Published on April 28, 2021
Nutrient intervention studies and individuals may get unexpected results when they don’t include evaluating co-nutrient intake or status
Key Points
- Calcium and magnesium are both essential minerals required by all cells to function properly, they work together to help the heart muscles beat, the nerve cells to communicate, and the bones to stay strong; both are also well-known co-nutrients of vitamin D
- Most individuals get enough calcium, however, at least half of us do not get enough magnesium on a daily basis, which may lead to health effects ranging from fatigue and loss of appetite, to tremors and muscle cramps; severe magnesium deficiency can cause cardiac arrhythmias
- The effect of either calcium or magnesium supplementation on a disease outcome may be dependent on an individual’s current calcium and magnesium intake ratio, or Ca:Mg, as seen in several studies described below
 Nutrients function in collaboration with each other in a co-dependent relationship. If one co-nutrient is limited, either missing or not plentiful enough in comparison to another co-nutrient, then the functions they are meant to carry out together may also be limited. Some examples include how different nutrients work together for bone health, how they are relied upon for certain enzymes to function, and more specifically, how some nutrients can influence the status and utilization of other nutrients.
Nutrients function in collaboration with each other in a co-dependent relationship. If one co-nutrient is limited, either missing or not plentiful enough in comparison to another co-nutrient, then the functions they are meant to carry out together may also be limited. Some examples include how different nutrients work together for bone health, how they are relied upon for certain enzymes to function, and more specifically, how some nutrients can influence the status and utilization of other nutrients.
In this post, we will focus on the intricate balance of magnesium and calcium and their relationship to vitamin D.
Most Get Enough Calcium but Not Enough Magnesium
Calcium and magnesium are both essential minerals required by all cells to function properly. They work together to help the heart muscles beat, the nerve cells to communicate, and the bones to stay strong. Both are also well-known co-nutrients of vitamin D.
Besides being essential for bone health, calcium helps regulate nerve transmission, muscle contractions, blood pressure, and blood clotting. Calcium requirements can be easily achieved through the diet for most individuals, by eating foods such as dairy, leafy green vegetables, beans and fortified foods. Calcium intake among adults in the United States has increased over the last several decades, with a 3-6 times increase in mean intake, especially among individuals taking supplements.
While most individuals do get enough calcium, at least half of us do not get enough magnesium on a daily basis, which may lead to health effects ranging from fatigue and loss of appetite, to tremors and muscle cramps. Severe magnesium deficiency can cause cardiac arrhythmias. Magnesium is one of the most important co-nutrients for vitamin D metabolism and utilization, and adequate intake of magnesium is especially important for the use of vitamin D within the body. It’s intrinsic to bone and tooth structure, calcium and vitamin D absorption, regulation of the cell cycle and stability of cells. There has been additional evidence showing a potential relationship between magnesium deficiency, chronic inflammation, CRP levels, and the development of multiple types of cancer, including breast cancer and colorectal cancer. Magnesium also regulates sodium, potassium, proton and calcium transport, all especially important for heart health. However, increasing magnesium intake alone in some studies has not always shown to be beneficial, even for the above health effects.
Calcium to Magnesium Intake Ratio may be More Important than Intake of Either Alone
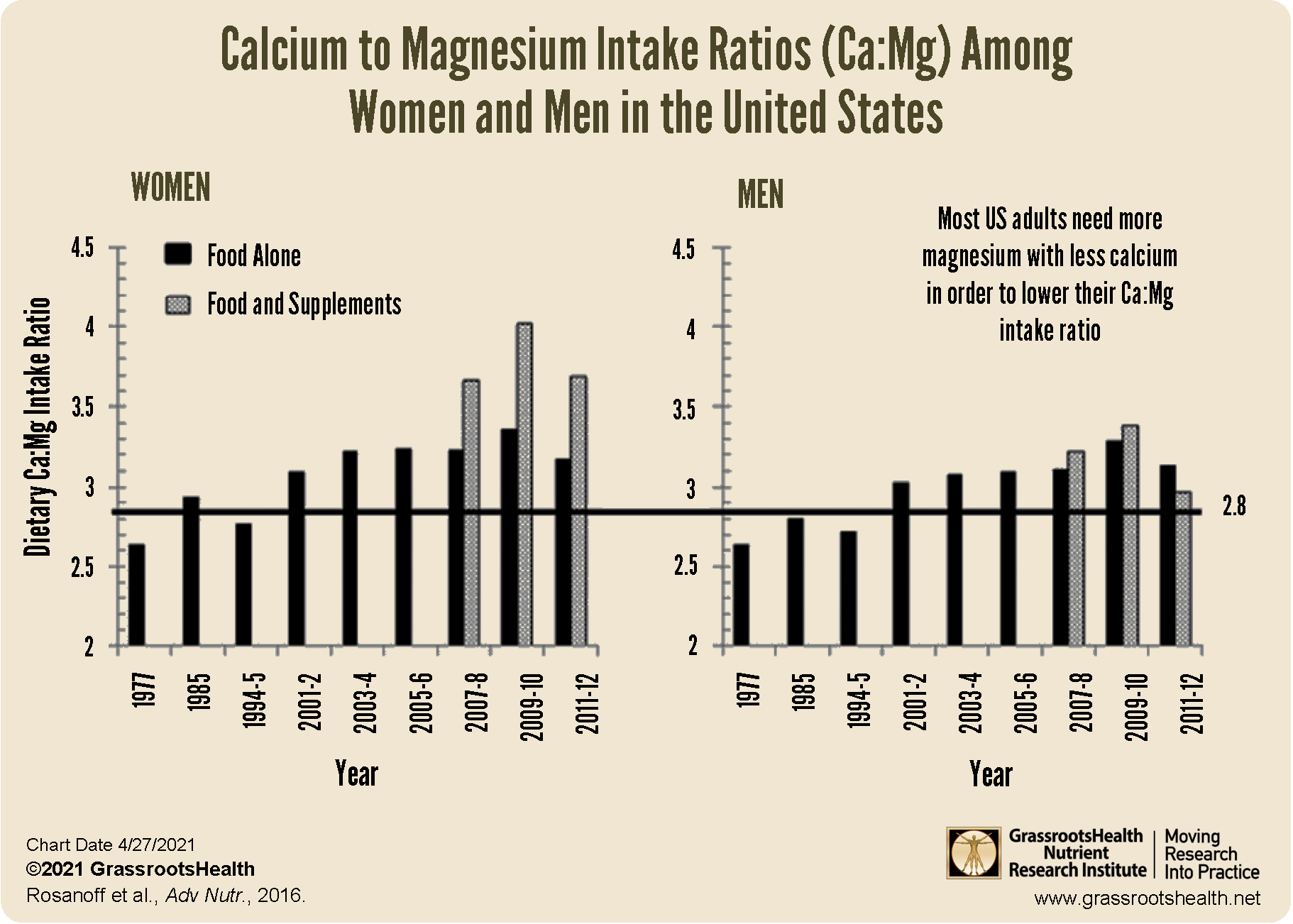
While magnesium intake has increased over the last several decades, it has only done so by 1.5-3 times, resulting in an average dietary calcium to magnesium intake ratio (Ca:Mg) of greater than 3.0 among adults in the United States. Research has shown an optimal Ca:Mg intake may be closer to 2.0, as discussed in a review by Rosanoff et al..
Additionally, while adults who take supplements that contain magnesium are more likely to achieve an average intake above the RDA, their intake of calcium also tends to be much higher, especially among female supplement users, as can be seen in the Ca:Mg intake graphs below.
What is the Problem with a Ca:Mg Intake that is Too High?
According to Rosanoff et al., these two minerals play an intricate role within all living cells, and the balance between them is so important that the intake of one can affect retention of the other. In fact, studies have shown that increased calcium intake may lead to increased urinary excretion of magnesium, while magnesium intake may reduce calcium absorption and/or increase urinary calcium excretion.
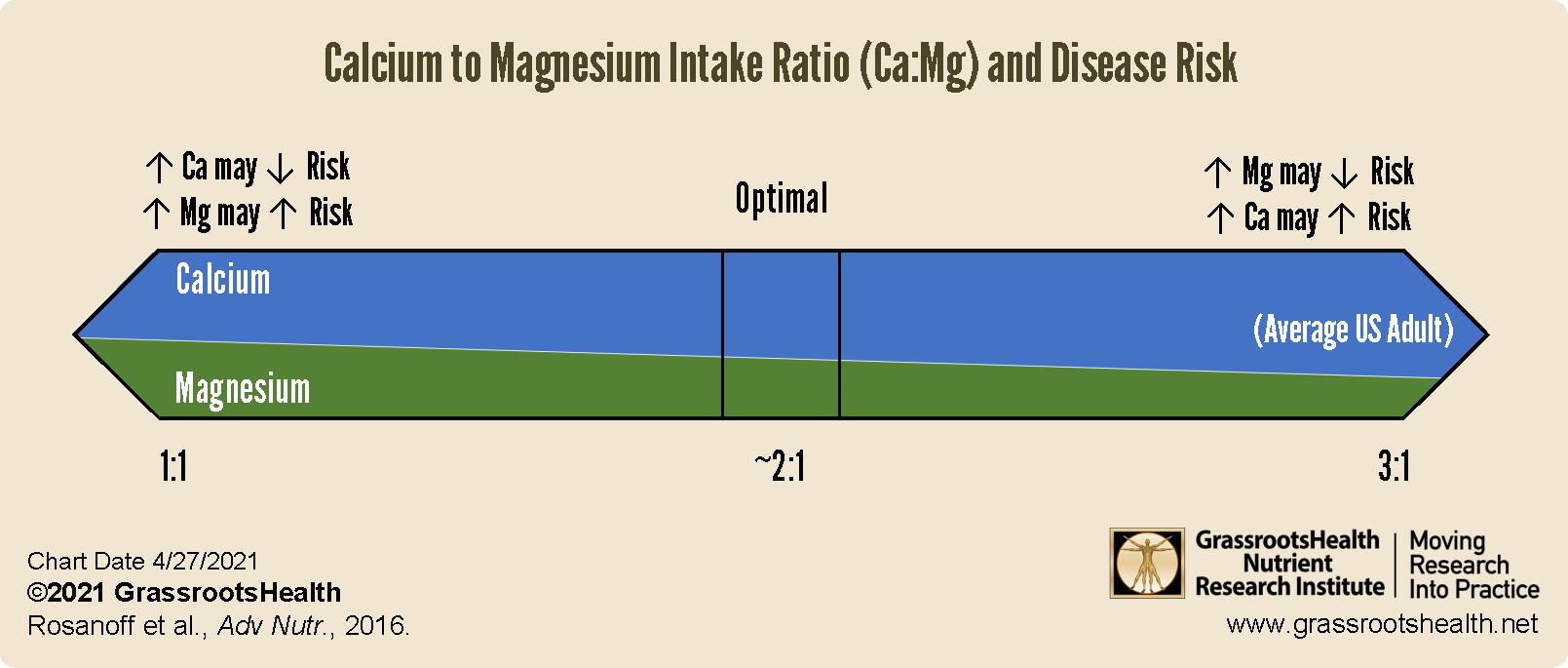
When this happens may be dependent on the Ca:Mg of each individual, which seems to have an effect on the results of several studies looking at calcium and magnesium intake and specific health outcomes. One study on colorectal cancer in the United States found that increased magnesium intake was related to a decreased risk of cancer only among those with a baseline Ca:Mg of less than 2.8. For this group, cancer risk decreased with increased dietary magnesium intake. For those with a Ca:Mg greater than 2.8, dietary magnesium intake did not seem related to risk while an increased dietary calcium intake showed a trend towards greater cancer risk. A follow up study showed that long-term calcium supplementation significantly reduced the risk of colorectal cancer only among those with a baseline Ca:Mg intake of less than 2.6, with no effect on cancer risk when the baseline ratio was higher.
Another study showed that increasing magnesium intake among those with Ca:Mg of less than 2.0 may actually increase the risk of disease when calcium is not also increased. For example, a large population study in China, where calcium intake is low on average, showed that those who took 320 mg per day or more of magnesium and had a baseline Ca:Mg intake of 1.7 or less had an increased risk of all-cause mortality, mortality due to cardiovascular disease, and colorectal cancer among women. In contrast, taking 320 mg per day of magnesium with a baseline Ca:Mg intake higher than 1.7 was significantly associated with decreased risks of total mortality, mortality due to ischemic heart disease among men, and mortality due to all cancers among women. Other study data has shown increased risk of prostate cancer and heart failure with low magnesium and high calcium intake.
In conclusion, the effect of either calcium or magnesium supplementation may be dependent on an individual’s current calcium and magnesium intake ratio, or Ca:Mg, as illustrated below.
What about Vitamin D?
We know that magnesium is an important co-nutrient for vitamin D, and is involved in the biosynthesis, transport, and activation of vitamin D. In fact, studies have shown that poor magnesium status potentially impairs vitamin D metabolism enough to limit the parathyroid hormone (PTH) response, which increases the activation of vitamin D to then increase calcium absorption. Also, an existing magnesium deficiency may result in a vitamin D level that does not increase as much as expected in response to vitamin D supplementation. As illustrated by Deng et al., without sufficient magnesium, the amount of vitamin D that can be metabolized and used by your body is limited and may result in a lack of conversion of vitamin D into its other active forms.
Because magnesium plays critical roles in the synthesis of PTH and in the conversion of vitamin D to 25(OH)D and 1,25(OH)2D, ensuring adequate intake of magnesium is essential, especially when supplementing with vitamin D and conducting nutrient studies on vitamin D.
Ensure Adequate Co-Nutrient Intake, In Research and Always
Dr. Robert Heaney, a leading expert in bone biology, osteoporosis, and human calcium and vitamin D physiology, and past Research Director for GrassrootsHealth, spoke often on the importance of ensuring adequate co-nutrient intake as one of the main criteria for designing nutrient studies. Dr. Heaney provides examples in the link above where differing, and sometimes unexpected, results can come from studies that only look at one nutrient without considering the status of important co-nutrients.
Measure Your Magnesium along with Your Vitamin D Level
The whole blood magnesium test can help give you an idea of your current magnesium status, while also paying attention to including foods in your diet every day that are high in magnesium and calcium. Based on the foods you eat, consider what supplements you may need to include to find your balance of important nutrients.
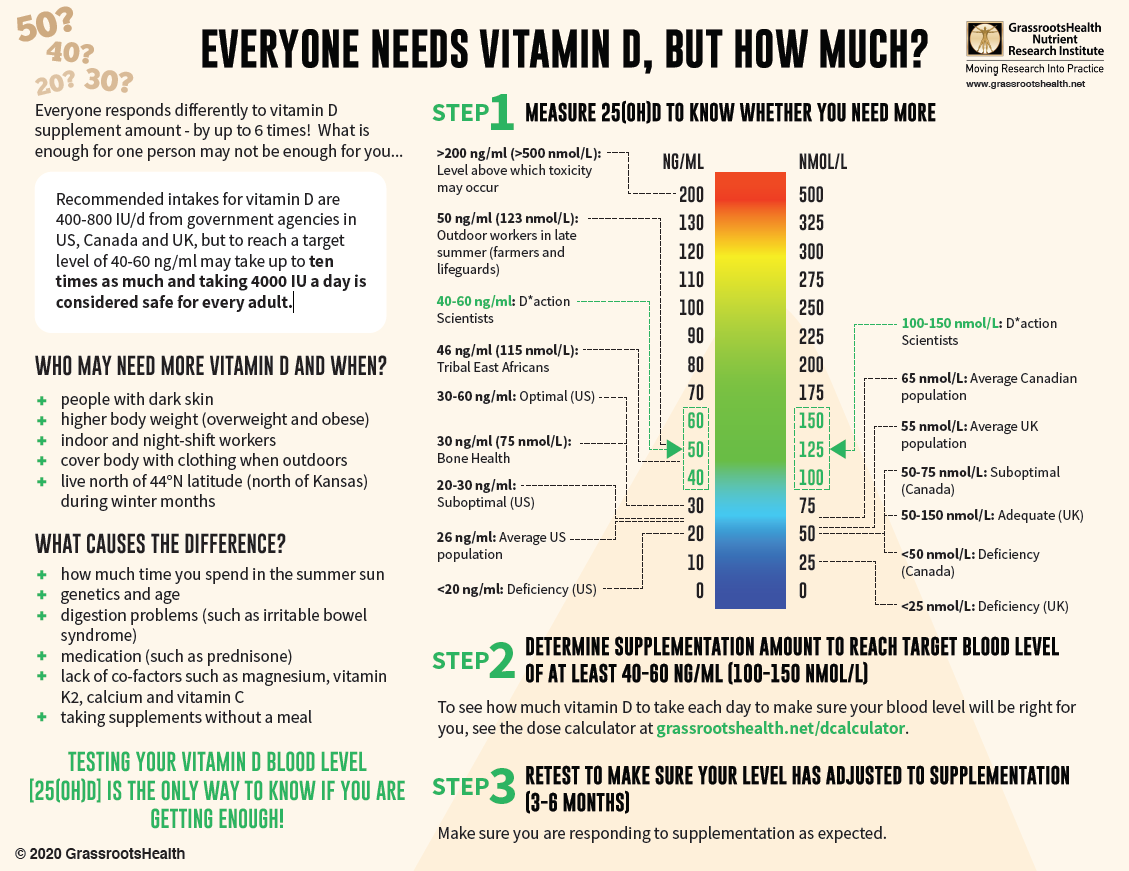
With almost 90% of the general population having vitamin D levels below the recommended 40-60 ng/ml (100-150 nmol/L), it is obvious that most people need more vitamin D. While most of us cannot achieve a vitamin D level of 40-60 ng/ml from sun alone, either due to our lifestyle, where we live, or other circumstances, we can certainly reach those levels with the right amount of supplementation.
Below is a guide for how much you might need, and who may need more. Your levels can be tested safely at home – order your home test kit today.
By joining the GrassrootsHealth projects, you are not only contributing valuable information to our study, but you are also gaining knowledge about how you could improve your own health through measuring and tracking your nutrient status, and educating yourself on how to improve it. Do you know what your status of vitamin D, omega-3s, and other essential nutrients is? Could your levels be improved? Test now to find out!