Published on November 22, 2023
Prof. Sunil Wimalawansa elaborates on calculating the correct amount of vitamin D to take and when certain forms of supplementation should be considered (Interview Series Part 4)
A 5-Part Interview Series with Dr. Sunil Wimalawansa
Part 1 Vitamin D: Everything You Need to Know… and More: An introduction to Dr. Wimalawansa along with details focusing on his experience with vitamin D in the clinical and scientific setting
Part 2 Defining Optimal Levels and Doses of Vitamin D for Every Individual: Answers to questions about optimal vitamin D levels and doses and how they may differ for certain individuals
Part 3 Understanding the Forms of Vitamin D: Vitamin D3, 25(OH)D, and 1,25(OH)2D:A detailed description of the forms vitamin D3, 25(OH)D, and 1,25(OH)2D and when each might be considered for measurement
Part 4 How Does One Determine the Right Amount and Type of Vitamin D to Take?: Calculating the correct amount of vitamin D to take and when certain forms of supplementation should be considered
Part 5 Vitamin D Safety and Adverse Effects – When Should Caution Be Advised?: Our final post for this series of questions-and-answers with Dr. Wimalawansa on vitamin D safety and toxicity
Key Points (Part 4)
- Administration of the proper doses daily or weekly will significantly reduce disease and hospital burdens, healthcare costs, loss of productivity, and absenteeism
- Because of the rapidity of action, the use of calcifediol is indicated in emergencies, such as acute infections (e.g., SARS-CoV-2), sepsis, and ICU setups, and is also indicated in liver failure [i.e., when there is a reduced capacity of hepatocytes to produce 25(OH)D] and in “severe” fat malabsorption syndromes, including following gastric bypass surgery
- Irrespective of any loading dose used, one must start an appropriate daily maintenance dose to maintain serum 25(OH)D concentrations above 50 ng/mL within a couple of weeks
- Calcitriol is indicated in renal failure to prevent secondary and tertiary hyperparathyroidism and to maintain serum-ionized calcium concentration within the physiological range; it is not indicated for use in infections, and if high doses of calcitriol are used, it will be associated with severe adverse effects
 Dr. Sunil Wimalawansa has been researching vitamin D for over four decades and is considered one of the world’s leading experts on micronutrients, especially vitamin D. His extensive background includes working with vitamin D in the laboratory setting, applying his vitamin D knowledge, working with patients as a medical doctor, and directing clinical trials involving vitamin D.
Dr. Sunil Wimalawansa has been researching vitamin D for over four decades and is considered one of the world’s leading experts on micronutrients, especially vitamin D. His extensive background includes working with vitamin D in the laboratory setting, applying his vitamin D knowledge, working with patients as a medical doctor, and directing clinical trials involving vitamin D.
We introduced Dr. Wimalawansa in Part 1 of this interview series, Vitamin D: Everything You Need to Know… and More, and shared his answers to questions about optimal vitamin D levels and doses and how they may differ for certain individuals in Part 2, Defining Optimal Levels and Doses of Vitamin D for Every Individual, followed by a detailed description of the forms vitamin D3, 25(OH)D, and 1,25(OH)2D and when each might be considered for measurement and/or supplementation in Part 3, Understanding the Forms of Vitamin D: Vitamin D3, 25(OH)D, and 1,25(OH)2D.
Today’s post will review questions and answers with Dr. Wimalawansa on how to supplement with vitamin D (doses and timing) and what forms of vitamin D should be considered during specific circumstances.
Note: Vitamin D2 (ergocalciferol) will not be discussed, as it is a synthetic (non-human) product that is derived from plant precursors that is not utilized by the body as efficiently as vitamin D3. With a much shorter half-life, it remains in the blood for only a few hours. Supplementation with vitamin D3 is recommended.
Questions and Answers with Dr. Sunil Wimalawansa: Vitamin D Dosing and Supplement Forms
Can you tell us how an individual can determine the most helpful amount or what vitamin D dose you recommend that applies to a broader population?
Vitamin D threshold and the minimal necessary levels do not change between people or disease status. Calculating the proper amounts of vitamin D dose for individuals should be based on either the serum 25(OH)D concentration (if known but not essential), BMI, or body weight (DOI: 10.3390/nu14142997). Based on the principles discussed previously, we published the simplified version of “vitamin D dose calculation” for individuals that applies to all body weight groups (DOI: 10.3390/nu14142997; 10.3390/nu15173842):
I. Not obese (average wt.: BMI ≤ 29): 70-90 IU/kg BW
II. Moderately obese (BMI 30-39): 100-130 IU/kg BW
III. Morbid obesity (BMI ≥ 40): 140-180 IU/kg BW
Note: All current vitamin D guidelines are based on outdated and some false concepts and research methodologies published 30+ years ago—(Results from the first randomized controlled trials on vitamin D and cancer – GrassrootsHealth). As described above, raising the minimum and upper limit of serum 25(OH)D concentrations to 50 and 80 ng/mL (125 to 200 nmol/L) and the safe upper limit of intake from the current 10,000 to 15,000 IU/day is indicated based on more recent data is essential. The average daily vitamin D intake for a non-obese 70 kg adult to maintain serum 25(OH)D levels between 50 and 80 ng/mL is 5,000 IU (up to 7,000 IU for a person with 90 mg body weight). Three straightforward suggestions are mentioned above; the needed amount of vitamin D can be easily calculated using an individual’s body weight or BMI.
Administration of the proper doses daily or weekly will significantly reduce disease and hospital burdens, healthcare costs, loss of productivity, and absenteeism. Daily intakes of vitamin D exceeding 7,000 IU or 50,000 IU/ once a week and above in a non-obese 70 kg person will increase the serum 25(OH)D to the range between 60 and 90 ng/mL. For those who maintain their serum 25(OH)D concentrations at those levels or above, it is advisable to also take vitamin K2 (MK-7).
GrassrootsHealth has also created a Vitamin D*calculator in which an individual can enter their current 25(OH)D level (if known), their weight, and their desired 25(OH)D level. The calculation provides two options for increasing your vitamin D levels – a “Loading Dose” (divided into doses of 25,000 IU over several days) and a “Maintenance Dose” (capped at 10,000 IU per day), allowing users to choose how quickly they would like to achieve their desired levels. The vitamin D* calculator can also suggest a daily vitamin D intake for individuals who enter only their weight and target 25(OH)D level. This calculation is an estimate based on the average intake required for people of the same body weight.
Which is better – taking vitamin D daily, once a week, or other?
Humans are supposed to generate most of the “daily vitamin D3 requirement” from UVB rays from sunlight. Daily sun exposure or supplementation keeps the circulatory levels of D3 and 25(OH)D stable. Physiologically, this is important, as D3 and 25(OH)D enter peripheral target tissues like immune and breast cells to generate the non-hormonal form of calcitriol that has a variety of physiological functions. This is especially important during pregnancy and for breastfeeding mothers, as it is predominantly vitamin D that enters the placenta and breastmilk. A daily intake of around 6,000 IU vitamin D has been shown to provide the breastfeeding infant with 400-500 IU per day of vitamin D; maintaining a target 25(OH)D serum level (such as with weekly or longer dosing) is less effective. (DOI: 10.1210/jc.2013-2653). Considering the short half-life of D3, “daily consumption” or sun exposure is the best option compared to taking it once a week or less frequently.
The main advantage of weekly vitamin D consumption is that it is easier to remember to take, improving adherence to therapy. There are many medications where a weekly schedule improves compliance (adherence to the therapy) compared to daily. However, generally, there is no clinical rationale or value for taking vitamin D less frequently than once a month or taking vitamin D metabolites (or analogs) as “vitamin D supplements.”
Could calcifediol be superior to D3 as a vitamin D supplement? The answer is NO.
 As we discussed, vitamin D is partially activated in the liver to form calcifediol [25-hydroxyvitamin D; 25(OH)D]), the primary circulating form. It is the most abundant vitamin D metabolite in the circulation and a measure to assess “vitamin D status.” While vitamin D is an over-the-counter nutrient supplement, calcifediol is a prescription medication in most countries that is expensive and difficult to obtain. The reported toxicity of calcifediol is higher than D3 (DOI: 10.1007/s00394-023-03103-1).
As we discussed, vitamin D is partially activated in the liver to form calcifediol [25-hydroxyvitamin D; 25(OH)D]), the primary circulating form. It is the most abundant vitamin D metabolite in the circulation and a measure to assess “vitamin D status.” While vitamin D is an over-the-counter nutrient supplement, calcifediol is a prescription medication in most countries that is expensive and difficult to obtain. The reported toxicity of calcifediol is higher than D3 (DOI: 10.1007/s00394-023-03103-1).
Based on equivalent international units, calcifediol costs 10 to 20 times more than vitamin D3, and availability of that suitable for human consumption is limited (95% of the manufactured calcifediol globally is used in animal food). In a few countries, calcifediol is also available as a slow-release or long-acting form. They are even more expensive; neither preparation is justified as routine vitamin D replacement therapy. Their use is cost-prohibitive when an over-the-counter, cheaper alternative D3 is available. Calcifediol extended-release analogs have no advantage over standard calcifediol under regular clinical use, including for liver or renal failure. When the cost of calcifediol is reduced by more than the-fold and becomes available over the counter in the future, it could become comparable to D3. It is inappropriate to prescribe calcifediol (or calcitriol) as a vitamin D supplement to correct hypovitaminosis D—e.g., for otherwise healthy people.
At what point might (or are there any conditions in which) a practitioner might supplement with oral calcifediol instead of vitamin D3?
Using calcifediol instead of vitamin D3 as a routine daily or weekly replacement therapy is not cost-effective as a replacement therapy for vitamin D deficiency or osteoporosis (and not recommended). While it has been suggested for use in renal failure, especially when liver functions are normal, there is no significant advantage (i.e., D3 is converted sufficiently into calcifediol in the liver), but it unnecessarily incurs additional costs. That push and marketing calcifediol for broader usage or as an alternative to vitamin D supplements primarily do so for commercial reasons.
The practical difference between vitamin D and calcifediol is the rapidity of raising serum 25(OH)D concentrations. The rising of serum 25(OH)D with calcifediol is linear and more predictable than cholecalciferol (D3), but it comes at a significantly higher cost (DOI: 10.1007/s00394-023-03103-1). Calcifediol raises blood levels of 25(OH)D within 4 hours, whereas vitamin D takes two to four days.
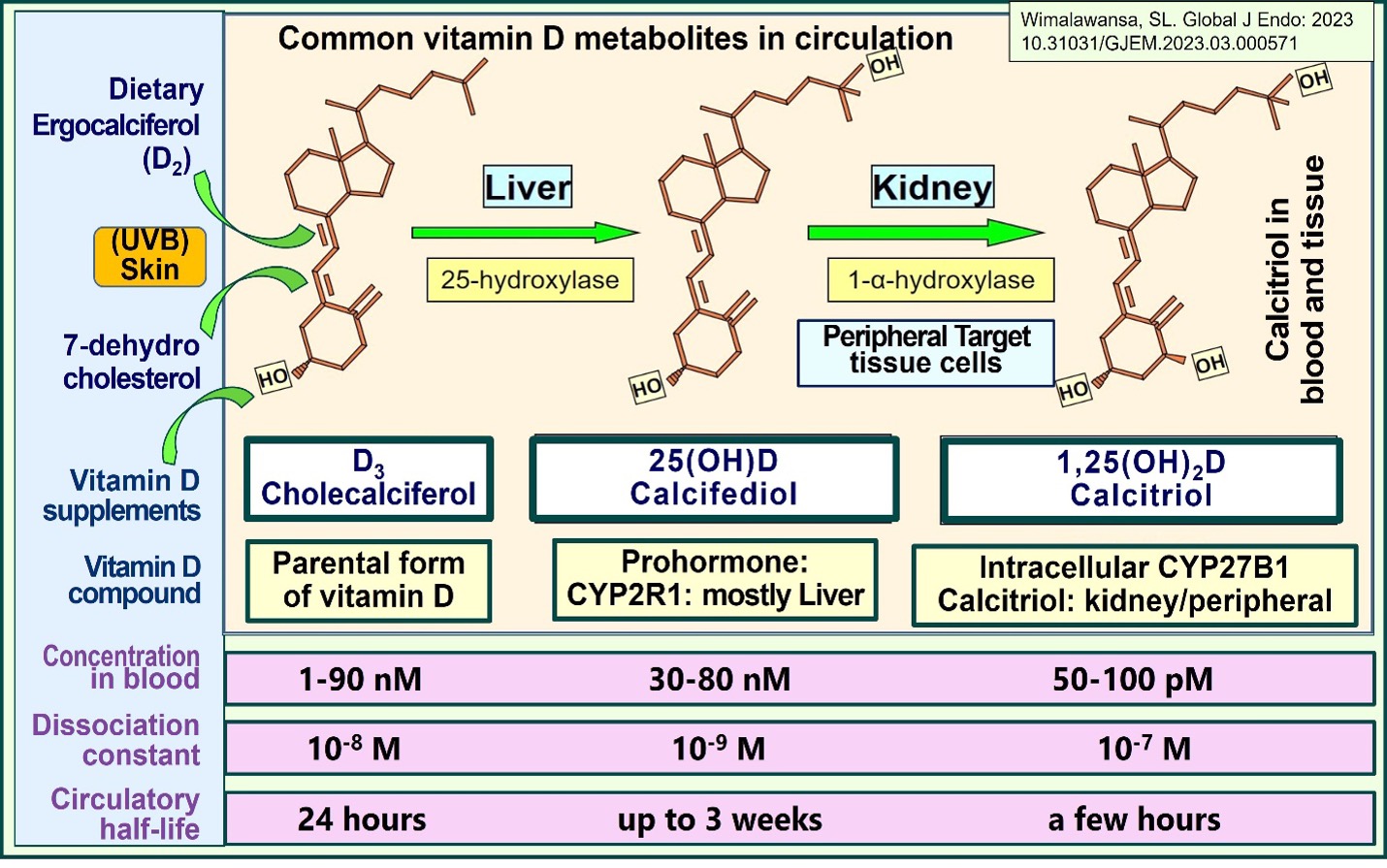
Because of the rapidity of action, calcifediol is indicated in emergencies, such as acute infections (e.g., SARS-CoV-2), sepsis, and ICU setups (DOI: 10.3390/nu14142997). Calcifediol is also indicated in liver failure [i.e., when there is a reduced capacity of hepatocytes to produce 25(OH)D] and in “severe” fat malabsorption syndromes (DOI: 10.1093/ajcn/nqab123), including following gastric bypass surgery. The following figure illustrates the differences between vitamin D3, calcifediol, and calcitriol (DOI: 10.31031/GJEM.2023.03.000571).
When using calcifediol, is it necessary to supplement with vitamin D3 simultaneously?
Great question. Calcifediol and vitamin D are not mutually exclusive and can be given simultaneously in emergencies, as in infections on admissions, which we strongly recommend (DOI: 10.3390/nu14142997). In emergencies, we recommend using a single dose of calcifediol 0.5 to 1 mg (calculated, 0.014 mg/kg body weight) for its immediate effects and a high dose of D3 for delayed raising and maintenance of serum 25(OH)D concentrations for prolonged benefits (DOI: 10.2147/PLMI.S373617). Alternatively, its longer half-life allows it to be used once or twice weekly as needed during the emergency period, such as during recovery from an infection.
What is your recommendation on the doses and frequency of administering calcifediol for healthcare practitioners?
In emergencies, calcifediol is administered as a single dose with high doses of vitamin D to maintain circulatory 25(OH)D for an extended period. Calcifediol can also be taken every third or fourth day during an emergency. Because of the high cost (and availability issues) and to get the best results, it is best to administer as a single oral dose, between 0.5 and 1.0 mg, at the first encounter with a patient who needs rapidly raising serum 25(OH)D concentration, as in acute infection. This will significantly expedite recovery with fewer complications and deaths (DOI: 10.2147/PLMI.S373617). The best option is to administer a single dose of calcifediol and a higher dose of vitamin D simultaneously, as early as possible: at first encounter or on admission to a hospital.
When calcifediol is unavailable in an emergency, administering a single bolus (upfront loading dose) of vitamin D between 100,000 and 400,000 IU should be considered. The amount depends on the circumstance and the patient’s body weight (DOI: 10.3390/nu14142997). Irrespective of the loading dose used, one must start an appropriate daily maintenance dose, as we discussed above, to maintain serum 25(OH)D concentrations above 50 ng/mL within a couple of weeks (usually at discharge from the hospital). The mechanisms, benefits, and indications for calcifediol are explained in detail in the following publications (DOI: 10.3390/biomedicines11061542; DOI: 10.2147/PLMI.S373617).
Are there specific indications for using calcifediol?
Yes, there are specific indications for using calcifediol. Despite being advertised by pharma and some physicians, calcifediol should not be used as a routine vitamin D supplement. This is due to its high cost, the lack of availability (thus, it should be reserved for emergencies), the need for a prescription, the potential high risk for adverse effects, and the unfamiliarity of most healthcare workers with its proper use. Calcifediol is indicated (A) when in the case of liver failure, where 25-hydroxylation of vitamin D is impaired, and (B) when there is a clinical reason (urgency) for a rapidly rising serum 25(OH)D concentration (i.e., acute infection). While it can be used in other circumstances, such usage is not cost-efficient.
The recommended dose of calcifediol is approximately 1.0 mg for a non-obese 70 kg adult and 0.5 mg for an adolescent (0.014 mg/kg body weight). For details on dose-calculations, please see Table 3: 10.3390/nu14142997.
Are there specific indications for using calcitriol?
As discussed, vitamin D metabolites (and analogs) are restricted to specific situations, such as calcifediol in hepatic failure and emergencies. In addition, calcifediol is used to rapidly raise serum 25(OH)D concentrations and maintain serum 25(OH)D concentrations in severe fat malabsorption syndromes, as with following Roux-en-Y Gastric bypass surgery.
Whereas calcitriol is indicated in renal failure to prevent secondary and tertiary hyperparathyroidism and to maintain serum-ionized calcium concentration (DOI: 10.4103/ijem.IJEM_292_19). Studies have confirmed that when vitamin D3 is co-administered with calcitriol, it improves the quality of life and longevity of those with chronic renal failure.
Even pharmacological doses of exogenous calcitriol generate too little circulatory blood concentration for it to enter immune cells. Therefore, calcitriol is not indicated in infections. If high doses of calcitriol are used, that will be associated with severe adverse effects but no tangible benefit. Understanding the mechanisms we discussed above and in recently published peer-reviewed papers allows proper selection and the use of vitamin D metabolites to save lives.
Why is there a lack of uniformity in the doses and serum 25(OH)D concentrations necessary to keep people healthy?
The answer to this question depends on whether a healthcare worker is considering treating a specific system in the body, like the musculoskeletal or cardiovascular system, or holistically. The latter would always make the body resilient and protect it from unexpected harmful events such as an injury, disease, or an infection like SARS-CoV-2, thus providing a broader cover.
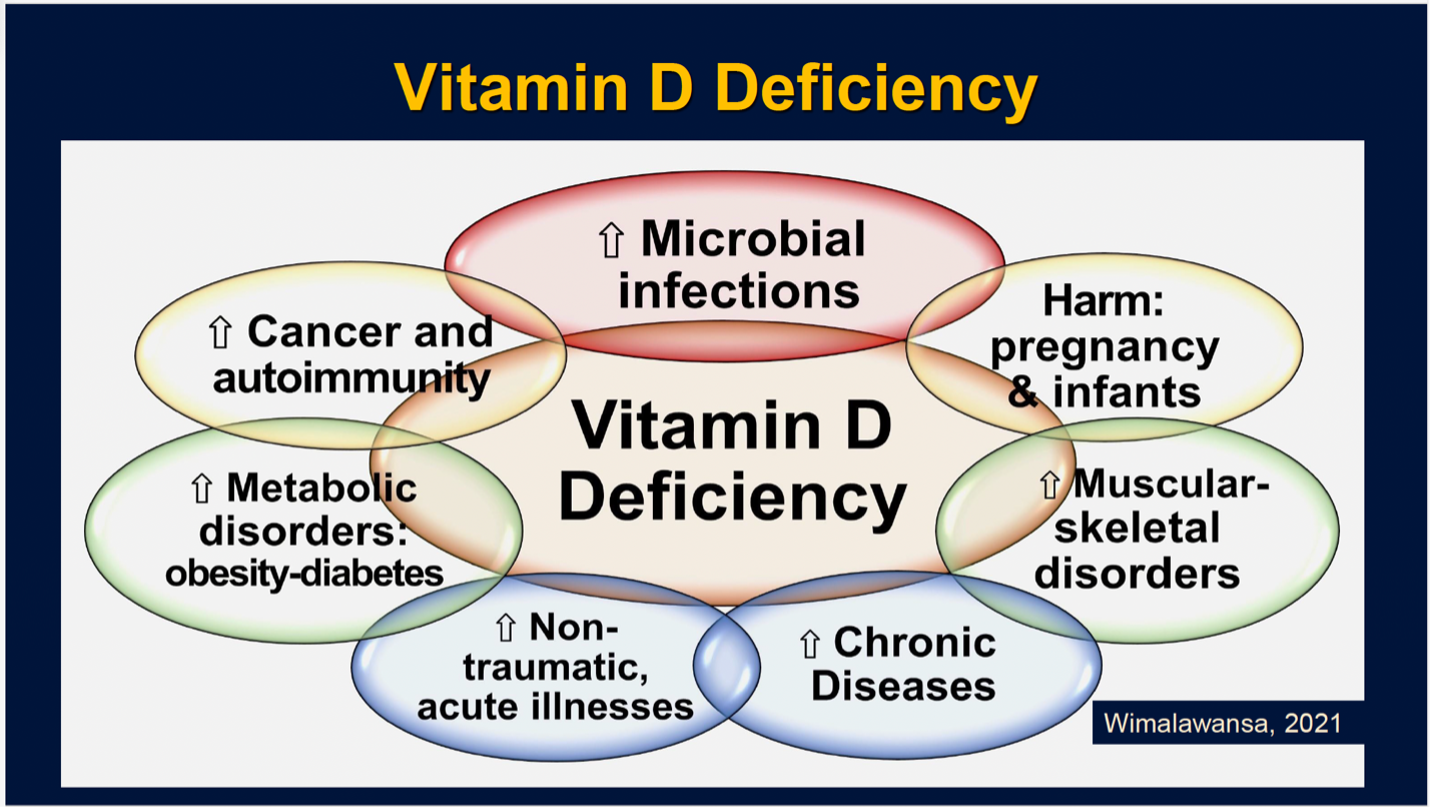
The following figure illustrates the consequences of vitamin D deficiency as it affects the whole body.
System-based therapy and medicine is a traditional compartmentalized medicine taught in all medical, osteopathic, and nursing schools. This is what almost all healthcare workers practice worldwide, propagated by their medical societies. Instead, with that basic knowledge, they should re-train and set their minds to holistic approaches, including (a) improving their listening capacity and (b) focusing on healing the whole patient, enriching their mind and the body.
We have the same issues regarding vitamin D. Healthcare workers are trained to work on system-based, compartmentalized thinking. Consequently, they focus on treating a part of the body or a system, not the entire patient as it should be. This learned habit of ignoring the whole person, dissociating the mind and the body connection, led scientists to design clinical trials based on one disease, a part of the body system, or a specific tissue. This deep-rooted subspeciality-based silo-mentality frequently manifests in study design as avoidable major errors. Such study data overlooks the entire person, thus leading to faulty or inferior clinical recommendations.
Is this due to ignorance or suppression of information?
The mentioned silo-mentality of scientists, medical specialists, and their scientific societies then publish contradictory guidelines with different recommendations for vitamin D doses. This has been varied from 400 IU to 4,000 IU/day for an adult and minimum effective serum 25(OH)D concentration, from 20 to 40 ng/mL, etc. This is not different from (or analogy) six blind persons describing the shape of an elephant by touching different parts of its body—i.e., for the individual disease or body system they are interested in, their proposed maximum levels might work, but not for the entire body. We need a minimal serum 25(OH)D level that overcomes all disorders affecting the body at 50 ng/mL.
Special interest groups and patient advocacy groups propagate these contradictory recommendations to favor their advantage and position, which worsens the confusion, preventing the progress of the vitamin D field (DOI: 10.1017/S0007114520002950). Consequently, big pharma and governments exploit this mass confusion and the lack of unity among scientists to their advantage. They support maintaining outdated vitamin D recommendations to sell their patented products at ten to hundred-fold higher prices. This keeps people unhealthy and requires more doctors’ visits, medications, and hospitalizations. Similar approaches have been used by big pharma, using their misinformation playbooks. (http://orthomolecular.org/resources/omns/v14n22.shtml)
Note: An independent vitamin D researcher from Australia (Robin Whittle) recently made the following comments:
“Everyone should follow Prof. Wimalawansa’s recommendation. Then, 99.5% would have their 25(OH)D levels above the critical lower limit of 50 ng/mL (125 nmol/L), which is crucial for proper immune system functions. With no vitamin D3 supplementation and no recent summertime-like UV-B skin exposure, most people have only between 20 to 50% of the 25(OH)D needed to be healthy and minimize complications from infection and sepsis. The government-recommended daily vitamin D3 supplementation, such as 0.02 mg (800 IU), has no beneficial effect on the immune system to overcome infections.
If everyone followed Prof. Wimalawansa’s advice, there would be no pandemic influenza or COVID-19 (now or in the future)—and minimize the epidemic of sepsis that kills eleven million annually worldwide (DOI: 10.1016/S0140-6736(19)32989-7). It will also minimize chronic diseases, like dementia, cognitive disorders, Kawasaki disease, and Multisystem Inflammatory Syndrome (MIS) in children and adults (DOI: 10.3390/nu15163623; DOI: 10.3390/nu15163623).”
* The above is a scientific discussion and should not be considered medical advice. Regarding clinical or personal issues, Prof. Wimalawansa advises readers to consult her/his physician.
Test to See if You Are Getting Enough Vitamin D and Other Important Nutrients
 Create your custom home test kit to measure your levels at home as part of the D*action project!
Create your custom home test kit to measure your levels at home as part of the D*action project!
With your kit you can measure your:
- Vitamin D
- Magnesium PLUS Essential and Toxic Elements
- Omega-3 Fatty Acids
- hsCRP
- HbA1c
- TSH
- Type 1 Diabetes Autoantibodies
Did you know that each of the above can be measured at home using a simple blood spot test? As part of our ongoing research project, you can order your home blood spot test kit to get your levels, followed by education and steps to take to help you reach your optimal target levels. Start by enrolling and ordering your kit to measure each of the above important markers, and make sure you are getting enough of each to support better mood and wellbeing!
Create your custom home test kit today. Take steps to improve the status of each of these measurements to benefit your overall health. With measurement you can then determine how much is needed and steps to achieve your goals. You can also track your own intakes, symptoms and results to see what works best for YOU.