Published on November 28, 2023
Prof. Sunil Wimalawansa elaborates on the safety of vitamin D and avoiding adverse effects, including types of individuals who may need to be more cautious about taking higher doses and concerns about co-nutrients. (Interview Series Part 5)
A 5-Part Interview Series with Dr. Sunil Wimalawansa
Part 1 Vitamin D: Everything You Need to Know… and More: An introduction to Dr. Wimalawansa along with details focusing on his experience with vitamin D in the clinical and scientific setting
Part 2 Defining Optimal Levels and Doses of Vitamin D for Every Individual: Answers to questions about optimal vitamin D levels and doses and how they may differ for certain individuals
Part 3 Understanding the Forms of Vitamin D: Vitamin D3, 25(OH)D, and 1,25(OH)2D:A detailed description of the forms vitamin D3, 25(OH)D, and 1,25(OH)2D and when each might be considered for measurement
Part 4 How Does One Determine the Right Amount and Type of Vitamin D to Take?: Calculating the correct amount of vitamin D to take and when certain forms of supplementation should be considered
Part 5 Vitamin D Safety and Adverse Effects – When Should Caution Be Advised?: Our final post for this series of questions-and-answers with Dr. Wimalawansa on vitamin D safety and toxicity
Key Points (Part 5)
- Vitamin D toxicity should not be diagnosed in isolation; relying only on a specific serum concentration of 25(OH)D for diagnosis is a fallacy
- There are a few conditions to be cautious of exposure to sunlight: those who are hyperreactive or hypersensitive to sunlight; examples are lupus erythematosus/syndromes (SLE) and genetic disorders like Williams syndrome (hypersensitive to vitamin D); also, those with chronic granulomatous diseases like sarcoidosis and tuberculosis could produce high amounts of calcitriol causing hypercalcemia
- For those taking vitamin D supplements, there is no reason to take calcium supplements, as intestinal calcium absorption will increase automatically, especially for those taking higher doses, as discussed below
- For several reasons discussed below, many require additional supplemental cofactors, like or including vitamins A, C, B2, and K2, magnesium, zinc, boron, and others for fully functioning enzymes and immune systems
 Dr. Sunil Wimalawansa has been researching vitamin D for over four decades and is considered one of the world’s leading experts on micronutrients, especially vitamin D. His extensive background includes working with vitamin D in the laboratory setting, applying his vitamin D knowledge, working with patients as a medical doctor, and directing clinical trials involving vitamin D.
Dr. Sunil Wimalawansa has been researching vitamin D for over four decades and is considered one of the world’s leading experts on micronutrients, especially vitamin D. His extensive background includes working with vitamin D in the laboratory setting, applying his vitamin D knowledge, working with patients as a medical doctor, and directing clinical trials involving vitamin D.
We introduced Dr. Wimalawansa in Part 1 of this interview series, Vitamin D: Everything You Need to Know… and More, and shared his answers to questions about optimal vitamin D levels and doses and how they may differ for certain individuals in Part 2, Defining Optimal Levels and Doses of Vitamin D for Every Individual. We followed these with a detailed description of the forms vitamin D3, 25(OH)D, and 1,25(OH)2D and when each might be considered for measurement in Part 3, Understanding the Forms of Vitamin D: Vitamin D3, 25(OH)D, and 1,25(OH)2D and discussed calculating the correct amount of vitamin D to take and when certain forms of supplementation should be considered in Part 4 How Does One Determine the Right Amount and Type of Vitamin D to Take?.
Today is our final post for this series of questions-and-answers with Dr. Wimalawansa on vitamin D safety and toxicity.
Questions and Answers with Dr. Sunil Wimalawansa: Vitamin D Doses, Toxicity, and Safety
Let us now discuss the adverse effects of vitamin D—What are the criteria for diagnosing vitamin D toxicity?
 Vitamin D toxicity should not be diagnosed in isolation—incidental findings of elevated serum 25(OH)D concentrations do not equate to toxicity. Toxicity is possible when levels exceed and are maintained above 150 ng/mL (over 375 nmol/L) and are associated with clinical signs and symptomatology of hypercalcemia. Characteristics of the calcitriol-driven hypercalcemic syndrome include hypercalcemia (raised serum “ionized” calcium), hypercalciuria (urinary calcium exceeding 400 mg/24 hours) and suppressed parathyroid hormone (PTH) concentration. All three components must be present to diagnose vitamin D toxicity. Notably, tolerance to higher circulatory 25(OH)D markedly varies between people. Therefore, relying on a specific serum concentration of 25(OH)D to diagnose vitamin D toxicity is a fallacy.
Vitamin D toxicity should not be diagnosed in isolation—incidental findings of elevated serum 25(OH)D concentrations do not equate to toxicity. Toxicity is possible when levels exceed and are maintained above 150 ng/mL (over 375 nmol/L) and are associated with clinical signs and symptomatology of hypercalcemia. Characteristics of the calcitriol-driven hypercalcemic syndrome include hypercalcemia (raised serum “ionized” calcium), hypercalciuria (urinary calcium exceeding 400 mg/24 hours) and suppressed parathyroid hormone (PTH) concentration. All three components must be present to diagnose vitamin D toxicity. Notably, tolerance to higher circulatory 25(OH)D markedly varies between people. Therefore, relying on a specific serum concentration of 25(OH)D to diagnose vitamin D toxicity is a fallacy.
Especially considering vitamin D is economical and cost-effective, is a widely available generic agent that does not need a prescription, can be taken without measuring (expensive) serum 25(OH)D levels, and has no adverse effects on “recommended amounts,” wider use is reasonable. Also, considering 75% of the world population either has no access to or cannot afford to measure blood levels of vitamin D [25(OH)D]. Despite that, vitamin D dose can be calculated using the body weight or the BMI; tables for calculating vitamin D amounts are published in the following free research paper: DOI: 10.3390/nu14142997 or by using the Vitamin D*Calculator.
Is there a vitamin D intake or level that you consider too high, and when might toxicity become a concern?
Hypercalcemic syndrome secondary to overdoses of vitamin D supplements is exceedingly rare. Such is due to taking very high, supra-pharmacological doses of vitamin D mistakenly or too frequently.
Sporadic reports (social media) have spread misinformation about the lack of effects of vitamin D and exaggerated toxicity. These sponsored or ignorant writings are designed to mislead, and scaremongers have no scientific basis and should be ignored and countered. There is no evidence of toxicity with the recommended doses, such as intakes up to 7,000 IU/day or 50,000 IU/week in a 70 kg non-obese adult, even though in some, it can lead to serum 25(OH)D concentrations up to 100 ng/mL. Such will not be associated with clinical signs and symptoms or laboratory indicators of hypercalcemia. Nevertheless, when the level exceeds 80 mg/mL, taking vitamin K2 (MK7) 100 µg a day or 800 µg/week is recommended.
In obese people and those with gastrointestinal fat malabsorption, daily doses of up to 25,000 IU cause no such adverse effects (DOI: 10.3390/biomedicines11061542). Besides gastrointestinal fat abruption issues, other groups also require higher doses of vitamin D, like familial or genetically inherited vitamin D resistance, and those with autoimmune disorders like multiple sclerosis require much higher daily doses of vitamin D for better health.
Have your patients ever experienced unpleasant side effects from vitamin D supplementation? If so, what was the usual reason, and how was it addressed? Could all your patients take vitamin D without experiencing any adverse side effects?
As a practicing clinician who routinely used higher doses of vitamin D in needy persons for over four decades, we have yet to see any person developing vitamin D toxicity. In the published literature, there are only about 100 true cases with such toxicity, which illustrates its rarity. Most healthcare workers will never encounter someone with vitamin D toxicity during their careers.
Because of the considerably high safety margin (vitamin D intake versus the potential to develop adverse effects), unless one is eager to document serum 25(OH)D concentration as in academia or research, it is not obligatory to test blood levels of 25(OH)D prior to initiating vitamin D. As discussed, the appropriate dose is easily calculated via two tables published in Nutrients in 2022 (DOI: 10.3390/nu14142997)— and shared in our previous post here, as well as with the Vitamin D*Calculator. This calculation can be done if 25(OH)D concentration is known, OR by using body weight or BMI.
Should certain individuals avoid high-dose vitamin D supplementation; if so, who and why?
There are a few conditions to be cautious of exposure to sunlight: those who are hyperreactive or hypersensitive to sunlight. Examples are lupus erythematosus/syndromes (SLE) and genetic disorders like Williams syndrome (hypersensitive to vitamin D). In the case of Lupus, while these patients are hypersensitive to sunlight, vitamin D is a crucial adjunct therapy. As we discussed previously, because of the lack of feedback control, those with chronic granulomatous diseases like sarcoidosis and tuberculosis (DOI: 10.1359/jbmr.07s221) could produce high amounts of calcitriol causing hypercalcemia.
What are the principles governing the use of vitamin D, including for safety?
Here are some principles healthcare workers need to be aware of when using vitamin D replacement therapy:
- Vitamin D is not a hormone but a threshold nutrient (DOI: doi:10.1111/nure.12090). D3 should be used instead of D2. Pharmaceutical agents have linear dose-responses, but nutrients have curvilinear responses. Clinical responses and adverse effects are directly dose-related.
- In hypovitaminosis D (or insufficiency), maximum benefit occurs over a relatively steep dose-response. Beyond that, no matter how high doses are provided, there will be little or no additional benefits. This principle is crucial for designing amounts to be used in RCTs and clinical practice (DOI: 10.3390/biomedicines11061542)
- As mentioned, as a threshold nutrient, the response to vitamin D is not linear but curvilinear. With increasing doses of vitamin D, a diminution of return (benefits) exists. With calcifediol, a partially activated vitamin D metabolite [25(OH)D], the dose-response is linear, and so is the (theoretical) toxicity.
- Never give vitamin D intramuscular injections. These vitamin D vials contain oil-based liquid, requiring a large needle to administer. In addition to being very painful, it causes granulomas at the site of injection; thus, injecting should be avoided. If such is available, please open the glass vial and give the oily content orally.
- D3, 25(OH)D (calcifediol), and 1,25(OH)2D (calcitriol) have biological functions in increasing order. The half-life of vitamin D3 in the blood is about one day; calcifediol is between two to three weeks, and calcitriol is only a few hours. These compounds circulate in the blood, primarily bound to vitamin D binding protein (VDBP). When treating patients and designing RCTs, these variables must be considered.
- Both vitamin D and calcifediol dose adjustments are based on body weight, as described above (DOI: 10.3390/nu14142997).
- When using higher vitamin D doses (i.e., doses above 7,000 IU/day or 50,000 IU/week), consider using vitamin K2 (MK7: 100 µg daily or 800 µg/week). When taking higher doses, it is advisable to take a low-calcium diet. For those taking vitamin D supplements, there is no reason to take calcium supplements, as intestinal calcium absorption will increase automatically. Those who take high doses of vitamin D should stop taking calcium supplements, including multiple vitamins that contain calcium.
- The two critical metabolites of vitamin D, calcifediol and calcitriol, have specific indications for use, as we previously discussed here. These two metabolites or synthetic analogs should not be used as vitamin D replacement therapy for deficiency.
Will taking vitamin D without supplementing with co-nutrients (especially vitamin K2 and magnesium) be harmful?
This is a complex question. 75% of the immune system functions depend on having (maintaining) enough vitamin D (DOI: 10.2147/PLMI.S373617; DOI: 10.3390/biomedicines11061542). The cofactors mentioned provide the remaining 25% of the immune cell activity necessary for a robust immune system to overcome infections. Magnesium is an essential component for calcitriol receptor interactions; deficiency impairs calcitriol‒receptor and DNA interactions and reduces the biological functions of calcitriol. It is also necessary to release hormones from endocrine cells. It is beneficial to maintain the physiological Ca2+/Mg2+ ratio of about 2.6 (DOI: 10.1186/s40001-023-01162-y).
While the hormonal form of calcitriol produced from renal tubular cells increases serum ionized calcium (Ca2+), K2 is necessary to divert it from soft tissues into skeletal tissues (i.e., it prevents calcium deposition and calcification in soft tissue). Consequently, when higher doses of vitamin D are taken (i.e., doses above 7,000 IU/day and 50,000 IU/week), taking vitamin K2 (MK7) is recommended.
You recently stated, “Maintaining the essential micronutrient ‘cofactors’ (like magnesium, B2, zinc, boron, etc.) and the population’s vitamin D [25(OH)D concentration above 40 ng/mL] is the most effective way to control infections, reduce chronic diseases, and future pandemics.” You have also recommended taking a certain amount of vitamin K2 and a “higher dose” of vitamin D (such as 7,000 IU and higher).
In recent years, imbalanced diets for micronutrients, modern unwholesome dietary constituents like increased consumption of fast food and reduced fresh ingredients-based homemade food, and unhealthy practices (e.g., higher consumption of processed food containing preservatives and saturated and trans-fat) increased the utilization (catabolism) of micronutrients. In conjunction with pollution-associated factors, they increase the prevalence of micronutrient deficiencies, especially vitamin D and other essential cofactors. These micronutrient deficiencies cause dysfunctional and ineffective immune systems. Correction of vitamin D and cofactor deficiencies reverse them.
This mentioned scenario is made worse by the increasing passive indoor lifestyle. The combination increases the requirement for vitamin D, magnesium, etc., and a higher maintained serum 25(OH)D concentration. Most analyses confirmed that maintaining serum 25(OH)D concentrations between 50 to 80 ng/mL facilitates overcoming approximately 99.7% of disorders affecting humans (DOI: 10.3390/nu15173842).
As we previously discussed, during acute illnesses, especially infections, there is a significantly increased utilization of vitamin D, magnesium, and other cofactors. Therefore, replacing them daily during these illnesses is crucial for a rapid recovery and preventing further complications and deaths.
Can you please elaborate on if you have a specific protocol for how to get enough of the essential co-nutrients to take along with vitamin D—what can be achieved through diet alone, and which are best obtained through supplements?
A balanced diet will provide adequate amounts of all micronutrients except vitamin D. Micronutrients are crucial for the physiological functions of enzymes, stabilizers, energy generation, synthesis and release of hormones and beneficial cytokines, and effective receptor interactions. An example of the latter is the interaction of calcitriol with its receptor and its binding to DNA molecules. However, obtaining the right balance and quantities of micronutrient cofactors is increasingly challenging because of unnatural, imbalanced Western diets.
Increased quantities of 25(OH)D and magnesium are consumed during metabolic and immune-related activities and infections. So, replacing them is needed during such scenarios, as in clinical situations and RCTs. The lack of which, as practiced today, delays the recovery with poor clinical outcomes. Therefore, higher maintenance doses of these cofactors are indicated, particularly during infections and other stress periods in clinical practice and RCTs.
A balanced diet high in colored vegetables will improve this situation. For example, consuming an average banana will provide between 150 to 200 mg of magnesium but adds calories. However, for the reasons above, many require additional supplemental vitamin D (A, C, B2, and K2) and magnesium, zinc, boron, and other cofactors for fully functioning enzymes and immune systems. Micronutrients can be supplemented economically via multivitamins or micronutrient capsules. Explaining the different cofactors that can be obtained from which food items is beyond the scope of this discussion.
Are there any nutrients you suggest individuals avoid when taking high-dose vitamin D, such as calcium?
One of the primary (canonical) functions of vitamin D [calcitriol; 1,25(OH)2D] is to increase intestinal calcium absorption. The most active metabolite of vitamin D, calcitriol, increases circulatory calcium concentrations. This occurs via enhancing intestinal absorption of calcium, renal tubular calcium reabsorption, and calcium release from mineralized bone. While this process is tightly regulated, excess calcium or vitamin D intake can override homeostasis, calcifying soft tissue.
There is an intrinsic protective mechanism: when dietary or supplemental calcium intake and biologically available calcitriol increases, the fractional (~percentage) intestinal absorption of calcium decreases—the higher the calcium and vitamin D, the lower the calcium absorption (similar, but not identical, to a threshold mechanism we discussed previously). This is an intrinsic safety mechanism to minimize excess calcium absorption from the intestine into the blood. There are hardly any drug interactions with vitamin D.
However, excess calcium (or vitamin D) intake, especially in the presence of vitamin D sufficiency, could override the safety mechanism. Therefore, when the vitamin D intake is increased, as we discussed above, reducing the (total) calcium ingestion is necessary. With pharmacological doses of vitamin D, as in the Coimbra protocol, it is essential to stop all supplemental calcium (including calcium containing multivitamins tablets), and consumption of a low calcium diet is recommended. There are no other interactions that need to be of concern.
I hope our discussion will be helpful to readers in keeping healthy at a minimal or no cost. Thank you for having me in this important questions and answers session.
Thank you, Dr. Wimalawansa, for sharing your time and wisdom with us here at GrassrootsHealth and the community worldwide!
* The above is a scientific discussion and should not be considered medical advice. Regarding clinical or personal issues, Prof. Wimalawansa advises readers to consult her/his physician.
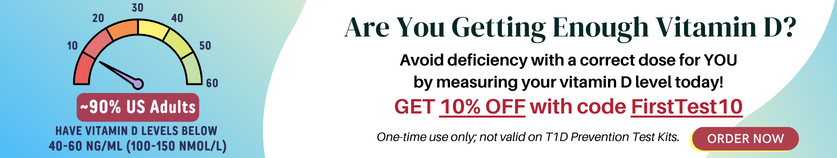
Test to See if You Are Getting Enough Vitamin D and Other Important Nutrients
 Create your custom home test kit to measure your levels at home as part of the D*action project!
Create your custom home test kit to measure your levels at home as part of the D*action project!
With your kit you can measure your:
- Vitamin D
- Magnesium PLUS Essential and Toxic Elements
- Omega-3 Fatty Acids
- hsCRP
- HbA1c
- TSH
- Type 1 Diabetes Autoantibodies
Did you know that each of the above can be measured at home using a simple blood spot test? As part of our ongoing research project, you can order your home blood spot test kit to get your levels, followed by education and steps to take to help you reach your optimal target levels. Start by enrolling and ordering your kit to measure each of the above important markers, and make sure you are getting enough of each to support better mood and wellbeing!
Create your custom home test kit today. Take steps to improve the status of each of these measurements to benefit your overall health. With measurement you can then determine how much is needed and steps to achieve your goals. You can also track your own intakes, symptoms and results to see what works best for YOU.