Published on May 6, 2020
There are many studies that have shown the connection between breast cancer and vitamin D, starting with the epiphany of the Garland Brothers when they first drove across the country in 1974, and then moving into many research studies, including our very own Breast Cancer Prevention Project.
An 80% risk reduction for breast cancer?
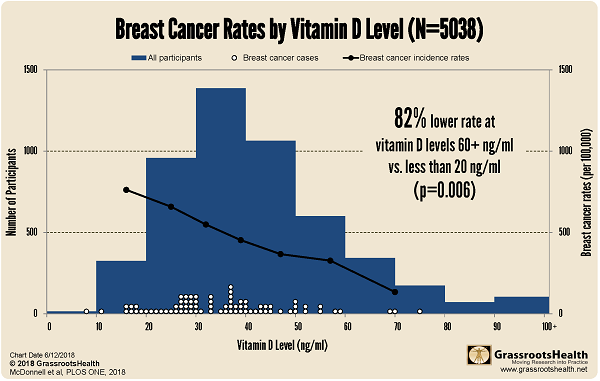
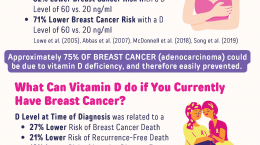
 This research paper, published in June 2018, combined the data from participants in two randomized controlled trials (RCT) and our Breast Cancer Prevention Project participants. The two RCTs were led by Dr. Joan Lappe, a member of our panel of scientists. Overall, an 80% reduction in the risk of breast cancer was observed among the women who reached a vitamin D level of at least 60 ng/ml (150 nmol/L) compared to those who had a vitamin D level of 20 ng/ml (50 nmol/L) or below.
This research paper, published in June 2018, combined the data from participants in two randomized controlled trials (RCT) and our Breast Cancer Prevention Project participants. The two RCTs were led by Dr. Joan Lappe, a member of our panel of scientists. Overall, an 80% reduction in the risk of breast cancer was observed among the women who reached a vitamin D level of at least 60 ng/ml (150 nmol/L) compared to those who had a vitamin D level of 20 ng/ml (50 nmol/L) or below.
The first RCT, focused on bone health and cancer, was published in 2007 and is summarized in our blog here. This study followed 1,179 healthy, postmenopausal women, aged 55 or older for four years and put them in one of three groups – taking a daily dose of 1,100 IU vitamin D and 1,400-1,500 mg calcium; calcium only; or placebo only. The study found that the vitamin D and calcium group had a 77% reduced risk of cancer as compared to the placebo group. When analyzing the same data by vitamin D level, it was found that participants with vitamin D levels equal to or above 40 ng/ml (100 nmol/L) had a 57% reduction in cancer risk, as compared to those with vitamin D levels below 20 ng/ml (50 nmol/L).
The second RCT focused solely on cancer. The 2,303 women enrolled in this study received either 2,000 IU/day of vitamin D and 1,500 mg/day of calcium or placebo. This study found a 30% reduction in cancer incidence with the vitamin D + calcium group, as compared to the placebo group. (paper here, blog here). Analyzed by serum level, the data showed that participants with a vitamin D level of 55 ng/ml (137 nmol/L) were 35% less likely to get cancer as compared to those with a vitamin D level of 30 ng/ml (75 nmol/L).
The third set of women comes from the GrassrootsHealth Breast Cancer Prevention Project. This group of women self-selected to be in the study. To match the entry requirements of the RCTs, data from women aged 55 or older with no current cancer and not in treatment for cancer were included. They are asked to conduct an at-home blood test every six months (they prick their finger and drop blood on a special card) and also answer a health questionnaire. At the time of this paper, there were 1,713 women enrolled whose data could be included in the analysis, many of whom had vitamin D levels above 40 ng/ml. Adding this many women with a higher vitamin D level allowed the higher serum level to be included in the total analysis, which showed the 80% reduction in risk when going from 20 ng/ml to 60 ng/ml.
How is it different from other studies?
We summarize results from nine other breast cancer studies here. The big difference in this research is that the analysis assessed breast cancer risk across a broad range of 25(OH)D concentrations, including >40 ng/ml (most previous studies focused on the lower ranges). GrassrootsHealth cohort has the ONLY large set of people at 40 ng/ml (100 nmol/L) or higher.
Also, most vitamin D clinical trials are designed and interpreted by assigned treatment dose, not by blood levels of vitamin D. Not all people respond the same to a specific dosage nor does this capture vitamin D from the sun, food and personal supplements. Therefore, it is better to report on blood levels achieved, than the dosage given. That way, all a person needs to do is monitor their blood levels and use that as a measurement of sufficiency. (Recommended 40-60 ng/ml (100-150 nmol/L) or even now ≥ 60 ng/ml for cancer prevention).
How is it the same?
Many research studies show vitamin D reducing cancer risk, just like this one. If a trial shows no reduction in risk, it is worth looking at the details – Did the trial give enough vitamin D to produce a change? A relatively small dose, such as 400 IU/day, may not make a large enough change in vitamin D level for a difference in cancer risk to be observed. Did the vitamin D levels end up reaching at least 40-60 ng/ml? Did the trial follow participants long enough? Vitamin D changes take 2-3 months to change in the body and cancer may take longer to develop, so these trials should have longer time frames. And one common one, did they give vitamin D daily? It is explained here why that is important.
Treatment and control
Of the 5,038 women, 3,325 were enrolled in a study which assigned them to take a specific dose of vitamin D (1,100 IU or 2,000 IU /day) with calcium (1,400-1,500 mg/day), or two placebos. The remaining 1,713 women, enrolled in the GrassrootsHealth’ Breast Cancer Prevention Project, were allowed to choose their supplement amount with a target of at least 40 ng/ml. They were also provided with information on the benefits of vitamin D and the importance of a blood level above 40 ng/ml (100 nmol/L) for good health. They were not in a “blind” study and received the results of periodic vitamin D tests. Many of them did achieve higher blood levels because they had a concrete goal, were measuring regularly, and were receiving feedback on whether or not their methods were effective.
Results
As you can see, vitamin D levels have a significant correlation with breast cancer incidence. The horizontal, or x-axis, records increasing vitamin D levels, from 0 to 100 ng/ml. Note that the average vitamin D level for all women in the US is 29 ng/ml (72 nmol/L), for African Americans, 21 ng/ml (52 nmol/L). The vertical, or y-axis, records the number of people in the study. The white dots represent breast cancer occurrence, note they are mostly below 40 ng/ml (100 nmol/L), and very rare above 60 ng/ml (150 nmol/L).
What is your next step?
Which side of the chart above would you like to be on? Where would you like your wife? Your mother? Your children? Test today and start taking charge of your health.
Are You Getting Enough Vitamin D to Help Yourself?
We’re in a time of great crisis that could be greatly affected by making sure you and everyone you know has a serum level of at least 40 ng/ml. Help us help you.
Do you know what your vitamin D level is? Be sure to test today to find out, and take steps to keep it within a target of 40-60 ng/ml or 100-150 nmol/L! Give your immune system the nutrients it needs to support a healthy you and protect yourself from unnecessary diseases.
GrassrootsHealth is moving forward by using science to drive global action, with using either clinical trials with our key researchers or by doing community Field Trials with individuals or other organizations. Please let us know if you are interested and how we can quickly setup your projects.
Through GrassrootsHealth Nutrient Research Institute, you can also test your essential elements magnesium, copper, zinc and selenium, toxins such as lead, mercury and cadmium, as well as your omega-3 levels, inflammation levels and thyroid stimulating hormone (TSH) level. Find out your levels today! Log on to the test selection page (click the link below) to get your tests and see for yourself if your levels can be improved.
Make sure you track your results before and after, about every 6 months!
Click Here to Access the Test Page
How can I track my nutrient intake and levels over time?
To help you track your supplement use and nutrient levels, GrassrootsHealth has created the Personal Health Nutrient Decision System called
For each specific supplement, you can track what days you take it, how much, and many other details. This will help you know your true supplemental intake and what patterns of use work for you to reach and maintain optimum nutrient levels. Check it out today!