Published on June 2, 2021
New Study Finds 84% Lower Risk of Death for Hospitalized COVID-19 Patients Receiving Vitamin D Treatment vs No Vitamin D
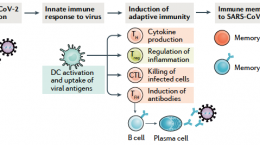
 Decades of research has demonstrated how the immune system relies on vitamin D, for both innate and adaptive immune function. Without enough vitamin D available, especially during certain acute respiratory infections, the immune response can become hindered, leading to an increased risk of severe symptoms, complications, and death. Since the main source of vitamin D is UVB from sunshine, those who do not get enough mid-day sun exposure or who do not take a vitamin D supplement have a high risk of vitamin D deficiency. In fact, approximately 90% of the adult population in the United States has a vitamin D level below the scientists’ recommended 40-60 ng/ml (100-150 nmol/L).
Decades of research has demonstrated how the immune system relies on vitamin D, for both innate and adaptive immune function. Without enough vitamin D available, especially during certain acute respiratory infections, the immune response can become hindered, leading to an increased risk of severe symptoms, complications, and death. Since the main source of vitamin D is UVB from sunshine, those who do not get enough mid-day sun exposure or who do not take a vitamin D supplement have a high risk of vitamin D deficiency. In fact, approximately 90% of the adult population in the United States has a vitamin D level below the scientists’ recommended 40-60 ng/ml (100-150 nmol/L).
The Body’s Demand for Vitamin D Increases during Acute Infections
A case study on the rise and fall of vitamin D throughout the day demonstrated not only that 25(OH)D levels fluctuate throughout the day and peak at mid-day, it also showed how vitamin D levels dropped just before an acute respiratory infection, even with consistent supplementation. This indicates the body’s increased demand for and use of available vitamin D (in the form of 25(OH)D) during the immune response.
25(OH)D3 (or calcifediol) is the form of vitamin D that is measured in the blood, after the vitamin D3 from the sun or diet has been converted within the liver. During a severe immune attack, when the need for vitamin D increases, waiting for the body to convert vitamin D3 to 25(OH)D3 may not be suitable for those who are vitamin D deficient, therefore 25(OH)D3 itself can be given in order to raise the blood levels more quickly.
Calcifediol Treatment for COVID-19 Shows More Promising Results
A pilot study on vitamin D and COVID-19, published by Castillo et al., found that the administration of 25(OH)D at the early stages of COVID-19 significantly reduced the need for admission to the intensive care unit (ICU), regardless of existing comorbidities, with no deaths in the treatment group compared to two deaths in the non-treatment group.
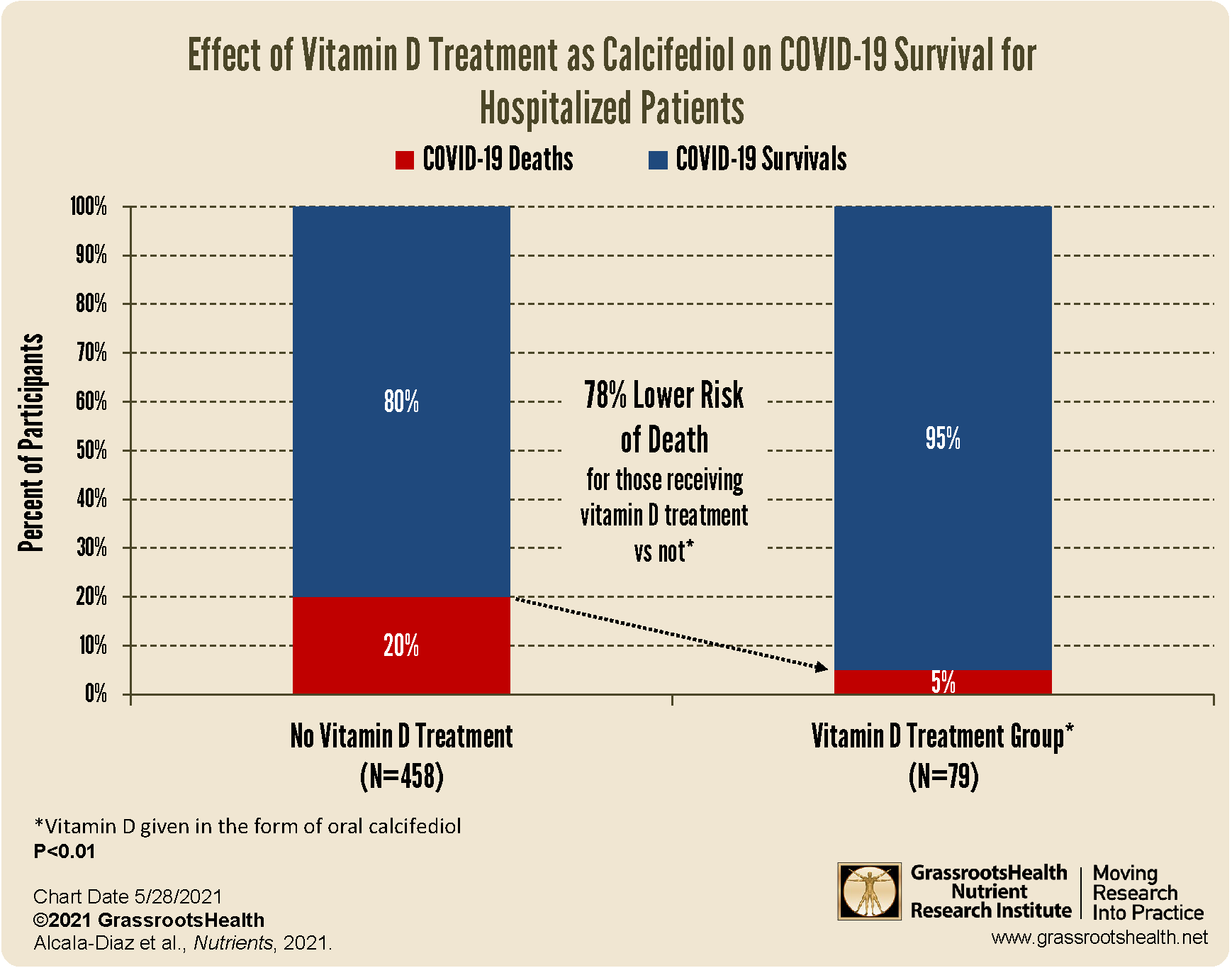
The same team of researchers performed a larger follow-up study, published by Alcala‐Diaz et al., to look at the mortality rate during the first 30 days after admission of patients receiving vitamin D treatment (in the form of calcifediol) in combination with the standard of care, compared to patients receiving only the standard of care. Patients who received the vitamin D treatment were given two capsules of 0.266 mg calcifediol upon admission, followed by one capsule on days 3, 7, 14, 21 and 28. There were a total of 537 patients included in the study, of which 79 received vitamin D treatment.
What did the study find?
The overall 30-day in-hospital death rate was 17.5%. The chart above shows the unadjusted, raw data, where the mortality rate among those receiving the vitamin D treatment was 5% compared to a mortality rate of 20% among those not receiving vitamin D (OR=0.22, P<0.01); a 78% lower risk of death for those receiving vitamin D treatment vs not.
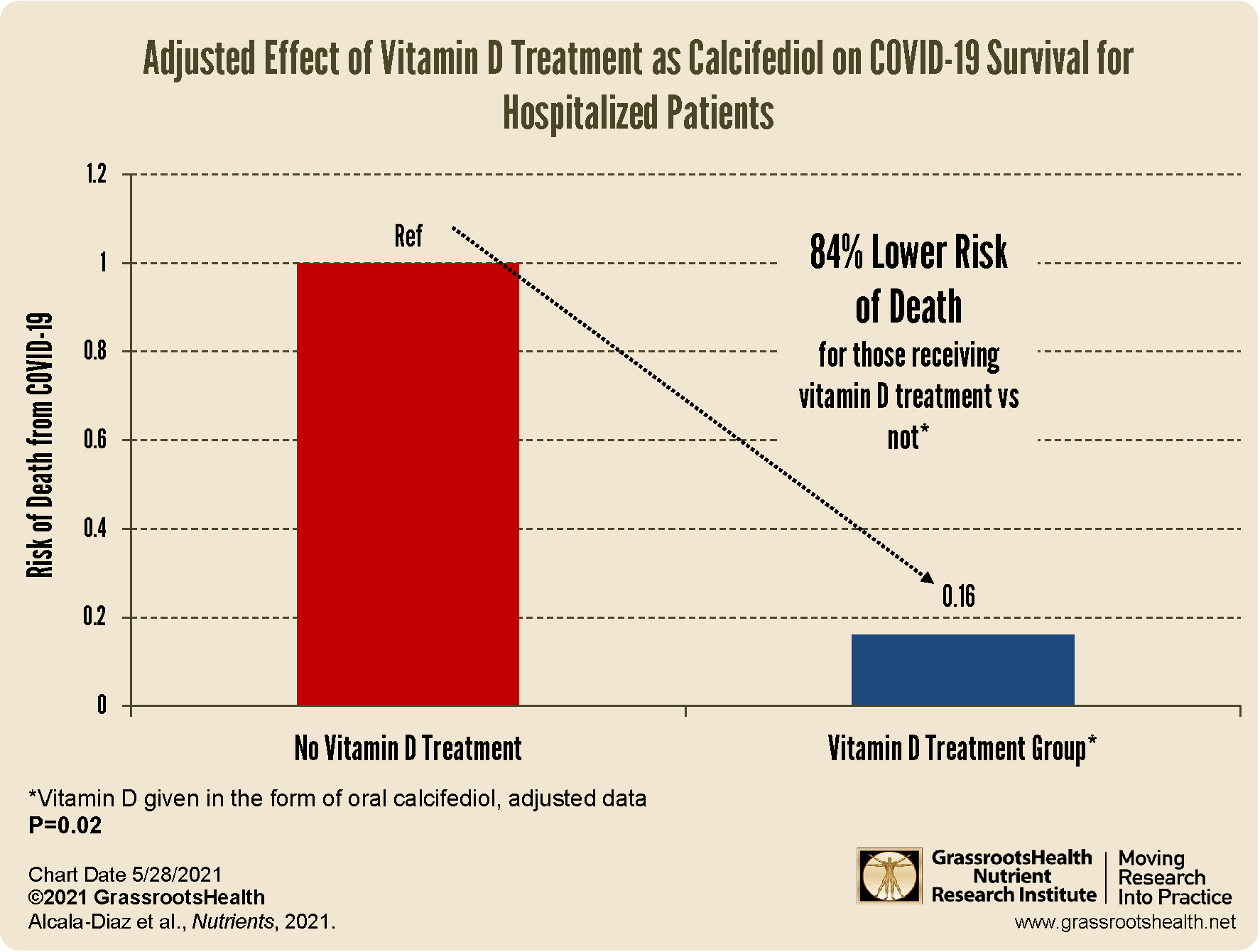
When the data was adjusted for confounding factors (variables that may also have an effect on COVID-19 survival and can influence the outcome of the study) such as age, gender, smoking status, and other existing medical conditions, there was an even further reduced risk among the vitamin D treatment group.
The adjusted data shows an 84% reduced risk of death for those receiving vitamin D treatment vs not (P=0.02), which is also a more precise indicator of the relationship between the risk of death from COVID-19 and the vitamin D treatment itself.
Check and Maintain Your 25(OH)D Levels to Keep Your Immune System Functioning Optimally
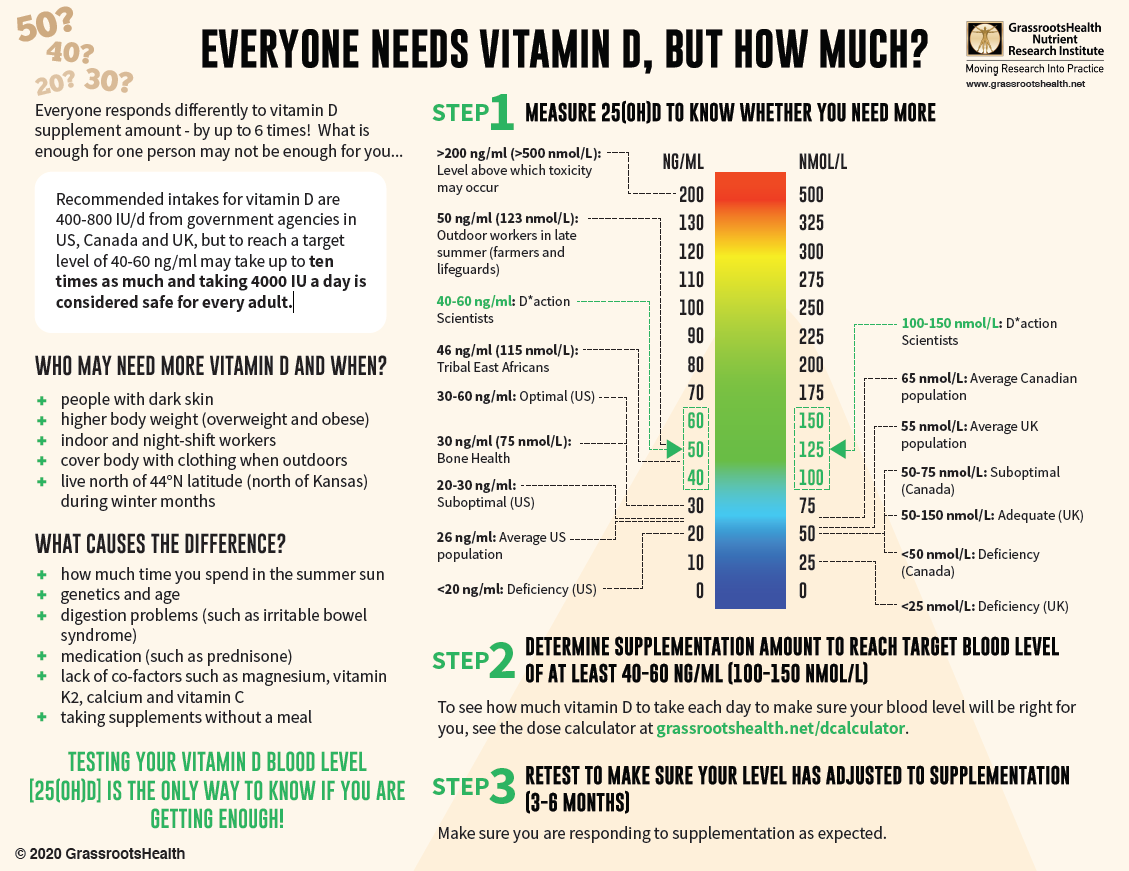
Measuring your vitamin D level is one way to tell if your body is getting enough, and correcting a vitamin D deficiency at any age and any time of life can decrease potential disease severity and improve outcomes. With almost 90% of the general population having vitamin D levels below the recommended 40-60 ng/ml (100-150 nmol/L), it is obvious that most people need more vitamin D. While most of us cannot achieve a vitamin D level of 40-60 ng/ml from sun alone, either due to our lifestyle, where we live, or other circumstances, we can certainly reach those levels with the right amount of supplementation.
Below is a guide for how much you might need, and who may need more. Your levels can be tested safely at home – order your home test kit today.
By joining the GrassrootsHealth projects, you are not only contributing valuable information to our study, but you are also gaining knowledge about how you could improve your own health through measuring and tracking your nutrient status, and educating yourself on how to improve it. Do you know what your status of vitamin D, omega-3s, and other essential nutrients is? Could your levels be improved? Test now to find out!
 We now have a NEW GIFTING SERVICE that allows you to quickly send ‘Gift Cards’ to friends, family and coworkers who you consider might need immediate access to testing, and to Claim the Joy of Your Health TODAY. Give the gift today!
We now have a NEW GIFTING SERVICE that allows you to quickly send ‘Gift Cards’ to friends, family and coworkers who you consider might need immediate access to testing, and to Claim the Joy of Your Health TODAY. Give the gift today!