Published on June 8, 2020
Our vitamin D myth busting series continues, with our last post dispelling the myth that vitamin D can be stored in our fat cells for later use and can become toxic. While it is true that vitamin D has a higher affinity for fat, there is a relatively constant ratio of vitamin D in fat to blood, and the body does not rely on vitamin D in fat to increase vitamin D blood levels, nor is build-up of vitamin D in fat tissues a concern for toxicity.
However, there is always concern about toxicity when taking in anything in excessive doses. Even drinking too much water can throw our system out of whack and become toxic, even fatal – a condition known as water intoxication or hyponatremia.
When should you be concerned about vitamin D toxicity?
 Vitamin D toxicity is rare and usually caused by excessive vitamin D supplementation, which can lead to hypercalcemia (increased calcium in the blood), hyperphosphatemia (increased phosphate in the blood), and suppressed serum PTH concentrations. Symptoms include vomiting, nausea, abdominal pain, fatigue, and weakness. Most cases of vitamin D toxicity have been related to supplement manufacturing and labeling errors, as well as overdosing (seen in some cases with intakes of 50,000 IU/day or more over an extended period of time such as six months or longer), or over-correction of vitamin D deficiency (seen with intakes of about 77,000 IU/day for two months).
Vitamin D toxicity is rare and usually caused by excessive vitamin D supplementation, which can lead to hypercalcemia (increased calcium in the blood), hyperphosphatemia (increased phosphate in the blood), and suppressed serum PTH concentrations. Symptoms include vomiting, nausea, abdominal pain, fatigue, and weakness. Most cases of vitamin D toxicity have been related to supplement manufacturing and labeling errors, as well as overdosing (seen in some cases with intakes of 50,000 IU/day or more over an extended period of time such as six months or longer), or over-correction of vitamin D deficiency (seen with intakes of about 77,000 IU/day for two months).
Currently, the U.S. National Academy of Medicine (NAM, formerly the Institute of Medicine) has set their recommended daily allowance of vitamin D at 600 IU/day, their upper intake level at 4,000 IU/day, and their no adverse effects level (NOAEL) at 10,000 IU/day. However, the vast majority of the population will not reach a vitamin D level of 40-60 ng/ml (100-150 nmol/L), the range recommended by the GrassrootsHealth panel of 48 vitamin D researchers and scientists, if taking only the daily recommended amount of 600 IU/day. Looking at a starting serum level of 20 ng/ml (close to the population average), an intake of at least 3,300 IU/day would be sufficient for only 50% of adults to achieve a level of 40 ng/ml or greater. Some will require more; at least 4,700 IU/day would be sufficient for 90% of adults to achieve 40 ng/ml or greater. These intake levels may seem high compared to the recommendations made by the NAM, leading to concern from individuals who are not aware of the wealth of vitamin D research demonstrating its safety.
How much vitamin D can cause toxicity?
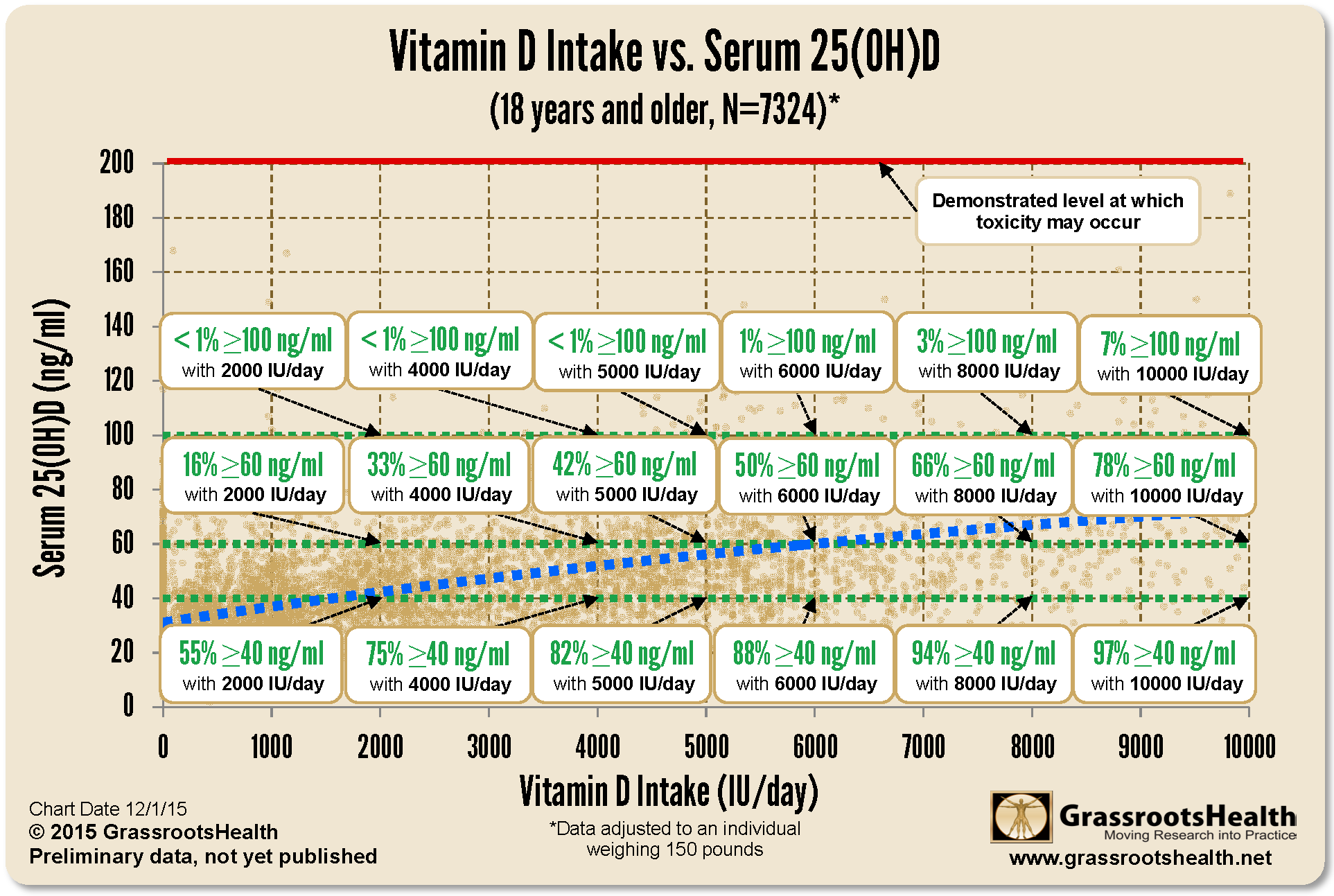
The chart below shows a plot of the vitamin D serum levels as a function of reported vitamin D intake amounts from the GrassrootsHealth cohort, adjusted to an individual weighing 150 pounds. The dotted blue line is the best fit line through the data.
Shown on the figure are the percent of participants who are at or above 40, 60, and 100 ng/ml for various vitamin D supplement intake amounts. Fewer than 1% of participants have vitamin D levels ≥100 ng/ml resulting from an intake of 6000 IU/day or less, and no participants reached a level above 200 ng/ml, the demonstrated level at which toxicity may occur (Hathcock et al.), as illustrated by the red line at the top of the chart. Hathcock et al. also observed no toxicity in studies reporting a daily vitamin D intake below 30,000 IU/day.
A study published by McCullough et al. describes the results of routine vitamin D testing and supplementation among all patients admitted to a state psychiatric hospital in Cincinnati, Ohio. Patients received vitamin D supplementation at either 5000 IU/day (group 1) or 10,000 IU/day (group 2), for 12 months or longer. Average baseline vitamin D levels among patients were 24-25 ng/ml. Doses ranging from 20,000 to 60,000 IU/day were used in individual cases for patients with psoriasis, asthma, and skin cancer. Serum calcium and parathyroid hormone (PTH) levels were also measured and tracked to identify potential cases of vitamin D toxicity. There were no adverse events related to vitamin D supplementation and no cases of vitamin D induced hypercalcemia were observed in any patients.
It is important to remember that a single dose of mid-day sunshine, known as an “erythema dose,” can produce roughly 10,000 to 25,000 IU of vitamin D. A minimal erythema dose is defined by a pinkness of the skin about 1-6 hours after sun exposure, going away within 24 hours. There is no single erythema dose or sun exposure time recommendation, due in part to varying sun intensity as well as differences in skin type and other individual differences in vitamin D production.
What else to consider?
Individuals with certain conditions, such as primary hyperparathyroidism, sarcoidosis, tuberculosis, and lymphoma, may be hypersensitive to vitamin D supplementation and may need to be more cautious when supplementing, or work with a health care provider.
Another concern, which we will address soon, is that taking too much vitamin D without co-nutrients may create imbalances – this is what makes adequate intake of co-nutrients, either from diet or supplements, so very important. Stay tuned!
Is it true?
Our goal with this “Vitamin D Myths” series is to provide information and resources to answer the question, “Why should I care about vitamin D?” and to help dispel the myths and misconceptions surrounding it that may be preventing you and others from accepting it as an essential component to health. We will also discuss other nutrients essential to the function of vitamin D (and vice versa) within the body that should not be ignored.
Vitamin D is necessary for multiple functions within the body and should not be ignored, but has the hype about vitamin D and its role in the body’s response to COVID-19 been over-exaggerated? What concerns about vitamin D are valid, and which are not? We want to provide you with evidence based information to help you decide what vitamin D action to take, if any, for your own health.
We want to hear from you!
Is there a particular ‘myth’ you have heard about vitamin D? Or, something you have read or been told that makes you question whether vitamin D ‘deserves’ so much attention? Or whether you should be taking it and how much? Share with us by emailing jen @grassrootshealth.org what you have heard that makes you question vitamin D so that we can consider addressing it in our newsletters.
Know if you are getting enough vitamin D and other important nutrients
Vitamin D, along with magnesium, zinc, and omega-3s, are just a few nutrients vital to maintaining our health. To know if you are getting enough of these nutrients, make sure you test today!
Are You Getting Enough Vitamin D to Help Yourself?
Do you know what your vitamin D level is? Be sure to test today to find out, and take steps to keep it within a target of 40-60 ng/ml or 100-150 nmol/L! Give your immune system the nutrients it needs to support a healthy you and protect yourself from unnecessary diseases.
Through GrassrootsHealth Nutrient Research Institute, you can also test your essential elements magnesium, copper, zinc and selenium, toxins such as lead, mercury and cadmium, as well as your omega-3 levels, inflammation levels and thyroid stimulating hormone (TSH) level. Find out your levels today! Log on to the test selection page (click the link below) to get your tests and see for yourself if your levels can be improved.
Make sure you track your results before and after, about every 6 months!
How can I track my nutrient intake and levels over time?
To help you track your supplement use and nutrient levels, GrassrootsHealth has created the Personal Health Nutrient Decision System called
For each specific supplement, you can track what days you take it, how much, and many other details. This will help you know your true supplemental intake and what patterns of use work for you to reach and maintain optimum nutrient levels. Check it out today!