Published on January 28, 2021
What to consider when headlines claim no benefit for vitamin D in bone health, falls and fractures
 Whenever a study comes out that questions the known benefits of vitamin D the press reports it ad nauseam, and the results are over-interpreted and misconstrued in sensational headlines. One study in particular is almost always referenced to show that vitamin D may not prevent falls (details below). It is time to make sure we know the facts – not the hyperbole.
Whenever a study comes out that questions the known benefits of vitamin D the press reports it ad nauseam, and the results are over-interpreted and misconstrued in sensational headlines. One study in particular is almost always referenced to show that vitamin D may not prevent falls (details below). It is time to make sure we know the facts – not the hyperbole.
Where does this claim come from?
The paper from Bischoff-Ferrari, et al. reported on 200 home-dwelling men and women, over the age of 70 years, in Zurich, Switzerland. One purpose of the study was to assess whether vitamin D prevented falls in the elderly. The participants were divided into three groups which received monthly doses of vitamin D: 24,000 IU; 60,000 IU; or 24,000 IU of vitamin D3 plus 300 μg of calcifediol (25-Hydroxyvitamin D3).
Previous research studies on vitamin D and the elderly have found that a higher level of vitamin D prevented falls and that fall reduction is associated with vitamin D blood levels above 30 ng/ml. But the results of this study were different. They found that while all groups increased their vitamin D levels, the higher vitamin D supplement groups, and those who achieved the highest 25(OH)D status, had more falls than the lowest group.
The authors did not conclude that vitamin D supplementation would not prevent falls or fractures.
Bischoff-Ferrari stated in the discussion section of the paper,
the physiology behind a possible detrimental effect of a high monthly bolus dose of vitamin D on muscle function and falls remains unclear and needs further investigation.
Also, the conclusion of the paper was not that vitamin D would not help seniors (something erroneously reported in many headlines), but that high monthly bolus dosing was not the right approach. Instead, the authors propose creating a new study using daily dosing.
In Defense of Vitamin D
While the paper from University Hospital Zurich received a lot of press, the results of the trial did not surprise us at GrassrootsHealth. More information is now known about the importance of daily dosing versus monthly dosing than was known at the time the study started. In order to prevent falls, you need strong muscles in addition to strong bones. For vitamin D to be effective in aiding muscle strength, stability and for general disease prevention, it is better to take it daily – not monthly.
Also extremely important is to measure the vitamin D level to make sure the daily dose is enough to have an effect, such as that found in a 2019 study that compared vitamin D levels (not intake) to bone quality and fracture risk. Both bone mineral density and the risk of fracture were significantly related to vitamin D level.
Effective vs. Ineffective Clinical Trials
Robert Heaney, MD, spent much of his career doing research on vitamin D and other nutrients and published a paper with guidelines for nutrient studies. Below is a chart which lists the guidelines he recommends for an optimum nutrient study and an analysis of how this Zurich study measured up.
| Nutrient Study Guidelines | Bischoff-Ferrari Study |
|---|---|
| 1. Basal nutrient status must be measured, used as an inclusion criterion for entry into study, and recorded in the report of the trial. | QUESTIONABLE Baseline 25(OH)D levels were measured and reported but were not used as inclusion criterion (58% were <20 ng/ml at baseline). Some analyses were limited to those with baseline levels <20 nmg/ml (but these analyses compared treatment groups, not achieved serum level groups). |
| 2. The intervention (i.e. change in nutrient exposure or intake) must be large enough to change nutrient status and must be quantified by suitable analyses. | DID MEET (WITH NOTES) There were three groups: 24000 IU/month (about 800 IU/day; control group), 60000 IU/month (about 2000 IU/day), and 24000 IU/month and 300 microgram/month calcifediol. These dose amounts were large enough to produce a change in nutrient status. Notes: While not measured with 25(OH)D, infrequent dosing of the parent coumpound, D3, may have influenced the results. |
| 3. The change in nutrient status produced in those enrolled in the trials must be measured and recorded in the report of the trial. | DID MEET 25(OH)D concentrations were measured and recorded at 6 and 12 months. |
| 4. The hypothesis to be tested must be that a change in nutrient status (not just a change in intake) produces the sought-for-effect. | DID MEET While the hypothesis was that higher monthly doses of vitamin D would reduce the risk of functional decline, findings were also reported by achieved serum level. |
| 5. Co-nutrient status must be optimized in order to ensure that the test nutrient is the only nutrition-related, limiting factor in the response. | QUESTIONABLE Data about other nutrients do not appear to have been collected or reported (e.g. calcium, magnesium, vitamin K, etc...). |
Reading all the Research and Applying the Guidelines for Nutrient Studies
Another paper (a meta-analysis) by Zhao, et al. received similar attention by the media, with claims that vitamin D did not prevent fractures. The authors analyzed data from 33 papers that met certain criteria (in this case randomized controlled trials using vitamin D, calcium, or both to test reduction in fractures for older adults). Of the 33 papers, 24 had participants take vitamin D or both vitamin D and calcium (9 studies used calcium supplements only). All the papers included were listed in a table, with a short summary of dosing, initial vitamin D level (if measured), and length of study (as well as a few other parameters) – all very important to consider for nutrient studies.
Let’s start by throwing out all the bolus dosing – or at least analyzing them separately
As explained in the above example, bolus dosing of vitamin D (especially anything more than weekly) is not the best way to get vitamin D, and studies using bolus dosing are more likely to have null or even negative results. It’s simply not the ‘natural’ way to get vitamin D. Here is a longer explanation that includes research by Dr. Bruce Hollis on the importance of daily dosing.
There were 8 trials on the list that had bolus dosing, one that gave 500,000 IU once a year! Now we are down to 16 papers.
Throwing out the trials that are too short
Why do we have to throw out those that are too short? It takes about two months for vitamin D levels to reach a steady state after a change in supplementation and longer for it to have an appreciable effect on the skeletal system. For the sake of this discussion let’s assume anything under a year is not long enough to show reliable results related to muscle or bone health, which eliminates another 4 studies on the list. Now we are down to 12 papers.
Throw out the trials with too little of a daily dose
One of the most important criteria for a trial to be reputable is for it to show a change in nutrient status – in other words, if vitamin D levels do not change appreciably we would not be able to have an effect. We know that the current RDA for vitamin D of 600-800 IU/day is not enough to make a measurable change, so let’s throw out the studies with less than 1000 IU/day.
This gets rid of all the calcium+vitamin D trials and 4 of the vitamin D alone trials and leaves us with one trial, BEST-D trial by Hin et al, 2017. The quick summary of this trial is that they gave 4000 IU/day, 2000 IU/day or placebo for one year to 305 white people, 65 years or older, in the UK. They found that 4000 IU/day was most effective in reaching optimal vitamin D levels of 40-60 ng/ml (100-150 nmol/L) and that there were NO ADVERSE EFFECTS. In other words, it was safe. They had no conclusions on fracture rates and bone health because they thought their trial was too short for that analysis but instead wanted to use this data to have a multi-year study with older people using 4000 IU/day and testing for fracture rates.
Well, that puts a damper on the headlines.
The Devil is in the Details
The moral of this story is that you can’t trust headlines. In effect, these studies were not very conclusive at all. None of the papers were strong enough to make a conclusion either way.
What most people see in the headlines, due to JAMA’s press release, notice the similarities:
Vitamin D, calcium supplements may not lower fracture risk
Reuters
Lisa Rapaport
December 26, 2017
Read News Article
Calcium and vitamin D supplements may not protect against bone fractures
Washington Post
Ariana Eunjung Cha
December 26, 2017
Read News Article
Vitamin D and Calcium Don’t Prevent Bone Fractures
The New York Times
Nicholas Bakalar
December 28, 2017
Read News Article
Two headlines that got it right, thank you!
Experts rebuke report casting doubt on link to bone health
Omaha World-Herald
Rick Ruggles
December 28, 2017
Read News Article
Industry Criticizes New Study Challenging Benefits of Calcium and Vitamin D
WholeFoods Magazine
Staff
December 26, 2017
Read News Article
Make sure you are getting enough vitamin D and other important nutrients
By joining the GrassrootsHealth projects, you are not only contributing valuable information to our study, but you are also gaining knowledge about how you could improve your own health through measuring and tracking your nutrient status, and educating yourself on how to improve it. Do you know what your status of vitamin D, omega-3s, and other essential nutrients is? Could your levels be improved? Test now to find out!
 We now have a NEW GIFTING SERVICE that allows you to quickly send ‘Gift Cards’ to friends, family and coworkers who you consider might need immediate access to testing, and to Claim the Joy of Your Health TODAY. Give the gift today!
We now have a NEW GIFTING SERVICE that allows you to quickly send ‘Gift Cards’ to friends, family and coworkers who you consider might need immediate access to testing, and to Claim the Joy of Your Health TODAY. Give the gift today!
What does the Research Say about Vitamin D & COVID-19?
It’s TIME to start saving lives! If you can help PREVENT the majority of the death, it’s time! What’s it costing you/us not to take action NOW?
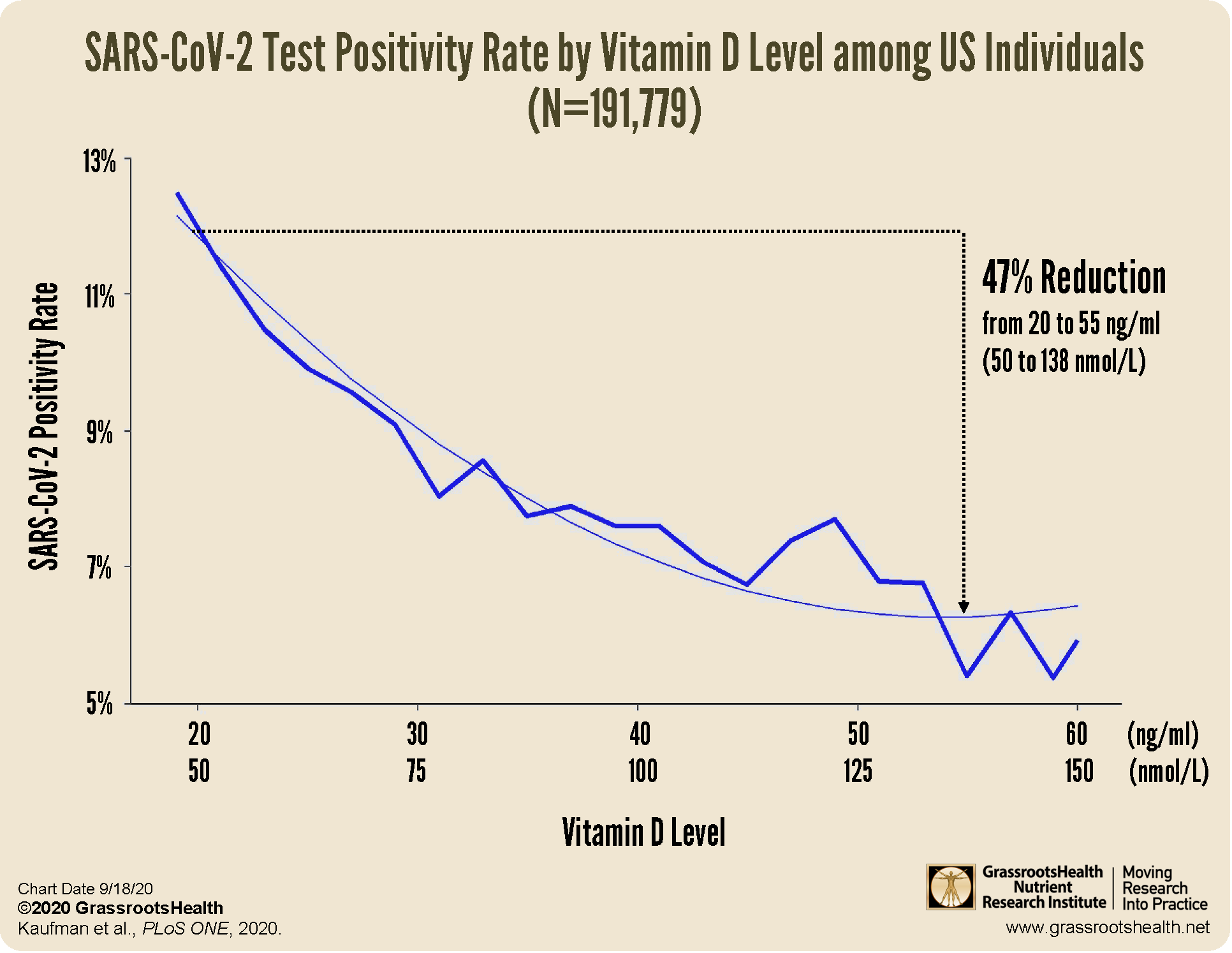
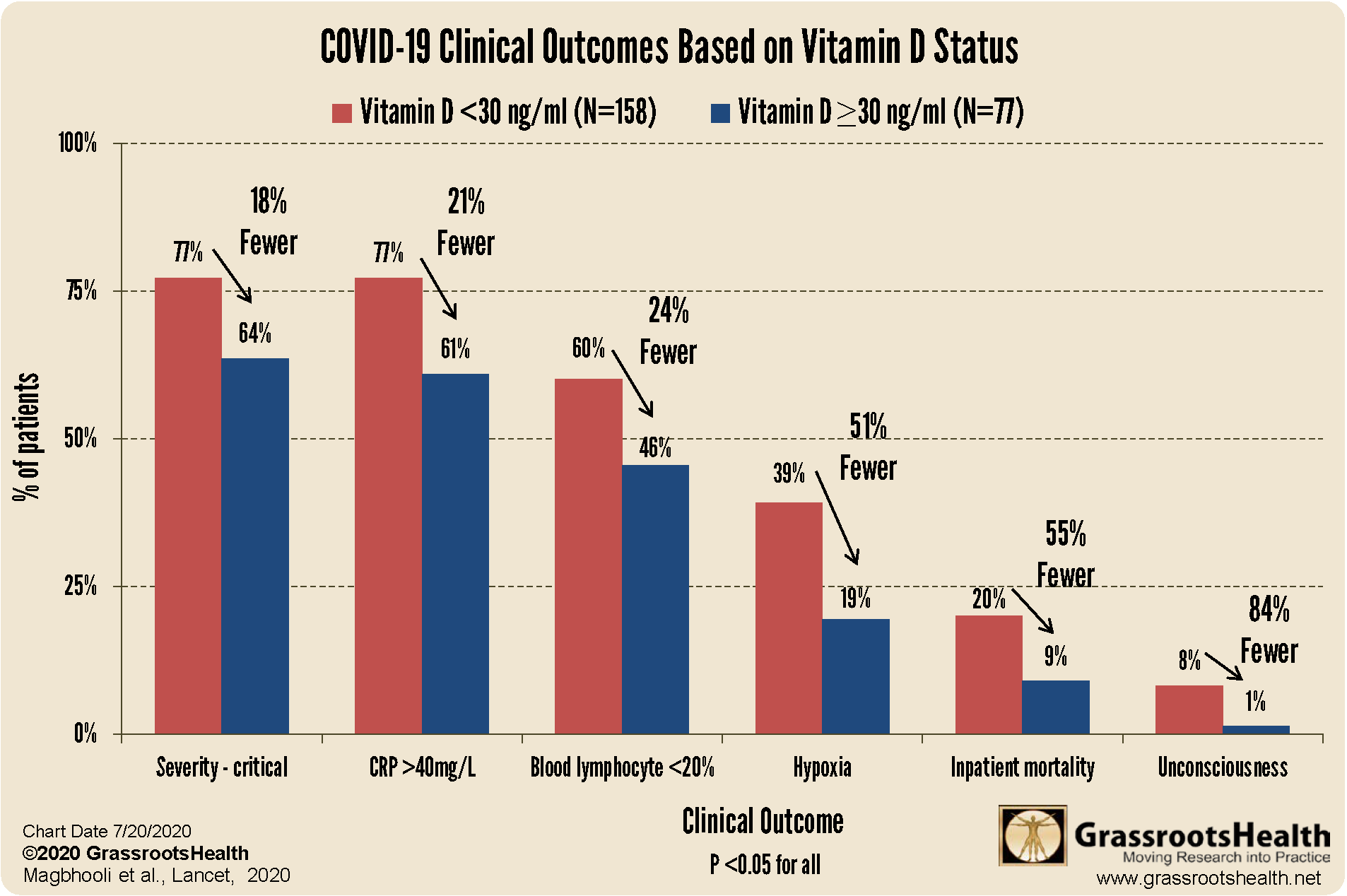
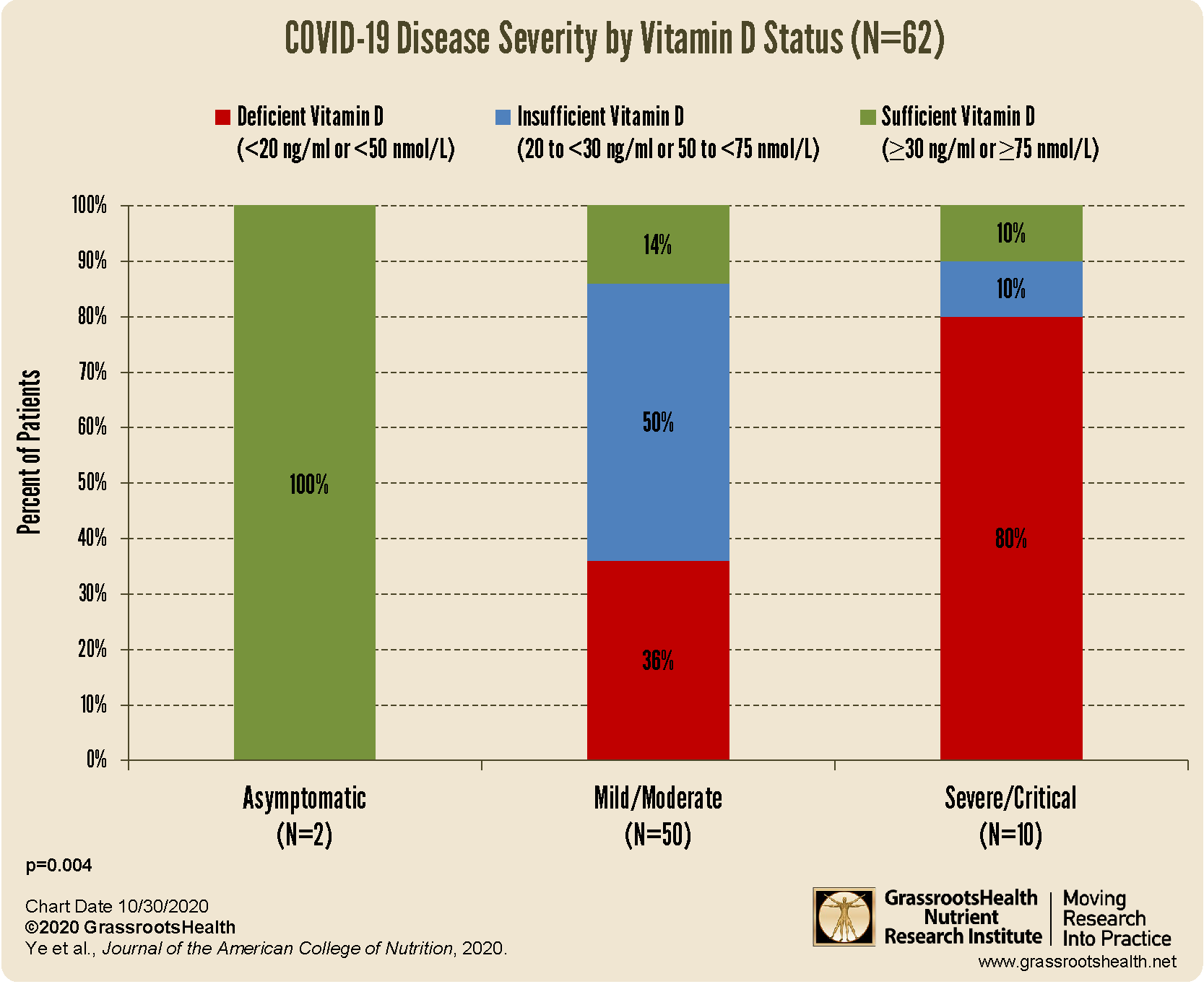
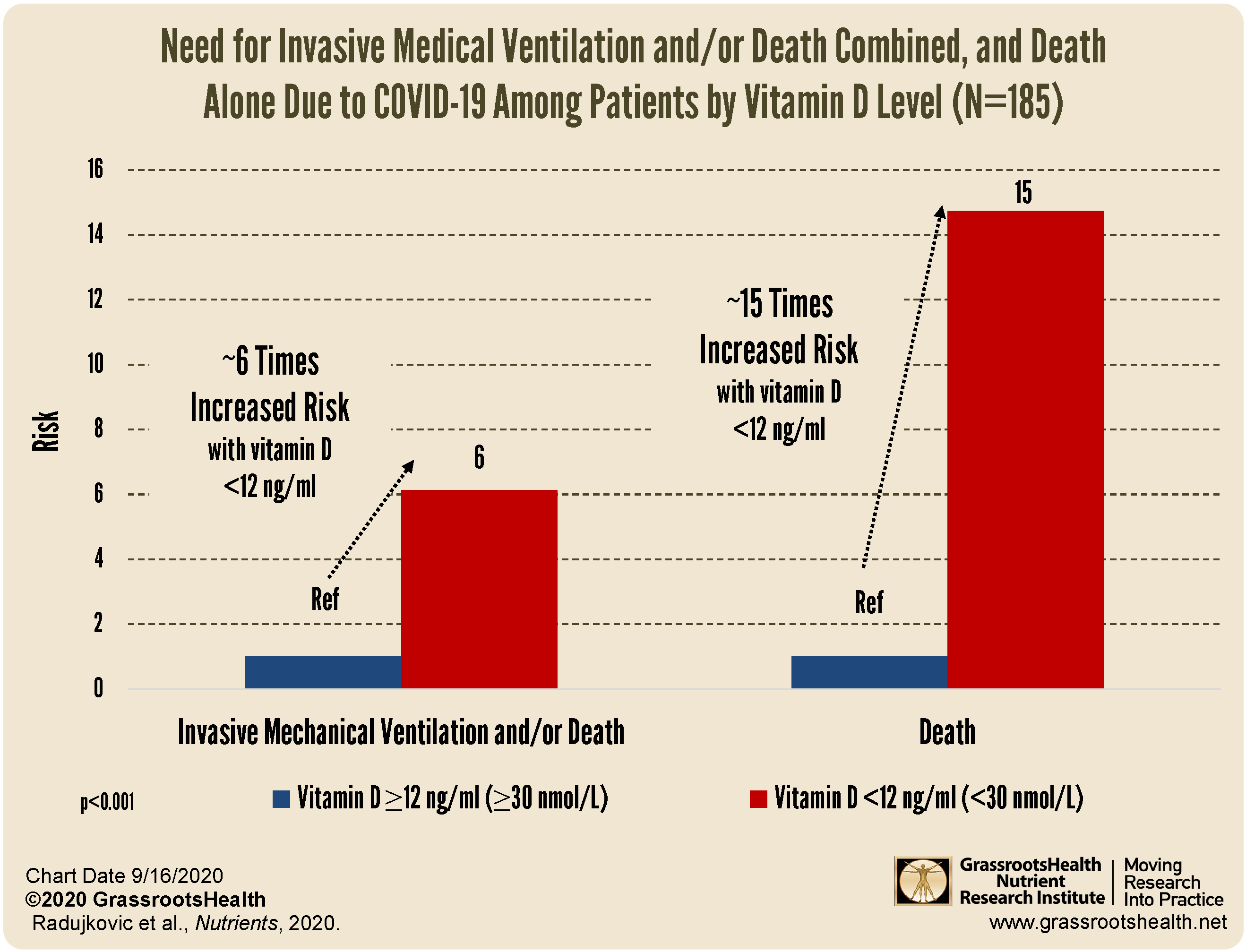
There is much published research that supports a clear link between vitamin D and COVID-19 showing that higher vitamin D levels are related to:
a decreased risk of testing positive for COVID-19
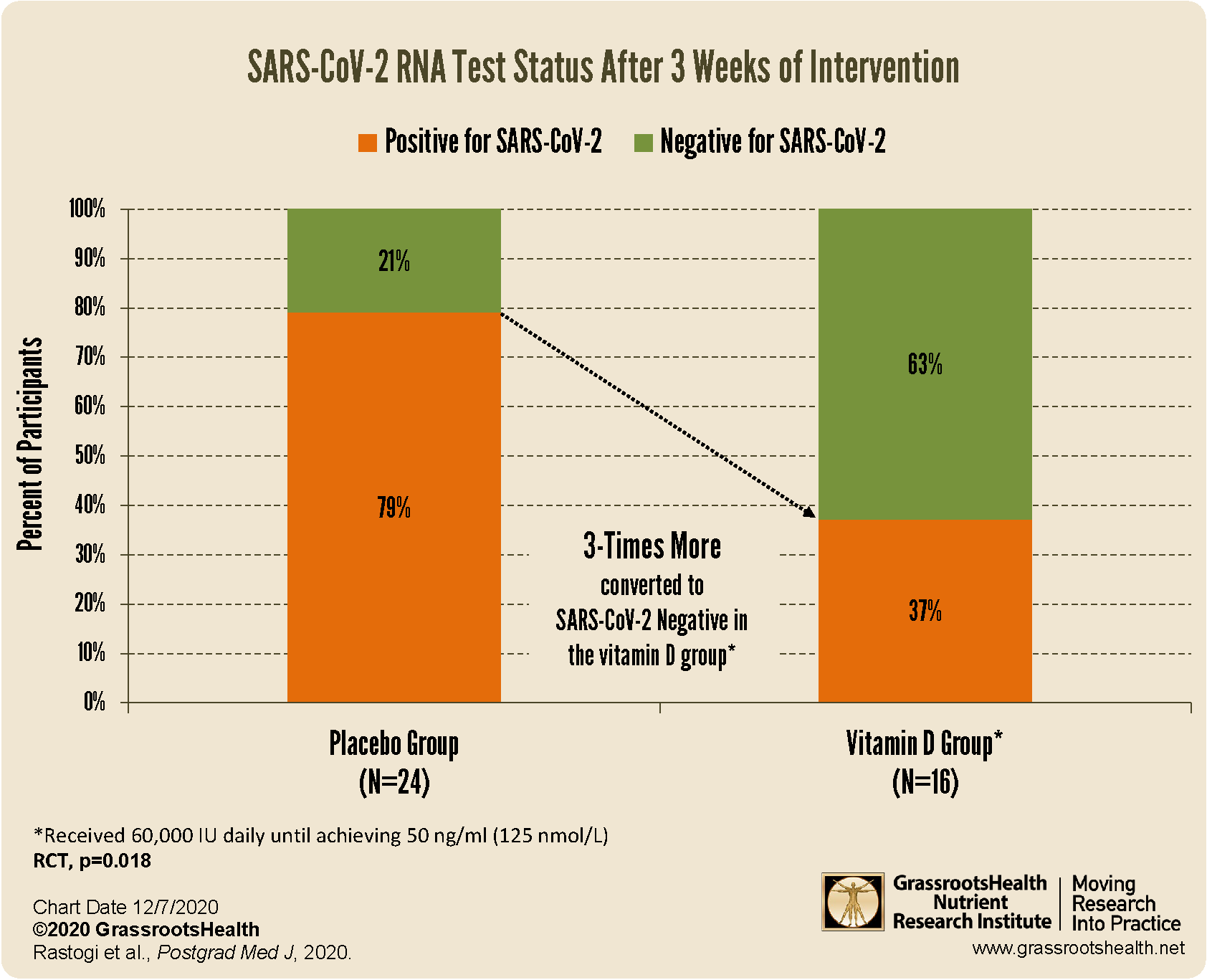 increased viral SARS-CoV-2 RNA clearance
increased viral SARS-CoV-2 RNA clearance
better clinical outcomes among patients with COVID-19
decreased risk of death due to COVID-19
Be sure to educate yourself on the benefits and importance of vitamin D for immune health, and take steps to ensure you and your loved ones are getting enough.
You can review all of the COVID-19 and immune health information we have shared on this page.