Published on October 8, 2021
A higher BMI increases the risk of both cancer and severe COVID-19 disease; could a higher risk of vitamin D deficiency be an underlying contributor for both?
Key Points
- A secondary analysis of the VITAL study found a significant 38% reduction of metastatic or fatal cancer among those with a normal BMI taking vitamin D compared to placebo; the findings were non-significant among those with higher BMIs, who were overweight or obese
- Obesity is also a known risk factor for increased risk of COVID-19 disease severity and death
- The more fat a person has on their body (the higher the BMI), the more likely they are to have vitamin D deficiency, and their need for vitamin D increases; in other words, obesity is a significant risk factor for vitamin D deficiency
- Due to the large range of variability in the response to a particular dose of vitamin D supplementation, vitamin D levels (not supplement amount) should be used to determine relationships in outcomes in research, as well as individualized supplementation amounts
 October is Breast Cancer Awareness Month (or Breast Cancer Prevention Month, as we say here at GrassrootsHealth), and this year, the focus on breast cancer continues to have to compete with that of COVID-19.
October is Breast Cancer Awareness Month (or Breast Cancer Prevention Month, as we say here at GrassrootsHealth), and this year, the focus on breast cancer continues to have to compete with that of COVID-19.
Both cancer and COVID-19 share obesity as a major risk factor, however, and there is one thing in particular that ties all three together: vitamin D.
Vitamin D Supplementation of 2000 IU/day Decreased Risk of Advanced Cancer, But Only with Normal BMI
The video below summarizes findings from Chandler et al., which were based on a secondary analysis of the VITAL randomized clinical trial data. The purpose of this analysis was to determine the effect of daily 2,000 IU vitamin D supplementation on the development of advanced, metastatic cancer and cancer death with BMI (grouped as below 25, 25 to under 30, and above 30) included to see if it modified the effects of supplementation. Initial findings from the VITAL trial were published in November of 2018; one paper compared cancer outcomes between those assigned to vitamin D (2000 IU/day) vs. placebo. When cancer outcome results were analyzed excluding the first two years after study initiation (allowing time for vitamin D to have an effect), there was a 25% reduced risk of cancer mortality among those taking vitamin D (p=0.02). However, the paper concluded that there was only a possible reduction in fatal cancer with vitamin D supplementation, noting a potential effect modification by body mass index (BMI).
VIDEO: Can Vitamin D Supplements Prevent Cancer? | Doctor’s Good News Ep 1
When taking BMI into consideration, the reduction in cancer was more pronounced. A significant reduction of metastatic or fatal cancer was seen among those with a normal BMI, with a decreased risk of 38% among those taking vitamin D compared to placebo (p=0.004); the findings were non-significant among those who were overweight or obese. In other words, the greatest risk reduction was seen among those with the lowest BMI. Could it have been that 2000 IU/day of vitamin D was not enough to make a big enough difference in vitamin D status for those with higher BMIs?
Both Obesity and Vitamin D Deficiency are Risk Factors for Severe COVID-19
Another video recently released, titled REPORT: 9 out of 10 CHILDREN with COVID in ICU had THIS health condition…, reviews findings from North Carolina discussing the correlation between obesity and COVID-19 severity among children hospitalized with COVID-19. These findings are similar to others showing both vitamin D deficiency and obesity as risk factors for severe COVID-19 among adults.
Why Does BMI Matter with Cancer Research, COVID-19 Disease, and Vitamin D?
Vitamin D has known anticancer effects, and much research has been published over the last several decades showing a link between vitamin D levels and cancer risk. Decades of research have also identified vitamin D as a vital component to a healthy immune system.
Evidence also shows that vitamin D levels are greatly affected by obesity. The more fat a person has on their body (the higher the BMI), the more likely they are to have vitamin D deficiency, and their need for vitamin D increases. This is one reason suggesting the same daily intake of vitamin D for all adults simply does not make sense. In fact, the amount of vitamin D needed on a daily basis to achieve a vitamin D level of 40 ng/ml (100 nmol/L) can vary by as much as 3 times the amount, depending on BMI.
Vitamin D Levels Above 40 ng/ml Associated with Lower COVID-19 Mortality
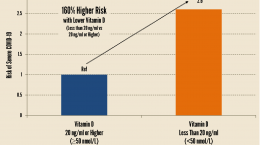
The authors of another paper looking at risk factors for COVID-19 disease severity and death analyzed their data based on vitamin D blood levels of at least 40 ng/ml (GrassrootsHealth’s Scientists’ Panel recommends a level between 40-60 ng/ml (100-150 nmol/L)). Although there were not enough patients for a full analysis based on this classification, they found that of those over 40 years old with vitamin D blood levels less than 30 ng/ml, 20% died from COVID-19, whereas in those with blood levels of at least 30 ng/ml, 9.7% died, and in those with vitamin D levels of at least 40 ng/ml, 6.3% died.
The study authors state that a blood level of at least 40 ng/ml may be optimal for vitamin D’s immunomodulatory effect. Do you know what your current vitamin D level is? Test today to find out!
Making Conclusions Based on Vitamin D Level, Not Intake
Due to the large range of variability in the response to a particular dose of vitamin D supplementation, vitamin D testing should be used to personalize the intake amount. Therefore, many published conclusions on outcomes based on vitamin D intake leave us to ponder, since BMI and other factors have such a major effect on the dose response of vitamin D, what would an analysis by vitamin D level instead of intake have shown us?
While the conclusions from the VITAL study reviewed above based on intake are promising, the optimal methodology for making such conclusions would have been to look at the results based on vitamin D levels at the start of the study and after supplementation. This would show what effect supplementation had on the serum level, and if it raised the level enough to make a difference for the outcome being measured.
Don’t Blindly Supplement – Test Your Vitamin D Level Today!
 Having and maintaining healthy vitamin D levels and other nutrient levels can help improve your health now and for your future. Choose which to measure, such as your vitamin D, omega-3s, and essential minerals including magnesium and zinc, by creating your custom home test kit today. Take steps to improve the status of each of these measurements to benefit your overall health. You can also track your own intakes, symptoms and results to see what works best for YOU.
Having and maintaining healthy vitamin D levels and other nutrient levels can help improve your health now and for your future. Choose which to measure, such as your vitamin D, omega-3s, and essential minerals including magnesium and zinc, by creating your custom home test kit today. Take steps to improve the status of each of these measurements to benefit your overall health. You can also track your own intakes, symptoms and results to see what works best for YOU.
Enroll and test your levels today, learn what steps to take to improve your status of vitamin D (see below) and other nutrients and blood markers, and take action! By enrolling in the GrassrootsHealth projects, you are not only contributing valuable information to everyone, you are also gaining knowledge about how you could improve your own health through measuring and tracking your nutrient status, and educating yourself on how to improve it.
Help everyone Move Research into Practice with vitamin D and other nutrients! As a special birthday gift to everyone, in honor of the science, we have created a special scholarship fund for anyone to donate to that will go towards helping others participate. Your donation will allow anyone to get help with funding their participation when they need it.
Text-to-give: Text Daction to 44321 to add to our Scholarship Fund.