Published on January 12, 2024
A recent article in a respected journal focuses on discrediting vitamin D and advancements made in vitamin D research – what should you believe, and how can you respond to this misinformation?
Key Points
- A recent Scientific American article can be viewed as the latest hit piece against vitamin D, and several of our followers and participants contacted us to know what our thoughts are about the information included; here we share some responses from Drs. Cedric Garland and Bruce Hollis, who are both on the GrassrootsHealth scientists’ panel and long-time researchers and scientists in the field of vitamin D, and several additional responses
- Results of the VITAL trial, when applied to the current annual number of 10,000,000 deaths from cancer worldwide, reveals that 1.7 – 2.5 million cancer deaths would be prevented by everyone taking 2,000 IU/day of vitamin D3; this abundant saving of deaths from cancer would be likely to occur in fewer than 5 years, yet this article totally neglects this outstanding outcome based on the VITAL data
- Additional important points to consider are the Nutrient Study Criteria defined by Dr. Robert Heaney, the mistakes made by the IOM in defining current recommended levels of vitamin D, and vitamin D levels naturally achieved within the body among those living an outdoor lifestyle…
 To kick off 2024, Scientific American featured an article on vitamin D titled How Much Vitamin D Do You Need to Stay Healthy?
To kick off 2024, Scientific American featured an article on vitamin D titled How Much Vitamin D Do You Need to Stay Healthy?
This article can be viewed as the latest hit piece against vitamin D, and several of our followers and participants contacted us to know what our thoughts are about the information included. The misinformation in the article is nothing new – we have written on all of it before. Below we share some responses from Drs. Cedric Garland and Bruce Hollis, who are both on the GrassrootsHealth scientists’ panel and long-time researchers and scientists in the field of vitamin D, followed by links to previous posts that address specific claims made in the article, most importantly
- A 3-part response to the fracture findings (and others) from the VITAL trial and how to assess the validity of findings from vitamin D research based on Dr. Robert Heaney’s nutrient study criteria.
- The video describing mistakes made by the IOM, What Vitamin D Serum Level Should We Target
Senior Vitamin D Researchers Respond to the Scientific American Article
 “This hit piece is obsolete and biased. It is unworthy of the great Scientific American brand, which has long been a beacon of truth in the reporting of scientific advances. Instead, the weirder, it is acting as the Grinch who stole Christmas and trying to devalue you the great advances made in the understanding of vitamin D during the past half century since its benefits against cancer and several important chronic diseases came to light.
“This hit piece is obsolete and biased. It is unworthy of the great Scientific American brand, which has long been a beacon of truth in the reporting of scientific advances. Instead, the weirder, it is acting as the Grinch who stole Christmas and trying to devalue you the great advances made in the understanding of vitamin D during the past half century since its benefits against cancer and several important chronic diseases came to light.
“The writer inexplicably glossed over the post-hoc analysis of the VITAL trial that revealed a 17-25% reduction in overall cancer mortality rates in the vitamin D group. These results of the VITAL RCT when applied to the current annual number of 10,000,000 deaths from cancer worldwide reveals that 1.7 – 2.5 million cancer deaths would be prevented by everyone taking 2,000 IU/day of vitamin D3. This abundant saving of deaths from cancer would be likely to occur in fewer than 5 years. This article totally neglects this outstanding outcome based on the VITAL data.
“They also did not mention that the otherwise legitimate VITAL randomized controlled trial used a now-obsolete exposure target of assignment to 2000 IU/day when the logical exposure criterion for the vitamin D group should have been the attained serum 25(OH)D concentration. This is because the response in the body to vitamin D supplementation varies enormously between individuals due to variations in amount of sunlight exposure, intestinal absorption, and diet.”
Cedric Garland DrPH FACE
—
 “I read with interest the Scientific American article on vitamin D. The author should realize that randomized controlled trials were never intended to be used for nutrient trials and are horribly confounded by circulating vitamin D prior to any study. This almost always results in null results.
“I read with interest the Scientific American article on vitamin D. The author should realize that randomized controlled trials were never intended to be used for nutrient trials and are horribly confounded by circulating vitamin D prior to any study. This almost always results in null results.
“In actuality, good observational and retrospective data are better because they represent a long-term lifestyle of an individual. I suggest you examine the following article recently published on vitamin D supplementation during pregnancy and childhood asthma by Scott Weiss, MD who is a leading world authority on the subject. The true results of this study were only uncovered after the data was analyzed in a fashion that corrected for entry point vitamin D levels of the subjects which removed this confounding factor from the analysis. Note what his recommendations are for future trials involving vitamin D as to not bias them from null results. Also note the supplementation levels he is recommending, which is quite a different from the article that was written. I have published extensively in this area for four decades, so I know the field quite well.”
Bruce W Hollis, PhD
Professor of Pediatrics
Medical University of South Carolina
Additional articles of interest suggested by Dr. Hollis, demonstrating the need for higher vitamin D especially for prenatal and childhood health outcomes:
Vitamin D and Child Neurodevelopment—A Post Hoc Analysis
The metabolic role of vitamin D in children’s neurodevelopment: a network study
How Else to Respond to the Misinformation in the Scientific American Article
Let’s start with the end of the article before we address the majority. At the very end, Scientific American states:
“Despite the disappointing trials on vitamin D, it’s not time to dismiss the vitamin completely… For instance, the VITAL trial showed that among slender or normal-weight people… vitamin D supplements appeared to lower the incidence of cancer, cancer deaths, and autoimmune disease.”
WOW! It’s amazing how these findings can be disregarded so easily (as part of the ‘disappointing trials’) while the additional points in the article were focused on instead. Dr. Garland pointed out the impact that this finding alone could make on cancer deaths above. If something as safe, simple, and inexpensive as vitamin D could make that big of an impact, why not focus the article on such a point? Let’s all remember the words of Benjamin Franklin,
“An ounce of prevention is worth a pound of cure.”
Unfortunately, the article chose to go a different direction. Several additional points were made in the Scientific American (SA) article that deserve a response. See below:
SA: “Although thousands of studies had linked low levels of vitamin D to an assortment of medical conditions, when scientists tried administering it as a means to prevent or treat those problems, the wonder supplement failed miserably.”
And “…randomized controlled trials, in which researchers recruit a group of participants and then assign them to receive different treatments (or a placebo), are considered the strongest kind of medical evidence… A randomized design makes it much more likely that any differences between the study and placebo groups are caused by the intervention rather than by some other variable.”
GrassrootsHealth: Read Making RCTs Work for (or Against) Vitamin D and our 3-part response to the fracture findings from the VITAL trial and how to assess the validity of findings from vitamin D research based on Dr. Robert Heaney’s nutrient study criteria.
- Part 1: Headlines Mislead to Make Some Believe Vitamin D is Useless
- Part 2: Did the VITAL Analysis Meet the Nutrient Study Criteria for Fracture Rates?
- Part 3: Did the VITAL Analysis Meet the Nutrient Study Criteria for Fracture Rates? cont
SA: “National population sampling showed that most people were already getting enough of the vitamin.” The article also consistently refers to the IOM’s definition of vitamin D deficiency, which was based on bone health, saying they “found that there were no benefits to having levels above 20 ng/ml… while noting that the majority of the population is just fine at 16 ng/ml.”
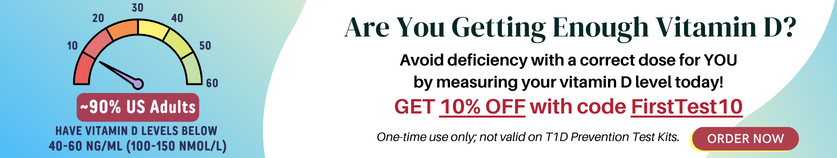
GrassrootsHealth: A chart of the findings from the National Health and Nutrition Examination Survey (NHANES, 2009-2014) data can be viewed in the blog Is Vitamin D Testing Necessary?, showing 23% of the population below 20 ng/ml (50 nmol/L). However, the definition of “enough” as defined by the IOM is a critical issue. A panel of 48 international vitamin D scientists and researchers agrees that the target vitamin D level should be 40-60 ng/ml (100-150 nmol/L); according to the NHANES data, 87% of the US population is below that recommended minimum target level.
Are the recommendations from the IOM enough?
- Read Current Recommendations are Too Low
- Watch the video What Vitamin D Serum Level Should We Target, for What?
- Watch the video by Dr. Patrick McCullough titled Why is there so much Confusion about Vitamin D? as he discusses the IOM report in detail
SA: Vitamin D “seems to bolster the immune system and tamp down inflammation.”
GrassrootsHealth: The many actions of vitamin D outside of bone health require higher levels of vitamin D for optimal function than what was defined as the minimum recommended level by the IOM. Check out a review of the strongest evidence available by Grant et al. that identifies differing optimal vitamin D levels needed to help prevent the top diseases known as major causes of death, Optimal Vitamin D Levels Differ for Specific Outcomes.
Also learn about system-specific nutrient response curves and why they are essential to understand, especially in the case of vitamin D, in the post titled Nutrient Reference Range vs Optimal Range.
SA: “Your liver and fat cells store vitamin D for future use… that means you don’t necessarily need a big dose every day…”
GrassrootsHealth: Learn more about the relationship between vitamin D in fat versus blood, and why this is important to understand, by reading Vitamin D is Fat Soluble: The storage debate
It is also important to understand why a daily dose of vitamin D is important for health, as explained in Do You Take Your Vitamin D Daily?
SA: The article focuses on findings from the VITAL trial quite a bit, in which 2000 IU per day of vitamin D was given for an average of 5.3 years. The study was “designed to look at whether vitamin D supplements could prevent cancer or cardiovascular disease.”
“The study findings were a shock. Vitamin D did not make a dent in cancer or heart disease, and it did not prevent falls, improve cognitive function or reduce bone fracture risk.”
GrassrootsHealth: Why the author would say that vitamin D “did not make a dent…” instead of focusing on the positive benefits they DID find with vitamin D is baffling. Read our post titled 30 Significant Outcomes from the VITAL Trial that You Likely Did Not Hear About, as well as the following posts based on the VITAL trial results:
- Vitamin D Supplementation Resulted in Lower Rates of Advanced Cancer and Cancer Death
- It’s Official: Vitamin D Reduces the Incidence of Autoimmunity
- And remember to keep in mind the concepts covered in Headlines Mislead to Make Some Believe Vitamin D is Useless
SA: Mentions the Vitamin D Assessment (ViDA) Study, which randomized participants to get either a placebo or 200,000 IU of vitamin D once per month; the study found no difference in tracked outcomes between groups.
GrassrootsHealth: Read When Taking Vitamin D Can be Ineffective and Possibly Harmful, which discusses how vitamin D supplementation done correctly can lead to great health benefits, but when taken in very large “pulse” or “bolus” doses, it can lead to a paradoxical vitamin D deficiency and contradictory results.
SA: “Three medical societies have endorsed a recommendation to not order population-based screening for vitamin D…”
GrassrootsHealth: …yet several vitamin D screening programs have proven successful, as outlined in Results from Vitamin D Testing Programs and Vitamin D Testing Reduces Healthcare Costs.
Also, read about our North Dakota project, which found that 45% of participants had vitamin D levels below 20 ng/ml and 20% were below 10 ng/ml! These folks would have likely remained vitamin D deficient (and suffered the health consequences of it) had their levels not been tested. Dismal Vitamin D Results among Participants in North Dakota Project
SA: “Although most people don’t need supplements, there are exceptions. Breast milk does not contain enough vitamin D for infants, so the American Academy of Pediatrics recommends that babies who are breastfed (partially or exclusively) be supplemented… In addition, the academy says all infants and children who consume less than 32 ounces of vitamin D-fortified formula or milk per day should also get supplements of 400 IU…”
GrassrootsHealth: Breast milk should be the perfect food for infants – yet they acknowledge that breast milk is deficient in vitamin D and consider this an exception to when supplementation is required. How does this make sense? Why would Mother Nature design breastmilk to be an incomplete food for infants?
The fact is, most breastfeeding mothers are deficient in vitamin D – which is the reason their breast milk does not have enough vitamin D to provide to their babies. Read about studies showing how, if the breast-feeding mother is getting enough vitamin D, her breastmilk will have enough vitamin D to provide to her baby. Infant Vitamin D Recommendations “A Largely Failed Initiative”
Also, children need additional vitamin D as they grow. Here are the Top 5 Reasons to Check Your Child’s Vitamin D Level
Let’s not forget ‘natural’ vitamin D levels found among those living an outdoor lifestyle, which range between 40 and 60 ng/ml (and climb even higher during pregnancy compared to any other time during the lifecycle). Should we Aim for ‘Natural’ Vitamin D Levels? This may be the best reason to question the conclusion made by the IOM that 16 ng/ml or even 20 ng/ml is all our bodies need to be healthy.
SA: “Despite the disappointing trials on vitamin D, it’s not time to dismiss the vitamin completely… For instance, the VITAL trial showed that among slender or normal-weight people… vitamin D supplements appeared to lower the incidence of cancer, cancer deaths, and autoimmune disease.” …WOW!… “But it’s possible that excess body fat may somehow hamper the effectiveness of vitamin D…”
GrassrootsHealth: The effect of body fat on vitamin D levels and the availability of vitamin D to other various tissues in the body is very well known and acknowledged in vitamin D literature. It should always be factored into vitamin D studies and individual recommendations for vitamin D supplementation. Read Vitamin D Supplementation Resulted in Lower Rates of Advanced Cancer and Cancer Death and learn why, as the amount of fat on the body increases (such as with obesity), the amount of vitamin D needed to maintain a healthy blood level also increases – a main reason why findings from trials on vitamin D should not be based on a single dose given to everyone, but on the achieved vitamin D blood level. Read Vitamin D is Fat Soluble: The storage debate as also suggested above.
We hope the above responses and links above provide anyone with more than enough information and resources for how to respond to the misinformation found in articles such as that recently published in Scientific American.
Please contact us (email jen(at)grassrootshealth.org) if we did not address a question or concern about vitamin D from this article.
Test to See if You Are Getting Enough Vitamin D and Other Important Nutrients
 Create your custom home test kit to measure your levels at home as part of the D*action project!
Create your custom home test kit to measure your levels at home as part of the D*action project!
With your kit you can measure your:
- Vitamin D
- Magnesium PLUS Essential and Toxic Elements
- Omega-3 Fatty Acids
- hsCRP
- HbA1c
- TSH
- Type 1 Diabetes Autoantibodies
Did you know that each of the above can be measured at home using a simple blood spot test? As part of our ongoing research project, you can order your home blood spot test kit to get your levels, followed by education and steps to take to help you reach your optimal target levels. Start by enrolling and ordering your kit to measure each of the above important markers, and make sure you are getting enough of each to support better mood and wellbeing!
Create your custom home test kit today. Take steps to improve the status of each of these measurements to benefit your overall health. With measurement you can then determine how much is needed and steps to achieve your goals. You can also track your own intakes, symptoms and results to see what works best for YOU.