Published on May 18, 2021
Several studies conclude that regular sun exposure and higher vitamin D levels are related to decreased incidence of melanoma and increased melanoma survival rates
 Melanoma accounts for approximately 1-7% of all skin cancers (depending on the country) and is more dangerous than other skin cancers because it is more likely to spread to other parts of the body if not caught early. The sun has been to blame for an increased risk of melanoma, however, studies are now clearly showing that the incidence of melanoma and the risk of death due to melanoma are actually decreased with increased, regular, non-burning sun exposure and higher vitamin D levels. Increased risk can be seen with burning, intermittent, or sudden, drastic exposure to high intensity sunlight compared to regular, moderate, non-burning exposure to sunshine.
Melanoma accounts for approximately 1-7% of all skin cancers (depending on the country) and is more dangerous than other skin cancers because it is more likely to spread to other parts of the body if not caught early. The sun has been to blame for an increased risk of melanoma, however, studies are now clearly showing that the incidence of melanoma and the risk of death due to melanoma are actually decreased with increased, regular, non-burning sun exposure and higher vitamin D levels. Increased risk can be seen with burning, intermittent, or sudden, drastic exposure to high intensity sunlight compared to regular, moderate, non-burning exposure to sunshine.
Skin type, UV index, and duration of time spent in the sun are all important factors to consider when talking about safe sun exposure and decreasing risk for skin cancer, including melanoma. When transitioning between the seasons, it is also important to allow your skin to acclimate to the sun at a rate that avoids burning. By gradually increasing UV exposure to the skin (from the sun or other UV sources), the body can begin to produce more melanin in the skin without burning. This gradual process induces a natural photo-protection mechanism in the form of a tan, which in turn reduces the risk of a sunburn as the skin is exposed to sunnier and hotter days.
Inverse Association between High Occupational Sun Exposure and Risk for Melanoma
In 2005, a comprehensive review by Gandini et al. on sun exposure and melanoma found a positive association between intermittent, high intensity sun exposure and increased risk for melanoma (one increased the other) and an inverse association between high occupational sun exposure and risk for melanoma (one decreased the other). This means that as occupational sun exposure increased, the risk of melanoma decreased.
In 2012, the World Health Organization’s (WHO) International Agency for Research on Cancer (IARC) published a detailed analysis of studies on sun exposure and melanoma and found that continuous, regular sun exposure was not associated with melanoma, but rather, sunburn doubled the risk of developing melanoma and intermittent, high-intensity sun exposure proposed a 61% increased risk for melanoma.
A Clear Decrease in Melanoma Risk Seen as Vitamin D Levels Increase
Bolerazska et al. (2017) reported the current knowledge surrounding the synthesis of vitamin D in the skin and its effect on malignant melanoma and found that vitamin D may protect against melanoma due to its involvement in DNA repair, cell differentiation, cell death, cell adhesion, and oxidative stress – all mechanisms involved in cancer development. The paper emphasizes that the origin of malignant melanoma is due to sun burns in people who spend most of their time indoors, only getting sun exposure in excessive amounts over holidays (intermittent exposure).
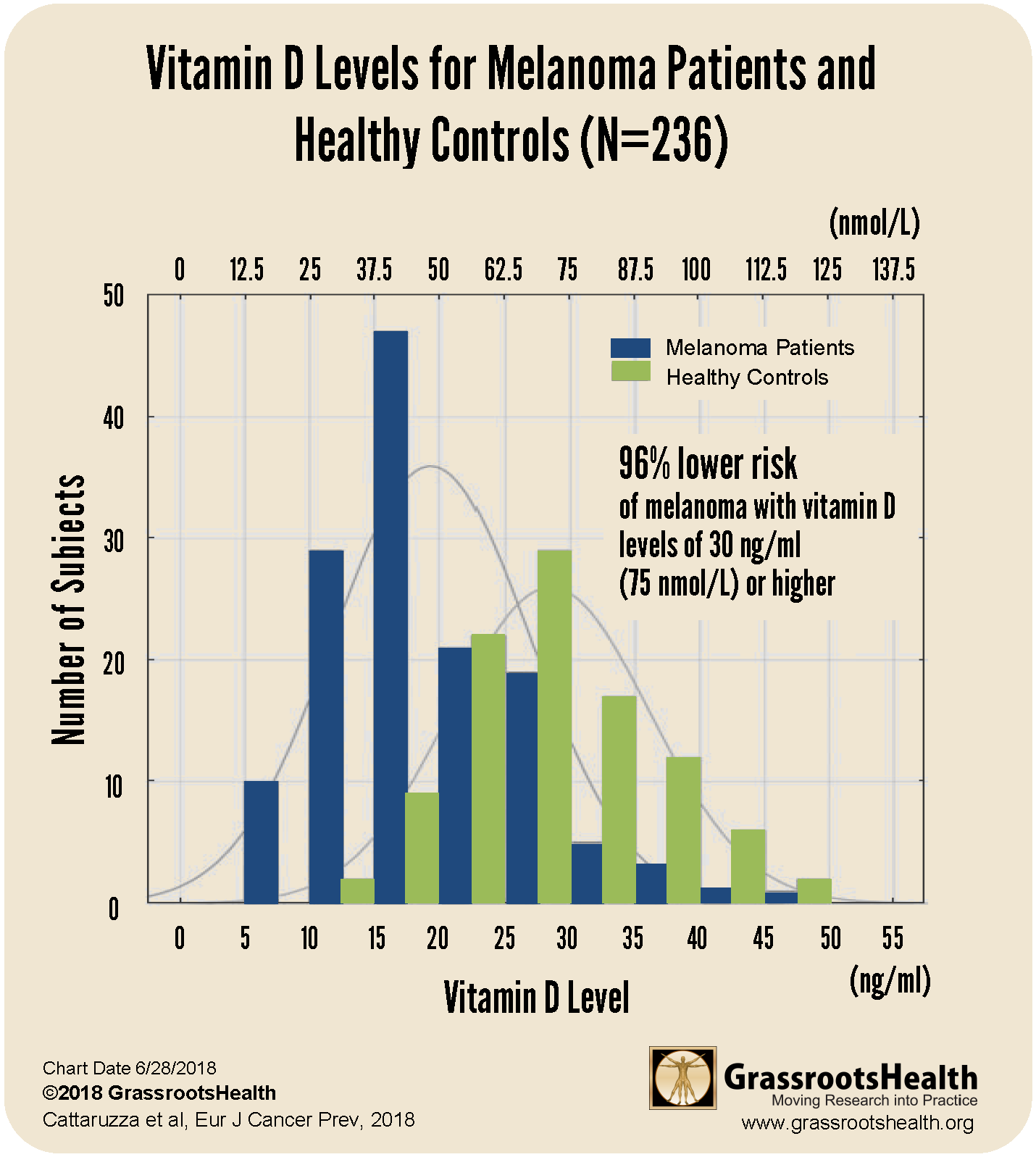
Results from a 2018 case-control study by Cattaruzza et al. showed a clear decrease in melanoma risk as vitamin D levels increased, as illustrated in the chart below.
This study included 137 melanoma patients and 99 healthy controls. The research team found that the average vitamin D level of melanoma patients was lower than the average level of the healthy controls by 10 ng/ml (25 nmol/L) and that the majority of melanoma patients had vitamin D levels at or below 20 ng/ml (50 nmol/L) compared to just 15% of the healthy controls. Furthermore, participants with vitamin D levels at or above 30 ng/ml (75 nmol/L) had a 96% lower risk of melanoma compared to participants with levels at or below 20 ng/ml (50 nmol/L) after adjusting for age, sex and BMI.
A 2020 meta-analysis by Tsai et al. looked at 25 studies, with a total of 11,166 melanoma patients, to evaluate the relationship between melanoma risk and prognosis, and vitamin D levels. They found that vitamin D deficiency was more prevalent among melanoma patients compared to controls (P<0.001), and melanoma patients had a significantly higher mortality rate if they had lower vitamin D levels compared to higher vitamin D levels (P<0.001). They also found that tumor thickness was significantly related to vitamin D level, with a thickness of 1 millimeter (mm) or less related to a higher vitamin D level and a tumor thickness of greater than 1 mm much more likely with lower vitamin D levels (P<0.001).
Skin Type, DNA Damage, and Melanoma
The differences in risk for developing melanoma are strongly associated with skin phenotype, or pigment of the skin. Since skin type influences sunburns and sunburns are associated with increased risk for melanoma, it is important to know your skin type to personalize your sun exposure. Individuals with fair complexion have the greatest risk for developing melanoma because they burn easily, whereas individuals with darker complexion are less likely to burn. This is because darker skin contains more melanin – a pigment that acts as natural sunscreen. While the amount of melanin in your skin is primarily genetic, it can also gradually increase through sensible sun exposure. This natural photo-protective response to sunshine is explained in detail by Dr. Edward Gorham in this recorded seminar lecture on Skin Cancer vs. Sunscreen – The Dilemma.
A study which aimed to identify the levels of sun exposure that generate vitamin D with minimal skin damage found that both vitamin D and DNA damage were produced across all skin types. They also found that the depth of DNA damage within the skin differed by skin type. Those with the darkest skin had DNA damage only in the surface layers of the skin whereas those with the lightest skin had DNA damage across all skin layers. The DNA damage in the deeper layers of the skin may explain why those with a fair phenotype have higher skin cancer rates. Studies, including those highlighted in this review article, have shown that vitamin D produced in the skin can decrease DNA damage in the skin cells and facilitate DNA repair directly upon any UV damage, and help prevent cell death.
Acclimating to the Sun to Prepare for Summer
In his lecture, Why the Sun is Necessary for Optimal Health, Dr. Alexander Wunsch presents the chart below as an illustration of how light therapists gradually acclimate the body to light (from sun or lamp).
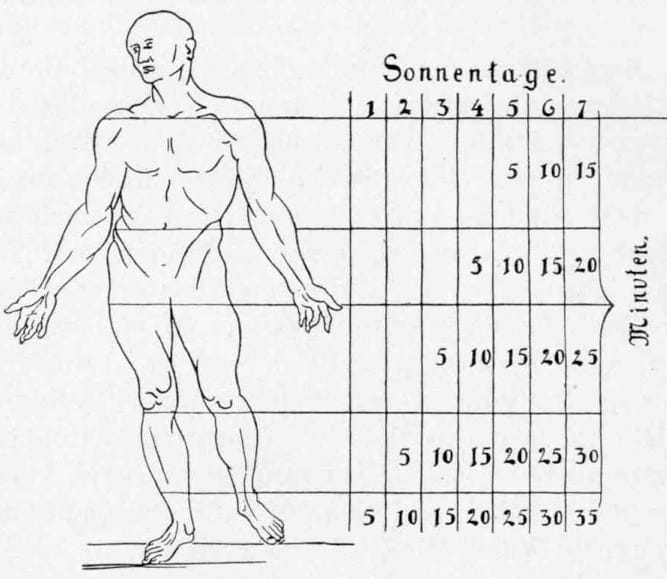
For the first exposure session, the therapist would only expose the feet to 5 minutes of light. Session 2, after 5 minutes of exposure only on the feet, a blanket is raised to expose the lower leg along with the feet for an additional 5 minutes, etc. You can see that this is a very gradual process, the timing of which will likely vary from one individual to the next.
Coming out of winter, most of us will need to acclimate slowly before going in the sun. If you hibernated all winter, don’t go whole hog at your first chance. Your skin is not prepared for it. During Dr. Wunsch’s presentation, he explains why – showing how skin cells acclimate to the sun and provide a natural sunscreen with gradual exposure.
There are a lot of benefits derived from sun exposure, and if used correctly, sunshine can greatly improve our health.
Be Sure to Get Healthy Sun Exposure and Healthy Vitamin D Levels!
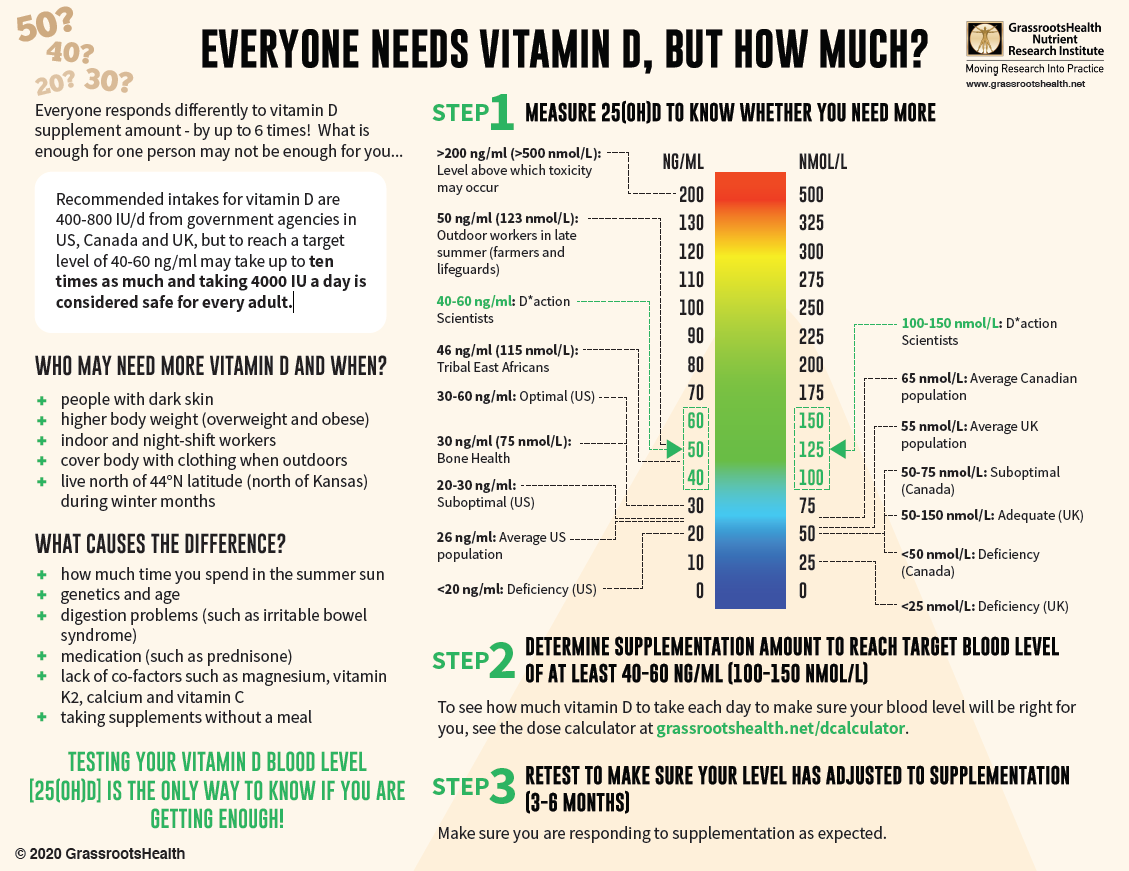
With almost 90% of the general population having vitamin D levels below the recommended 40-60 ng/ml (100-150 nmol/L), it is obvious that most people need more vitamin D. While most of us cannot achieve a vitamin D level of 40-60 ng/ml from sun alone, either due to our lifestyle, where we live, or other circumstances, we can certainly reach those levels with the right amount of supplementation.
Below is a guide for how much you might need, and who may need more. Your levels can be tested safely at home – order your home test kit today.
By joining the GrassrootsHealth projects, you are not only contributing valuable information to our study, but you are also gaining knowledge about how you could improve your own health through measuring and tracking your nutrient status, and educating yourself on how to improve it. Do you know what your status of vitamin D, omega-3s, and other essential nutrients is? Could your levels be improved? Test now to find out!
 We now have a NEW GIFTING SERVICE that allows you to quickly send ‘Gift Cards’ to friends, family and coworkers who you consider might need immediate access to testing, and to Claim the Joy of Your Health TODAY. Give the gift today!
We now have a NEW GIFTING SERVICE that allows you to quickly send ‘Gift Cards’ to friends, family and coworkers who you consider might need immediate access to testing, and to Claim the Joy of Your Health TODAY. Give the gift today!