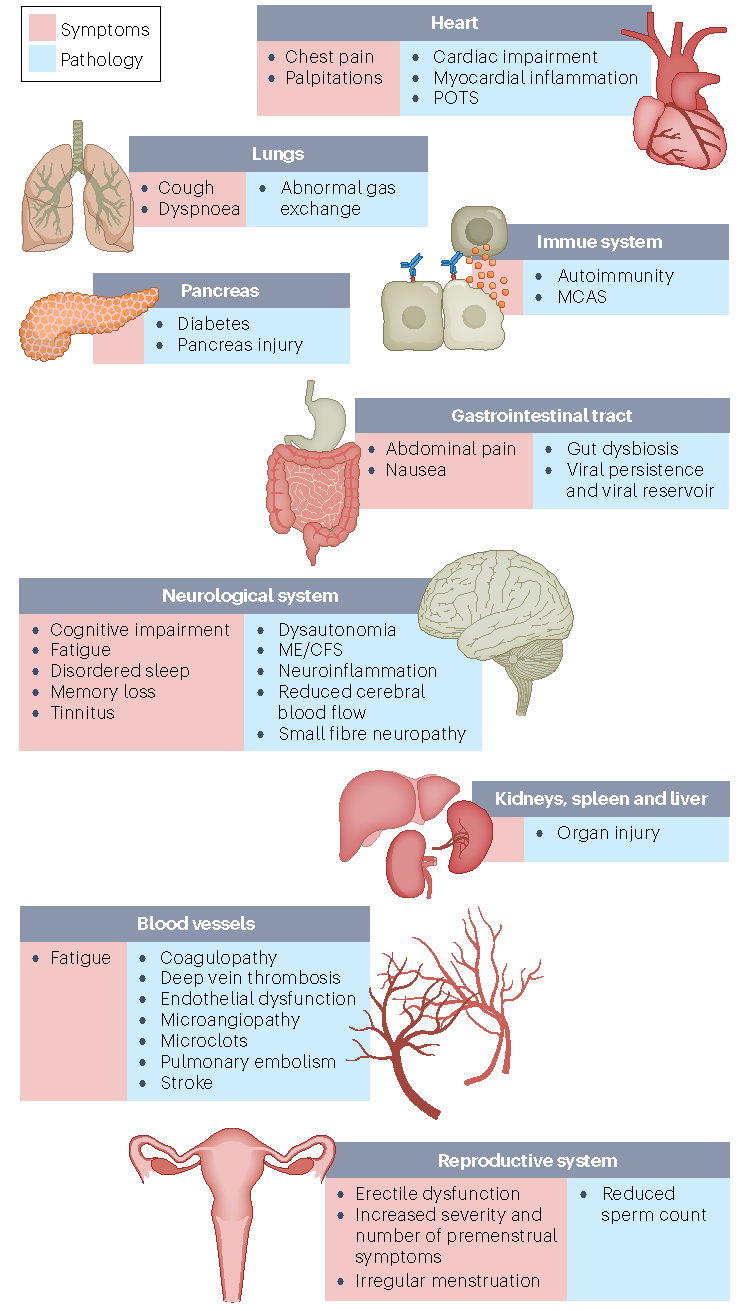
The symptoms of Long COVID affect multiple organ systems and often include brain fog, shortness of breath, and chronic fatigue. Long COVID has also been shown to increase the risk of worsening existing health problems, and inducing new onset conditions, including type 2 diabetes, cardiovascular and cerebrovascular disease, and dysautonomia [especially postural orthostatic tachycardia syndrome (POTS)].
The diagram below by Davis et al. illustrates the many ways Long COVID can affect multiple systems within the body.
Review Investigates Top Contributors to Long COVID
A review by Davis et al. lists the main contributors to Long COVID as inflammation, autoimmunity, and immune dysregulation. Other possibilities include an inability of the body to clear the virus from the tissues, blood clotting with endothelial dysfunction, imbalance of the gut microbiome, and re-activated viruses (including Epstein-Barr and human herpesvirus 6). High levels of multiple autoantibodies that target different tissues and organ systems have been found in patients with COVID-19 and Long COVID, indicating an autoimmune component as well.
As the authors state,
“The damage that has been demonstrated across diverse tissues has predominantly been attributed to immune-mediated response and inflammation, rather than direct infection of cells by the virus.”
What Can be Done to Address Inflammation and Immune Dysregulation?
While diet and lifestyle changes, such as increasing exercise, losing weight, and quitting smoking, can help lower inflammation levels and improve immune function, there are several markers that could be measured and optimized in order to address potential underlying factors contributing to ongoing inflammation and immune dysregulation. Several of these markers are included in the Inflammation Panel test kit, which measures levels of vitamin D, omega-3s (including the AA:EPA Ratio), C-reactive protein, and Hemoglobin A1c (HbA1c). Measure these markers now – get 10% Off the Inflammation Panel test kit during the month of February, 2023!
Vitamin D
Vitamin D has demonstrated anti-infective, anti-inflammatory, and immunomodulatory properties, and it has been shown to reduce the risk of autoimmune disease. Multiple studies have linked vitamin D deficiency to increased severity and death due to COVID-19; it is known to affect the immune response in several important ways, specifically against viral infections. One of the most important ways vitamin D helps protect against COVID-19 is through its role in modulating inflammation and preventing the cytokine storm, which could also be a reason vitamin D has been shown to help prevent chronic diseases such as diabetes. Vitamin D works directly on the cells of the immune system, and many of these cells also produce their own vitamin D by expressing vitamin D converting enzymes to manufacture site-specific 25(OH)D and 1,25D.
Evidence points to a minimum 25(OH)D level of 40 ng/ml (100 nmol/L) to fully optimize these demonstrated anti-inflammatory and immune regulating properties of vitamin D.
Balancing Omega-3s and Omega-6s
Omega-3 and omega-6 fatty acids are poly-unsaturated fatty acids (PUFAs) that work together to directly regulate inflammation, immune function, and pain. Eicosapentaenoic acid (EPA) and eocosahexaenoic acid (DHA) are the two main omega-3 fatty acids, while the most common omega-6 fatty acid is linoleic acid (LA), which is converted into longer omega-6 fats such as arachidonic acid (AA). Omega-6s (such as AA) are pro-inflammatory, essential for initiating and sustaining the inflammatory response – a physiologic function necessary for healing from injuries and infection. Omega-3s (such as DHA and EPA) are anti-inflammatory and promote the resolution of the inflammatory process. More specifically, AA plays an important role in the initiation of acute inflammation, which then becomes moderated by the involvement of omega-3s (EPA and DHA) as they replace AA, and with the help of vitamin D, begin to resolve inflammation.
The AA:EPA ratio is a measure of the primary pro/anti-inflammatory fatty acids. Higher levels of AA lead to a higher AA:EPA ratio, promoting inflammation and the development of chronic disease. Higher levels of EPA can help lower the AA:EPA ratio and reduce inflammation. AA is found in cooking oils, processed foods, and animal products, while EPA is found in seafood (primarily fatty fish) and most marine-based omega-3 supplements. To lower the AA:EPA ratio, and therefore, lower inflammation, increasing EPA rich foods and/or supplements while decreasing AA rich foods is often the best route to getting this marker into its target range.
Some experts consider the desirable range for the AA:EPA ratio to be 2.5 to 11; others consider a range or 1.5 to 3 to be low risk, 3 to 6 to be moderate risk, 7-15 to be elevated risk, and above 15 to be high risk. Knowing your AA:EPA ratio can help you take more specific steps to achieve an ideal ratio through diet and supplements.
High Sensitivity C-Reactive Protein (hs-CRP)
C-reactive protein (CRP) is a protein produced by the liver in response to a very broad range of causes, such as infection from hepatitis to cancer, and is used as a general marker of inflammation. Elevated CRP levels have been linked to future heart attacks, stroke, peripheral arterial disease, metabolic syndrome, the development of diabetes, and many other chronic diseases.
The CRP test blood spot test offered by GrassrootsHealth uses a high sensitivity assay, hs-CRP where “hs” means high sensitivity, to detect small elevations in CRP.
Evidence suggests that levels below 1.0 mg/L indicate low inflammation and low risk of cardiovascular disease, levels between 1.0 and 3.0 mg/L indicate average risk, and levels between 3.1 and 10 mg/L indicate increased risk (levels above 10 mg/L most likely indicate an acute infection or injury).
Hemoglobin A1c Test (HbA1c)
HbA1c is a measure of how healthy average blood sugar levels have been in the recent few months, and is a better representation of blood sugar health than a single glucose measurement, since glucose levels vary throughout the day. HbA1c is the compound formed in the blood when a hemoglobin molecule in a red blood cell binds with a glucose molecule in the blood; the resulting molecule is also known as glycated hemoglobin. It can be a good indicator of glucose intolerance even in the absence of abnormal fasting glucose levels, and higher levels of HbA1c are associated with increased levels of inflammation in the body.
A healthy A1c level is less than 5.7%, while greater than 6.5% indicates diabetes, and between 5.7-6.5% represents prediabetes (see this post for special circumstances).
Magnesium and Long COVID
Multiple studies have observed associations between low magnesium intake and levels, and increased levels of inflammation and oxidative stress. A new study has shown the relationship between serum magnesium levels and the onset of Long COVID. This study found a 114% increased risk of Long COVID among participants whose serum magnesium levels were at or below 1.96 mg/dL at the beginning of their COVID-19 disease, compared to those magnesium levels were higher.
Consider adding the magnesium blood spot test to the inflammation panel tests above to see what your current magnesium status is, by creating your custom test kit here.
Take Steps to Lower Your Levels of Inflammation & Improve Immune Function
 Having and maintaining healthy vitamin D levels and other nutrient levels can help improve your health now and for your future. Choose which additional nutrients to measure, such as your omega-3s and essential minerals including magnesium and zinc, by creating your custom home test kit today. Take steps to improve the status of each of these measurements to benefit your overall health. With measurement you can then determine how much is needed and steps to achieve your goals. You can also track your own intakes, symptoms and results to see what works best for YOU.
Having and maintaining healthy vitamin D levels and other nutrient levels can help improve your health now and for your future. Choose which additional nutrients to measure, such as your omega-3s and essential minerals including magnesium and zinc, by creating your custom home test kit today. Take steps to improve the status of each of these measurements to benefit your overall health. With measurement you can then determine how much is needed and steps to achieve your goals. You can also track your own intakes, symptoms and results to see what works best for YOU.
Enroll in D*action and Test Your Levels Today!