Published on June 11, 2020
Some of our recent posts have discussed the topics of vitamin D toxicity and the importance of managing other existing nutrient deficiencies when taking vitamin D. While we will continue with our vitamin D myth busting series, some of our upcoming posts will instead focus on several rare but very real situations in which individuals with certain conditions may experience what seems to be a hypersensitivity to vitamin D supplementation, and sometimes, to the sun as well.
Primary hyperparathyroidism is one such condition that may become “unmasked” upon supplementation with vitamin D.
What is Primary Hyperparathyroidism (PHPT)?
 Primary hyperparathyroidism (PHPT) is the hyper-functioning of one or more of the parathyroid glands, usually due to some type of tumor, and resulting in increased and uncontrolled secretion of parathyroid hormone (PTH). This in turn leads to hypercalcemia and other toxic imbalances, with symptoms such as increased urination, dehydration, constipation and weight loss.
Primary hyperparathyroidism (PHPT) is the hyper-functioning of one or more of the parathyroid glands, usually due to some type of tumor, and resulting in increased and uncontrolled secretion of parathyroid hormone (PTH). This in turn leads to hypercalcemia and other toxic imbalances, with symptoms such as increased urination, dehydration, constipation and weight loss.
While the annual incidence of hypercalcemia is only about 0.1-0.2%, PHPT is the most common cause, with 80-85% of PHPT due to adenoma (a single, benign tumor causing an enlarged parathyroid gland).
Approximately 60-80% of individuals with PHPT are asymptomatic, and their condition is mainly discovered with mild hypercalcemia diagnosed through routine laboratory testing. Up to a quarter (20-25%) of individuals with PHPT may experience intermittent hypercalcemia with symptoms such as recurrent kidney stones. Only 5-10% have severe, symptomatic hypercalcemia with a large tumor and further kidney and bone involvement.
What is the role of vitamin D in PHPT?
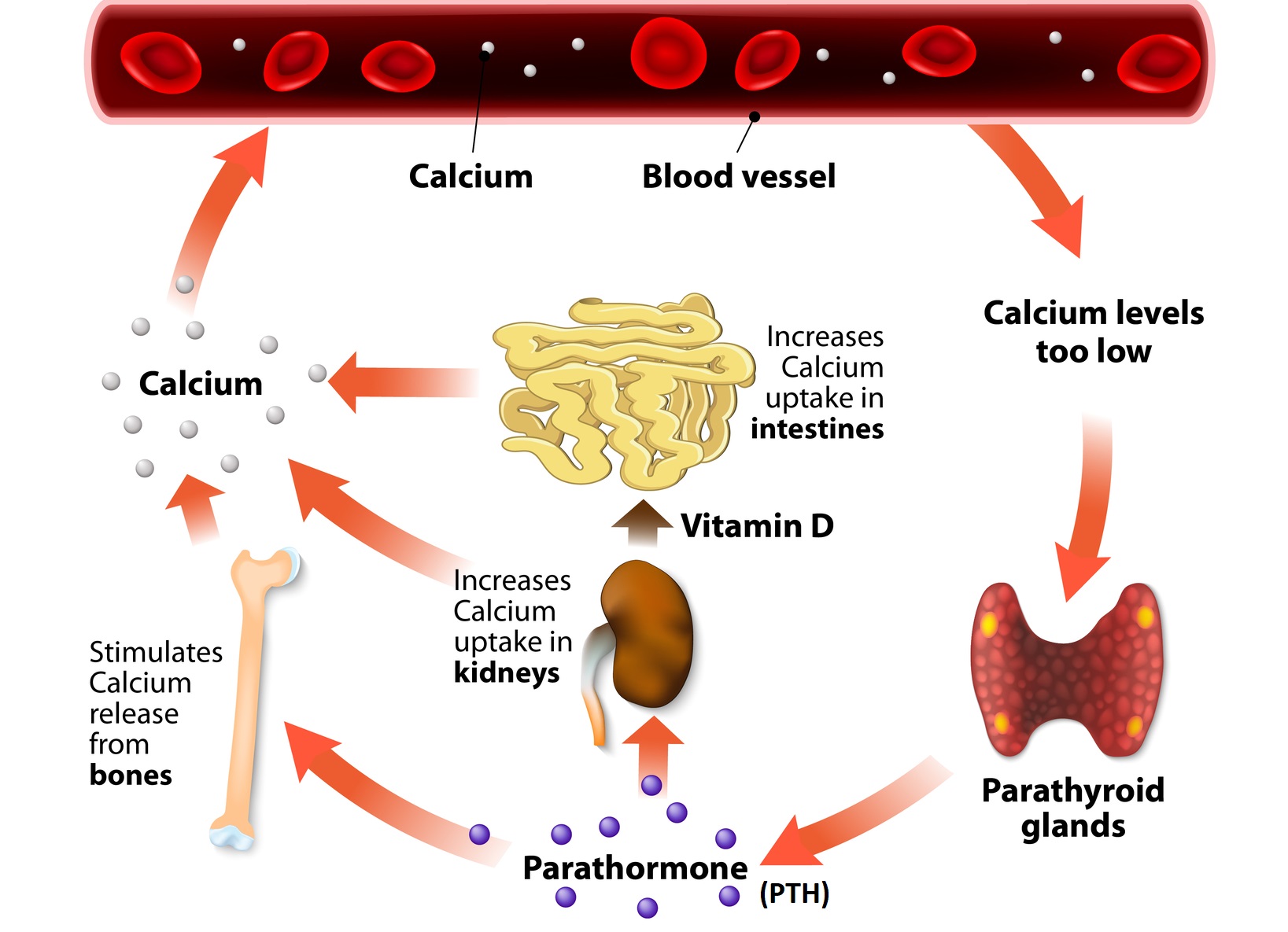
Vitamin D works in balance with the parathyroid to help regulate calcium levels in the blood. Low calcium levels (caused by either low Ca or D) causes PTH to rise, which increases the activation of vitamin D to then increase Ca absorption from the gut and reabsorption from the bone. The increased calcium then circles back to lower PTH, turn off vitamin D and maintain a steady balance.
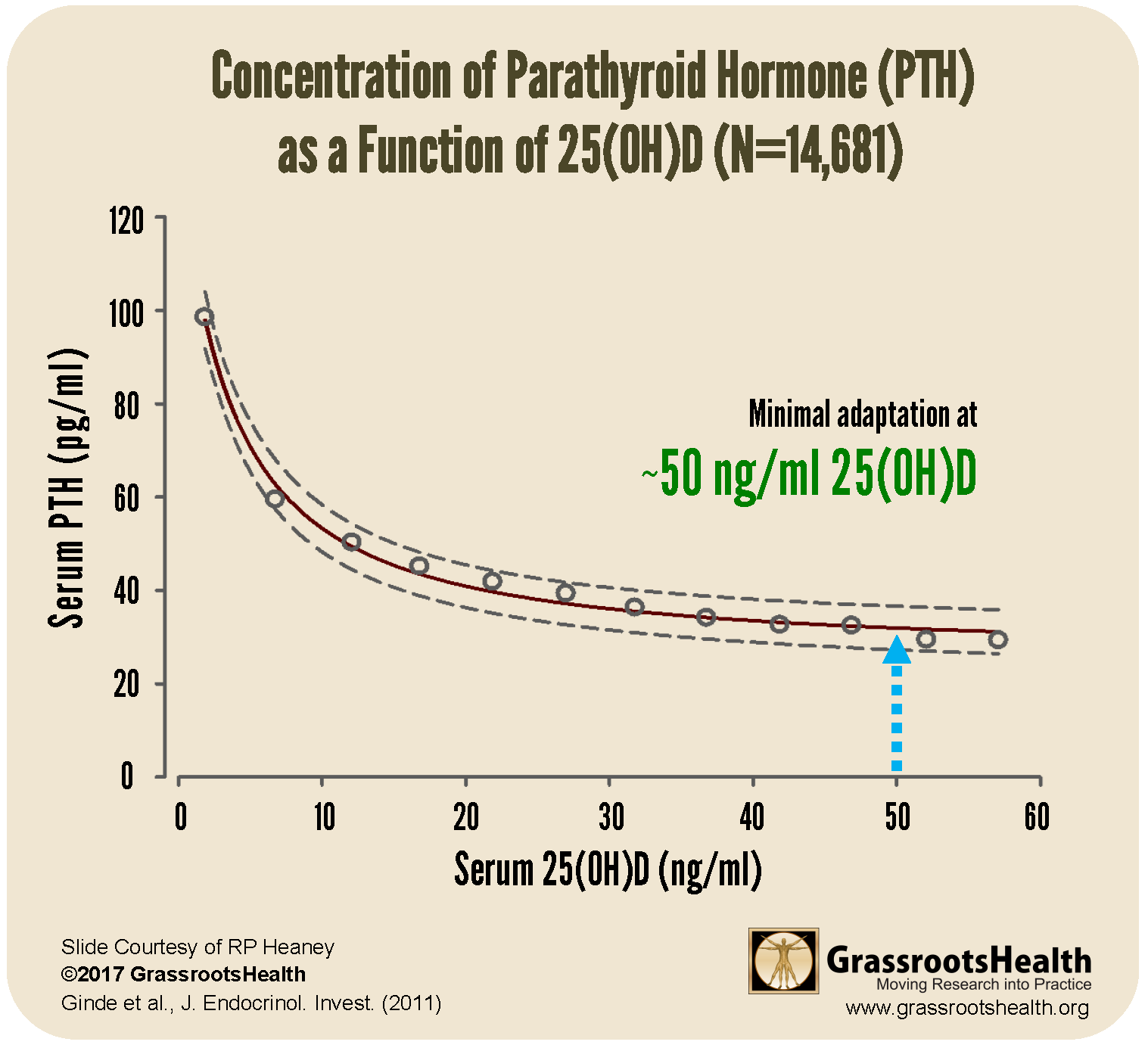
In the absence of PHPT, the relationship between vitamin D levels and PTH can be seen in the chart below. When vitamin D levels are optimal, at a level of about 50 ng/ml, parathyroid hormone does not need to compensate for low vitamin D. This provides a situation of minimal adaptation for parathyroid function.
When PTH rises uncontrollably, such as in PHPT, vitamin D’s action on calcium absorption also becomes uncontrolled, leading to abnormally high levels of calcium, or hypercalcemia. In a situation where an individual has underlying and asymptomatic PHPT, it is possible that vitamin D supplementation may “unmask” the condition by triggering more severe hypercalcemia and resulting in symptoms.
Catch 22
Unfortunately, most individuals with PHPT tend to be vitamin D deficient or insufficient as well, leading to an increased need for vitamin D supplementation. One case study demonstrated the severe negative effects of the combination of vitamin D deficiency and PHPT on bone. A study by Grey et al. involving 25 PHPT patients found that vitamin D supplementation resulted in lower PTH levels and decreased bone turnover, and suggests a protective effect of vitamin D against PHPT progression and severity.
What’s the take-away? Vitamin D supplementation may unmask a previously asymptomatic case of PHPT, leading to symptoms and the potential for hypercalcemia. In individuals with PHPT, it is still very important to get enough vitamin D to maintain a blood level between 40-60 ng/ml, however, working with a health care provider may be advised to ensure toxicity does not become an issue.
If you feel you may have this condition, or if you experience what feels like a hypersensitivity or negative effects due to vitamin D, please work with your health care provider to address potential underlying conditions, and work with them to safely resolve any existing vitamin D deficiency.
Is it True?
Our “Vitamin D Myths” series will continue to provide information and resources to answer the question, “Why should I care about vitamin D?” and to help dispel the myths and misconceptions surrounding it that may be preventing you and others from accepting it as an essential component to health. We will also discuss other nutrients essential to the function of vitamin D (and vice versa) within the body that should not be ignored.
Vitamin D is necessary for multiple functions within the body and should not be ignored, but has the hype about vitamin D and its role in the body’s response to COVID-19 been over-exaggerated? What concerns about vitamin D are valid, and which are not? We want to provide you with evidence-based information to help you decide what vitamin D action to take, if any, for your own health.
We want to hear from you!
Is there a particular ‘myth’ you have heard about vitamin D? Or, something you have read or been told that makes you question whether vitamin D ‘deserves’ so much attention? Or whether you should be taking it and how much? Share with us by emailing jen @grassrootshealth.org what you have heard that makes you question vitamin D so that we can consider addressing it in our newsletters.
Do You Have Enough Vitamin D to Support a Healthy Immune System?
Do you know what your vitamin D level is? Be sure to test today to find out, and take steps to keep it within a target of 40-60 ng/ml or 100-150 nmol/L! Give your immune system the nutrients it needs to support a healthy you and protect yourself from unnecessary diseases.
Through GrassrootsHealth Nutrient Research Institute, you can also test your essential elements magnesium, copper, zinc and selenium, toxins such as lead, mercury and cadmium, as well as your omega-3 levels, inflammation levels and thyroid stimulating hormone (TSH) level. Find out your levels today! Log on to the test selection page (click the link below) to get your tests and see for yourself if your levels can be improved.
Make sure you track your results before and after, about every 6 months!
How can I track my nutrient intake and levels over time?
To help you track your supplement use and nutrient levels, GrassrootsHealth has created the Personal Health Nutrient Decision System called
For each specific supplement, you can track what days you take it, how much, and many other details. This will help you know your true supplemental intake and what patterns of use work for you to reach and maintain optimum nutrient levels. Check it out today!