Published on March 24, 2021
What is Vitamin D Good For? (Part 7: Cancer Prevention) – Vitamin D is needed by virtually every cell in the body, and is essential for hundreds of processes each and every day
 Cancer Prevention Awareness Week (March 20-26, 2021) has been launched to help people better understand the links between cancer and diet, lifestyle, weight, and other factors, as well as the steps they can take on a daily basis to help reduce cancer risk.
Cancer Prevention Awareness Week (March 20-26, 2021) has been launched to help people better understand the links between cancer and diet, lifestyle, weight, and other factors, as well as the steps they can take on a daily basis to help reduce cancer risk.
Vitamin D has known anticancer effects, and much research has been published over the last several decades showing a link between vitamin D levels and cancer risk. Depending on the type of cancer, vitamin D alone can potentially reduce the risk of cancer by about 25% to 80%! Today, as part of our What is Vitamin D Good For? series, we will focus on how vitamin D can help reduce cancer.
Since vitamin D acts as a protector and regulator, it is able to enhance the functioning of all types of cells, tissues and organs to keep us healthy. So far in this series, we have covered how vitamin D contributes to the health of the musculoskeletal system, dermatological system, reproductive system, respiratory system, cardiovascular system, and to cognitive and mental-emotional wellness. A deficit in vitamin D can lead to impairment or disease in each of these systems – from brittle bones to heart disease, cancer and dementia. With this in mind, why take a chance at being deficient in vitamin D?
Summary of Overall Benefits of Vitamin D to Help Fight & Prevent Cancer
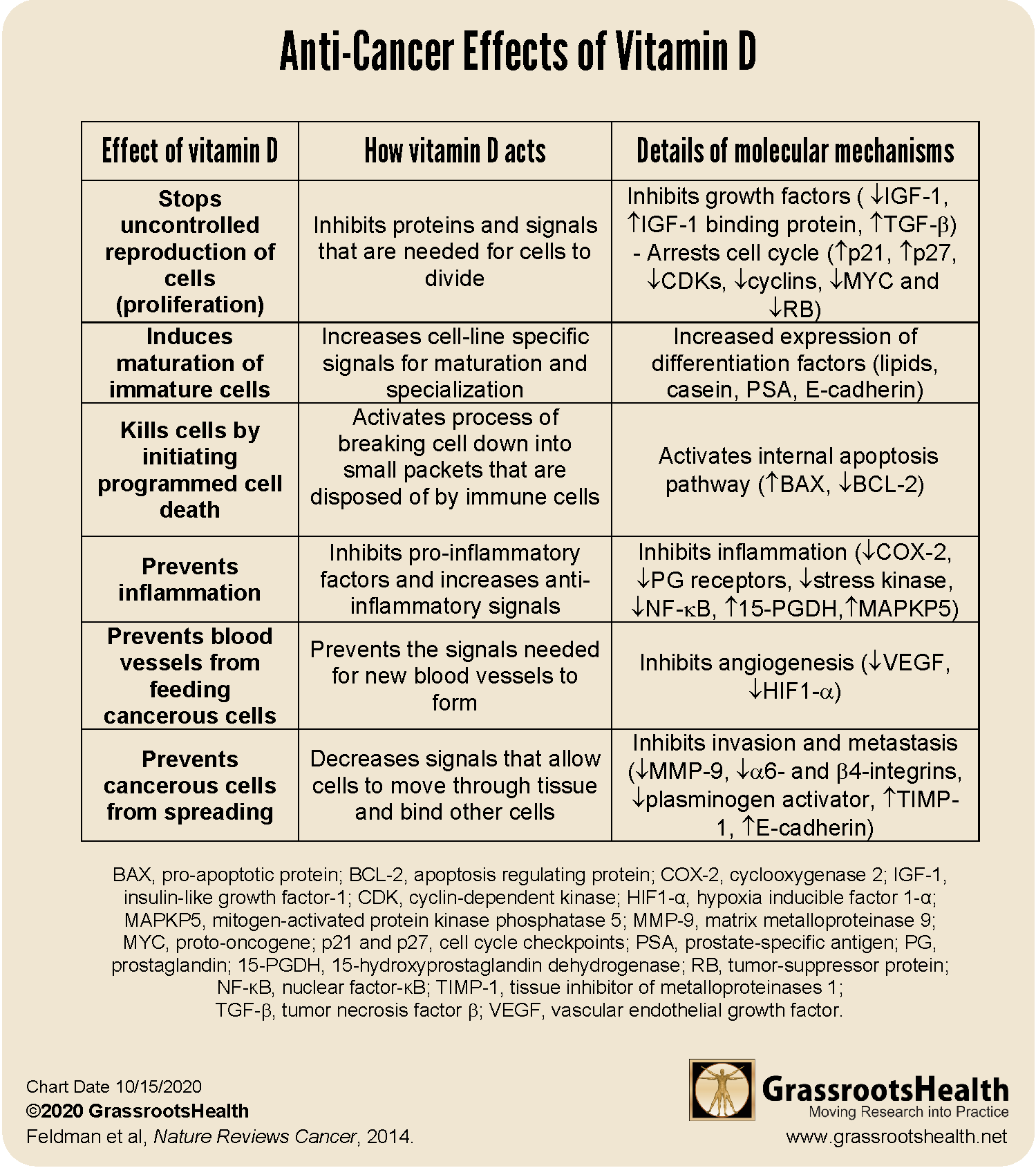
Anti-cancer functions of vitamin D include:
- Inhibits cancer cell growth and proliferation
- Reduces cancer metastasis
- Stimulates maturation of healthy cells (differentiation)
- Induces death of cancer cells (apoptosis or programmed cell death)
- Prevents blood vessel growth in tumors (angiogenesis)
- Prevents inflammation associated with cancer
- Reduces the risk of incidence and/or death due to cancer
Cancers associated with low vitamin D include:
- Colorectal cancer
- Breast cancer
- Prostate cancer
- Lung cancer
- Lymphoma
- Ovarian cancer
- Liver cancer
- Bladder cancer
Vitamin D is a Likely Causal Factor for Cancer Risk Reduction
The evidence associating vitamin D and cancer is so strong that vitamin D is now thought to be a causal factor in the risk-reduction of most types of cancer. Causation can be determined using Hill’s criteria for causality, a scientific set of guidelines for looking at data based on the strength of association, consistency between studies, temporality, biological gradient, plausibility, coherence with known scientific facts, experiment, and analogy. Two separate publications (WB Grant and Mohr et al.) have confirmed vitamin D as a causal risk-modifying factor for most cancers using Hill’s criteria.
How Vitamin D Fights Cancer
The active form of vitamin D, calcitriol, controls multiple pathways associated with the life cycle of the cell including those involved with reproduction, maturation and programmed death. Calcitriol regulates the production of a number of signals and growth factors at the genetic level. As detailed in the table below, some of the signals turned on by vitamin D stimulate growth, development, maturation and programmed cell death while other signals inhibit inflammation, prevent blood vessels from being made that can feed cancer cells, and stop the spread of the cancer to other parts of the body.
Specifically, calcitriol stops the uncontrolled reproduction of cancer cells by decreasing production of growth factors and increasing “stop” signals. In addition, calcitriol pushes the cell towards maturation and away from reproduction, and can also activate an internal process that starts programmed cell death in the cancerous cell. Part of the process for cancer growth and metastasis involves creating an inflammation response, building new blood vessels within the tumor, and breaking up surrounding tissue to allow the cancer to spread to other parts of the body. Calcitriol prevents inflammation, new blood vessel growth (called angiogenesis) and spread through inhibiting the signals needed.
Interestingly, some cancer cells find ways to stop vitamin D metabolism by the cell (by preventing the vitamin D receptor from being expressed, increasing the breakdown of calcitriol, or decreasing the production of calcitriol), which may help the cancer evade detection and continue to grow.
GrassrootsHealth Analysis Shows 71% Lower Cancer Risk
In April 2016, GrassrootsHealth partnered with leading vitamin D and cancer researchers Drs. Garland, Gorham, Heaney, and Lappe to publish Serum 25-Hydroxyvitamin D Concentrations ≥40 ng/ml Are Associated with >65% Lower Cancer Risk: Pooled Analysis of Randomized Trial and Prospective Cohort Study, a paper focused on achieved vitamin D serum levels and cancer incidence. Data was combined for women 55 and older from our GrassrootsHealth cohort (N = 1,135, median serum level = 48 ng/ml or 120 nmol/L) and the cohort of a previously published randomized controlled trial (RCT) of vitamin D and calcium supplementation with respect to cancer (Lappe RCT paper; N= 1,169, median serum level = 30 ng/ml or 75 nmol/L). The pooled cohort was analyzed to investigate cancer incidence over time (median = 3.9 years) for all invasive cancers combined, excluding skin cancer. Pooling the data allowed for a broader range of serum levels, more data, and thus improved statistical power.
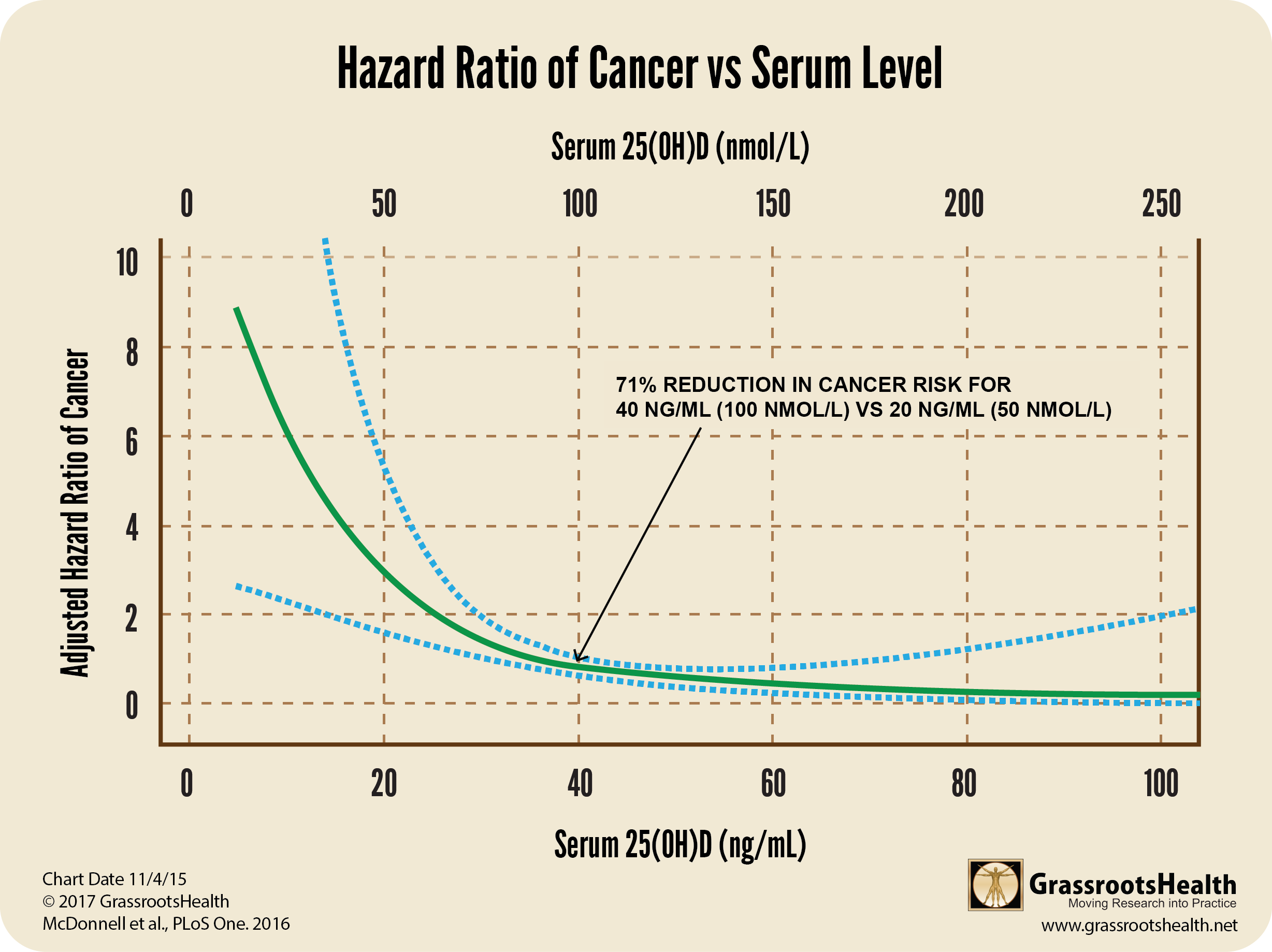
In the analysis, without adjusting for other risk factors, we found that women with a mean vitamin D serum level greater than or equal to 40 ng/ml (100 nmol/L) had a 71% lower risk of cancer than women with serum levels <20 ng/ml (<50 nmol/L; P-value = .02). The greatest decrease in risk occurred between about 10 – 40 ng/ml (25 – 100 nmol/L).
The graph below shows the plot of cancer incidence versus vitamin D level. The blue dotted lines are called the ‘confidence interval’, the closer they are to the actual plotted line (green line) the surer we are of the data, meaning the more data points we had in this region to ensure accuracy. Because we used D*action data with the Lappe data, we had a lot of people in the 40-60 ng/ml range (our recommended range) and can say clearly that cancer incidence is much lower when vitamin D levels are within this range.
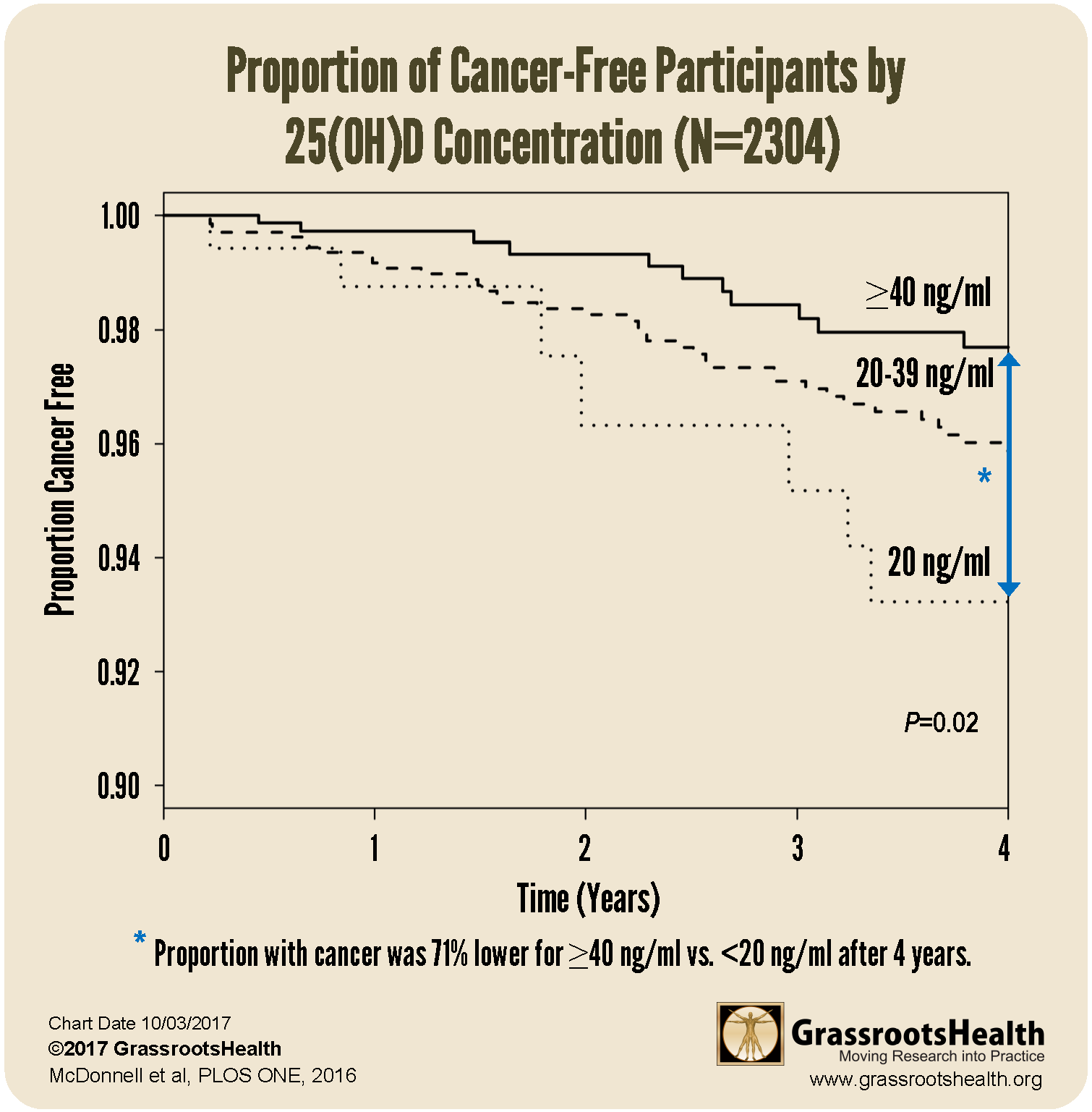
This second look at the combined data uses a Kaplan Meier curve to clearly illustrate the difference between the proportions of cancer-free participants at the end of the 4 year observation period.
The lines in the chart above represent the percent of participants without cancer for each vitamin D level group. Lines that are closer to the bottom of the chart represent higher cancer incidence and lines that are closer to the top of the chart represent lower cancer incidence.
VITAL Trial Shows Cancer Risk Reduction with Vitamin D Stronger when BMI Considered
The VITAL trial was a recent, randomized, double blind, placebo-controlled clinical trial conducted in multiple centers around the United States. It included 25,871 participants who were free of cancer and cardiovascular disease diagnoses at baseline. Participants were given 2000 IU vitamin D per day and 1 gram of marine omega-3 fatty acids per day, or placebo. The average vitamin D level at baseline among all participants was about 30 ng/ml (75 nmol/L).
Initial findings from the VITAL trial were published in November of 2018; one paper compared cancer outcomes between those assigned to vitamin D (2000 IU/day) vs. placebo. When cancer outcome results were analyzed excluding the first two years after study initiation (allowing time for vitamin D to have an effect), there was a 25% reduced risk of cancer mortality among those taking vitamin D (p=0.02).
In the VITAL trial, vitamin D levels varied significantly by BMI at baseline and after one year of supplementation. In participants with a normal BMI (25 to 30) average vitamin D levels increased from 29.5 ng/ml at baseline to 41.4 ng/ml at follow-up – meaning that only half of the participants achieved levels above 40 ng/ml (100 nmol/L) with 2,000 IU of vitamin D supplementation. In comparison, in those who were overweight (BMI above 30), average vitamin D levels did not reach 40 ng/ml, only increasing from 26.7 ng/ml at baseline to 38.6 ng/ml at one year.
When taking BMI into consideration for the analysis, the reduction in cancer was more pronounced. A significant reduction of metastatic or fatal cancer was seen among those with a normal BMI, with a decreased risk of 38% among those taking vitamin D compared to placebo (p=0.004); the findings were non-significant among those who were overweight or obese. In other words, the greatest risk reduction was seen among those with the lowest BMI, likely because the dose of 2,000 IU vitamin D per day was not enough to significantly increase vitamin D levels among those with a higher BMI.
Other Important Cancer Fighting Co-Nutrients
Don’t forget that vitamin D works along with other essential nutrients for our health. For anti-cancer effects, these include:
- Omega-3s for breast cancer and non-melanoma skin cancers
- Magnesium for breast cancer and cancer in general
- Vitamin C
- Selenium
Are you getting enough vitamin D and other nutrients to help prevent or reduce cancer?
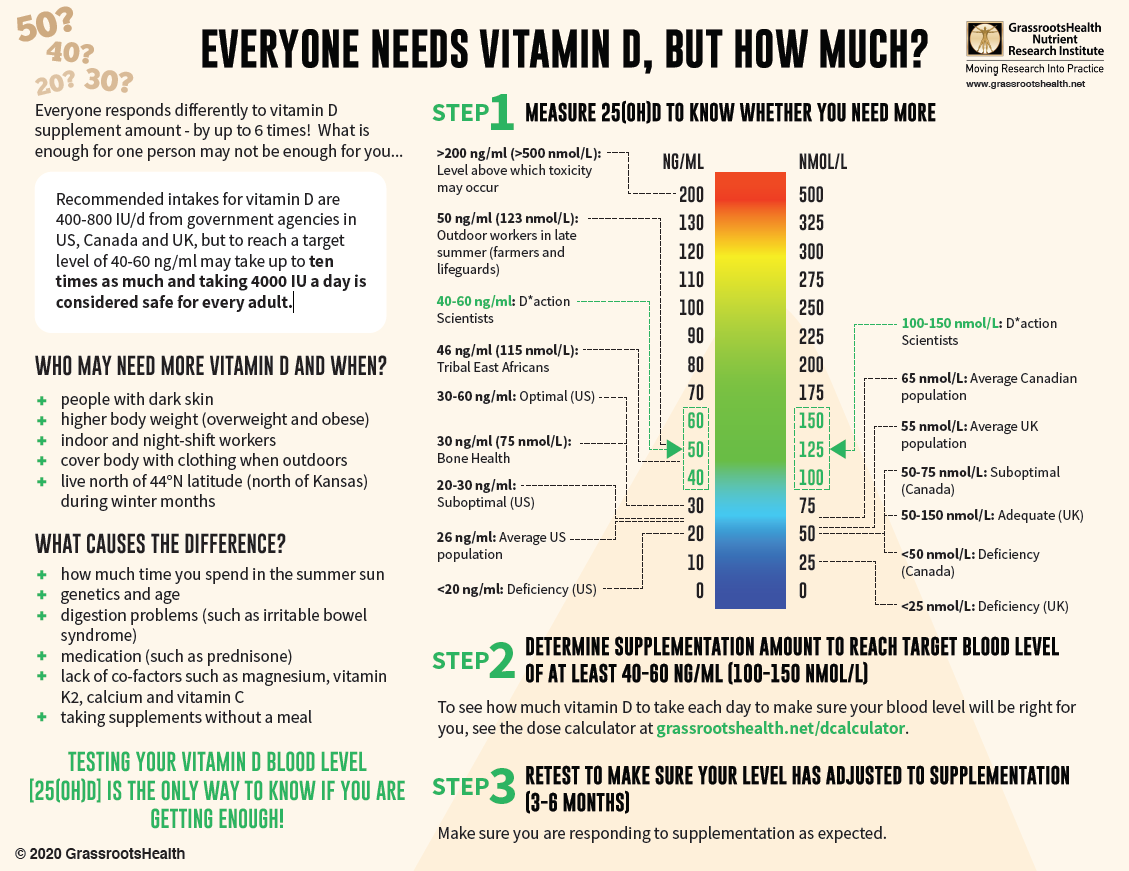
With almost 90% of the general population having vitamin D levels below the recommended 40-60 ng/ml (100-150 nmol/L), it is obvious that most people need more vitamin D. While most of us cannot achieve a vitamin D level of 40-60 ng/ml from sun alone, either due to our lifestyle, where we live, or other circumstances, we can certainly reach those levels with the right amount of supplementation.
Below is a guide for how much you might need, and who may need more. Your levels can be tested safely at home – order your home test kit today.
By joining the GrassrootsHealth projects, you are not only contributing valuable information to our study, but you are also gaining knowledge about how you could improve your own health through measuring and tracking your nutrient status, and educating yourself on how to improve it. Do you know what your status of vitamin D, omega-3s, and other essential nutrients is? Could your levels be improved? Test now to find out!