Published on February 6, 2024
From a physiological set-point perspective, ‘normal’ vitamin D status would be a 25(OH)D concentration that requires little or no compensatory PTH response under basal conditions, where minimal adaptation is necessary, which occurs around 50 ng/ml
Key Points
- The current approach to defining nutrient recommendations is to presume that average intakes in the general population are adequate (normal), and to require hard evidence that something more or less would be better; this despite the fact that the populations of the industrialized nations are beset with a myriad of chronic health conditions and the individuals we take as our benchmark normal are, in fact, individuals in the incubation stage of one or more chronic disorders
- The “set point” criterion or the “least adaptation” criterion approach is based on the fact that many – perhaps most – physiological systems function at a status or setting that ensures that conditions are optimal for our physiology, operating around a system-specific set point to maintain those functions
- For example, a low level of PTH in the blood is an indication not only of the adequacy of diet calcium, but of vitamin D status, as well, and the point at which further increases in vitamin D status produce no further decreases in PTH concentration defines the PTH set point for both calcium and vitamin D; such a value would seem to be a reasonable estimate of optimal vitamin D status, and therefore an indicator of the vitamin D requirement
 Written by Robert P. Heaney, M.D., reviewed for updates by Reinhold Vieth, PhD.
Written by Robert P. Heaney, M.D., reviewed for updates by Reinhold Vieth, PhD.
In a recent post I pointed out that clinical nutrition as a discipline, and the nutrition policy establishments in particular, have no shared concept of what is “normal” nutrition. This creates obvious difficulties in formulating and publishing recommendations for nutrient intakes. The approach currently in vogue is to presume that average intakes in the general population are adequate, and to require hard evidence that something more or less would be better. This despite the fact that the populations of the industrialized nations are beset with a myriad of chronic health conditions, piling up toward the end of life, and including such disorders as cancer, cardiovascular disease, atherosclerosis, obesity, osteoporosis, diabetes, dementia, and many others. Unavoidably, the individuals we take as our benchmark normal are, in fact, individuals in the incubation stage of one or more of these chronic disorders. Thus presuming that typical intakes are “normal” (i.e., optimally healthful) is clearly circular.
In a prior post I suggested an alternative approach to the definition of “normal” as applied to nutrition, i.e., selecting the ancestral intake, the one that prevailed when human physiology was evolving. In this post, I offer yet another possible criterion, one that could be applicable to many nutrients. It might be called the “set point” criterion or perhaps better, the “least adaptation” criterion.
This suggested approach is based on the fact that many – perhaps most – physiological systems function at a status or setting that ensures that conditions are optimal for our physiology. We maintain those settings by control systems that operate around a set point. The number of such systems is legion, including thirst, hunger, blood pressure, blood sugar, body temperature, bone mass, the ionic composition of the various body water compartments, on and on.
Perhaps the most familiar example of such a system is the means whereby we regulate the temperature in our homes and work places. We have a device called a thermostat, and we set it to a certain temperature (the “set point”). If the temperature falls below that set point, then the heating system kicks in and pours heat into the system. Conversely, if the temperature rises above that setting, then the cooling system does the opposite. The colder the temperature outside, the more the heating system has to work. The downside of too much work by the heating or cooling systems is not just the extra energy cost, but the fact that the equipment, working harder and longer, wears out sooner.
All analogies limp, but this one is better than most, with our various body systems working almost exactly as I’ve just described. There’s just one small difference: in our dwellings we are able to change the set point, while in our bodies we can’t; they’ve been pre-set for us by the forces of natural selection.
Take for example the regulation of blood calcium concentration. For reasons that are not entirely understood, the concentration of calcium ions in our blood serum and body fluids is one of nature’s physiological constants, with the same value being found across most of the vertebrate phylum. The set point value for total serum calcium is about 2.4 mmol/L (9.6 mg/dL). In humans calcium is lost from the body in a variety of ways, and is gained by the body from absorption of the calcium contained in the foods we eat. The job of the regulatory system is to reduce the impact of those gains and losses on blood calcium concentration so that it doesn’t vary appreciably in response to the inevitable variation in inputs and losses over the day. The body uses two hormones of the endocrine system to counter these fluctuations: for a fall in blood calcium, parathyroid hormone (PTH), and for a rise in blood calcium, calcitonin. These hormones are exact counterparts of the heating and cooling systems in our dwellings.
Under the environmental conditions in which human physiology evolved, calcium was a surfeit nutrient. For that reason, our intestines have evolved to block most calcium absorption. Only about 10–12% of diet calcium is absorbed unless we actively need more, at which point the endocrine control loops cause the intestine to extract more of the calcium from our foods. But today our diets are relatively low in calcium, which means that the PTH arm of the control system is usually more active than the calcitonin arm. The concentration of PTH circulating in our blood stream is, thus, a reflection of how close our serum calcium level is to the set point, or how hard the body has to work to keep it there. When calcium intakes are low (either because the food contains little calcium or because, with vitamin D deficiency, we’re not absorbing efficiently), PTH levels will typically be elevated. And, accordingly, when absorbed calcium intakes rise, PTH levels fall, until they reach some minimum value below which they drop no further, no matter how much additional calcium we may consume. Other things being equal, a low PTH level is an indication of calcium adequacy. One can see immediately how this approach could be used to define the “normal” calcium intake, i.e., the intake that ensures that the body is not required to adapt or compensate for what the diet has failed to provide.
This is not to suggest that adaptation or compensation are not, themselves, “normal”. Indeed they are. Even under optimal ancestral conditions, when human physiology was evolving, external conditions and food sources were constantly in a state of flux. Indeed, the ability to respond, to adapt, and to compensate is an integral feature of life itself and is to be found in all living organisms, from the most simple to the most complex. Even with a theoretically optimal calcium intake, there will be times during the day when some degree of compensation is necessary, simply because there will be times during the day when there is no calcium-containing food within the portions of the intestine that absorb calcium. So we have to be able to adapt. The question is: How much adaptation is just right? And: How much is too much?
The adrenal hormones are clearly of vital importance in helping us adapt to stressful situations, but nearly everyone knows that living with a high adrenaline level all the time, or a high cortisol level, is neither healthful nor pleasant. Is there a physiological cost from too much PTH, just as there is a cost from too much adrenaline or cortisol? The answer is clearly “yes”. Constantly high levels of PTH increase the rate of bone remodeling activity and decrease bone strength in the areas being remodeled. That leads to skeletal fragility and fractures. That is probably the main reason why low calcium intakes predispose to osteoporosis.
The foregoing discussion has focused on calcium intake, properly considered, but it applies, also, to the issue of vitamin D adequacy. The reason, as hinted above, is that the intestine’s ability to increase calcium absorption in response to PTH is dependent upon vitamin D status. One simply cannot absorb enough calcium from typical diets, no matter how high the PTH level, if there is appreciable vitamin D inadequacy. So, a low level of PTH in the blood is an indication not only of the adequacy of diet calcium, but of vitamin D status, as well.
How would one apply this understanding to the requirement for vitamin D? The approach I’m suggesting is to evaluate the relationship between PTH concentration and vitamin D status, as in this figure.
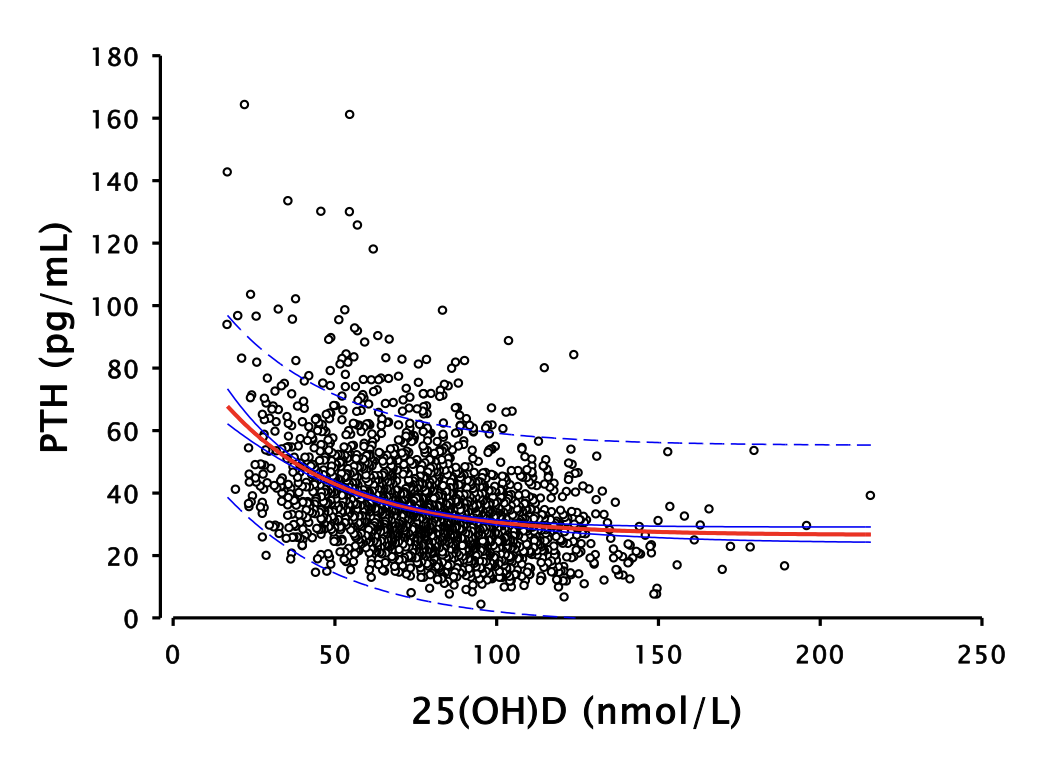
The data behind the figure come from a group of over 2,300 individuals studied in our laboratories at Creighton University in whom measurements were made of both PTH and vitamin D status [serum 25-hydroxyvitamin D – 25(OH)D]. The figure shows clearly the expected high levels of PTH at low vitamin D status values, with PTH concentration falling and becoming essentially flat as vitamin D status rises to levels in the range of 125 nmol/L (50 ng/mL). Exactly the same relationship is exhibited in a report from the National Health and Nutrition Examination Survey, involving a population-based sample of over 14,000 individuals. Both data sets found almost exactly the same vitamin D status level, above which PTH fell no further.
Because there are many factors that influence PTH concentration beyond vitamin D status, this approach will not work very well in determining individual requirements of calcium or vitamin D. However, it does work at a population level, as the graph shows.
The point at which further increases in vitamin D status produce no further decreases in PTH concentration [i.e., a plot of PTH on 25(OH)D is flat] defines the PTH set point for both calcium and vitamin D. This is the point around which the body can exercise its regulatory control of serum calcium concentration with optimal capacity in both directions. The need to compensate, and the duration of adaptation are minimized. Such a value would seem to be a reasonable estimate of optimal vitamin D status, and therefore an indicator of the vitamin D requirement.
Postscript. Another nutrient for which this approach seems preeminently well suited is sodium. Details will have to wait for another post, but it is enough to say here that low sodium diets require a constant adaptative response, without which blood pressure would drop to dangerously low levels. Sodium intakes requiring the “least adaptation” appear to fall between 2500 and 4500 mg per day.
About Dr. Robert P. Heaney
 Dr. Heaney was a full time professor at Creighton University who also donated his time and energy, starting in 2012 until his passing in 2016, as Research Director at GrassrootsHealth. In this capacity Dr. Heaney consulted on studies, methodologies, and how to best change public health direction. Dr. Heaney provided nearly 50 years of advancements in our understanding of bone biology, osteoporosis, and human calcium and vitamin D physiology. He is the author of three books and has published over 400 original papers, chapters, monographs, and reviews in scientific and educational fields. At the same time, he has engaged nutritional policy issues and has helped redefine the context for estimating nutrient requirements. Dr. Heaney was presented a lifetime achievement award in the US House of Representatives on November 10, 2015 (Watch the video here). He was an inspiration to researchers everywhere – his intellect, dedication, integrity, and caring was unsurpassed.
Dr. Heaney was a full time professor at Creighton University who also donated his time and energy, starting in 2012 until his passing in 2016, as Research Director at GrassrootsHealth. In this capacity Dr. Heaney consulted on studies, methodologies, and how to best change public health direction. Dr. Heaney provided nearly 50 years of advancements in our understanding of bone biology, osteoporosis, and human calcium and vitamin D physiology. He is the author of three books and has published over 400 original papers, chapters, monographs, and reviews in scientific and educational fields. At the same time, he has engaged nutritional policy issues and has helped redefine the context for estimating nutrient requirements. Dr. Heaney was presented a lifetime achievement award in the US House of Representatives on November 10, 2015 (Watch the video here). He was an inspiration to researchers everywhere – his intellect, dedication, integrity, and caring was unsurpassed.
Read more about Dr. Heaney and a few of his accomplishments here.
How Are Your Levels of Important Nutrients?
Do you know what your vitamin D level is? Check yours along with omega-3s, magnesium, and other levels today as part of the vitamin D*action project; add the Ratios for more about how to balance your Omega-3s and 6s!
Measure your:
- Vitamin D
- Magnesium PLUS Elements
- Omega-3 Fatty Acids
- hsCRP (for Inflammation)
- HbA1c (for Blood Sugar)
- and more
Did you know that each of the above can be measured at home using a simple blood spot test? As part of our ongoing research project, you can order your home blood spot test kit to get your levels, followed by education and steps to take to help you reach your optimal target levels. Start by enrolling and ordering your kit to measure each of the above important markers, and make sure you are getting enough of each to support better mood and wellbeing!
Build your custom kit here – be sure to include your Omega-3 Index along with your vitamin D.
Start Here to Measure Your Levels