Published on February 3, 2023
An explanation of how taking both vitamin D and omega-3s together works to help prevent autoimmune disorders and immune-mediated conditions
Key Points
- Vitamin D has demonstrated anti-infective, anti-inflammatory, and immunomodulatory properties; it acts to suppress the production of inflammatory cytokines (such as IL-1, IL-6 and IFN which are predominant in the cytokine storm characteristic of severe COVID-19), and plays a very important role in preventing the activation of an inappropriate hyper-inflammatory immune response, therefore preventing cytokine storm
- Omega-6s (such as AA) are pro-inflammatory, essential for initiating and sustaining the inflammatory response – a physiologic function necessary for healing from injuries and infection, while omega-3s (such as DHA and EPA) are anti-inflammatory and promote the resolution of the inflammatory process; AA plays an important role in the initiation of acute inflammation, which then becomes moderated by the involvement of omega-3s (EPA and DHA) as they replace AA and begin to resolve inflammation
- New research is showing a potential effect of omega-3s on vitamin D levels and metabolism, leading to an overall increase in 25(OH)D levels following omega-3 supplementation of 8 weeks or longer, and a role of omega-3s in increasing 1,25(OH)2D levels
- Measuring vitamin D levels along with the AA:EPA Ratio and HbH1c (a marker of blood sugar health) can help individuals take more specific steps towards achieving lower overall inflammation levels

One of the most impressive findings published from the VITAL trial may have been the effect of vitamin D and omega-3s on reducing the incidence of autoimmune disease.
To follow up on these findings, Infante et al. review the mechanisms and properties of vitamin D and omega-3 co-supplementation, and how the two molecules work together to decrease inflammation and modulate the immune response, in their publication The importance of vitamin D and omega-3 PUFA supplementation: a nonpharmacologic immunomodulation strategy to halt autoimmunity.
How Vitamin D and the Omegas Influence the Immune System and Inflammation
Vitamin D has demonstrated anti-infective, anti-inflammatory, and immunomodulatory properties. It acts to suppress the production of inflammatory cytokines (such as IL-1, IL-6 and IFN which are predominant in the cytokine storm characteristic of severe COVID-19), and plays a very important role in preventing the activation of an inappropriate hyper-inflammatory immune response, therefore preventing the now infamous cytokine storm. Not only does vitamin D work directly on the cells of the immune system, many of these cells also produce their own vitamin D by expressing vitamin D converting enzymes to manufacture site-specific 25(OH)D and 1,25D. The authors suggest evidence pointing to a minimum 25(OH)D level of 40 ng/ml (100 nmol/L) to fully optimize these demonstrated anti-inflammatory and immune regulating properties of vitamin D.
Omega-3 and omega-6 fatty acids are poly-unsaturated fatty acids (PUFAs) that work together to directly regulate inflammation, immune function, and pain. Eicosapentaenoic acid (EPA) and eocosahexaenoic acid (DHA) are the two main omega-3 fatty acids, while the most common omega-6 fatty acid is linoleic acid (LA), which is converted into longer omega-6 fats such as arachidonic acid (AA). Omega-6s (such as AA) are pro-inflammatory, essential for initiating and sustaining the inflammatory response – a physiologic function necessary for healing from injuries and infection. Omega-3s (such as DHA and EPA) are anti-inflammatory and promote the resolution of the inflammatory process. More specifically, AA plays an important role in the initiation of acute inflammation, which then becomes moderated by the involvement of omega-3s (EPA and DHA) as they replace AA, as well as vitamin D, and begin to resolve inflammation. It is for this reason that the AA:EPA ratio can be used as a biomarker of systemic inflammation, with a smaller ratio being indicative of lower levels of inflammation compared to a higher ratio. Infante et al. suggest an AA:EPA ratio of between 1.5 and 3 to represent optimal inflammation levels.
The Results of Vitamin D and Omega-3 Co-Supplementation
Many studies have identified a link between decreased levels of inflammation and higher levels of either vitamin D and/or omega-3s, with potentially synergistic anti-inflammatory and immunomodulating effects when taken together (meaning the sum of the effect is greater than either alone).
Research has demonstrated that co-supplementation with both vitamin D and omega-3s has the potential to significantly affect
- insulin resistance
- non-alcoholic fatty liver disease
- prediabetes
- type 2 diabetes associated with coronary heart disease
- gestational diabetes
- polycystic ovary syndrome (PCOS)
- type 1 diabetes
- inflammatory bowel disease
- autism spectrum disorder
How Omega-3s and Vitamin D Influence Each Other
New research is showing a potential effect of omega-3s on vitamin D levels and metabolism. A recent review and meta-analysis by Alhabeeb et al. revealed an overall increase in 25(OH)D levels following omega-3 supplementation of 8 weeks or longer, with a significant effect seen when baseline vitamin D levels were below 20 ng/ml (50 nmol/L). Evidence also suggests omega-3s can directly modulate vitamin D metabolism and activation by acting on the enzymes that regulate vitamin D, leading to an increase in 1,25(OH)2D and a higher ratio of 1,25(OH)2D to 25(OH)D.
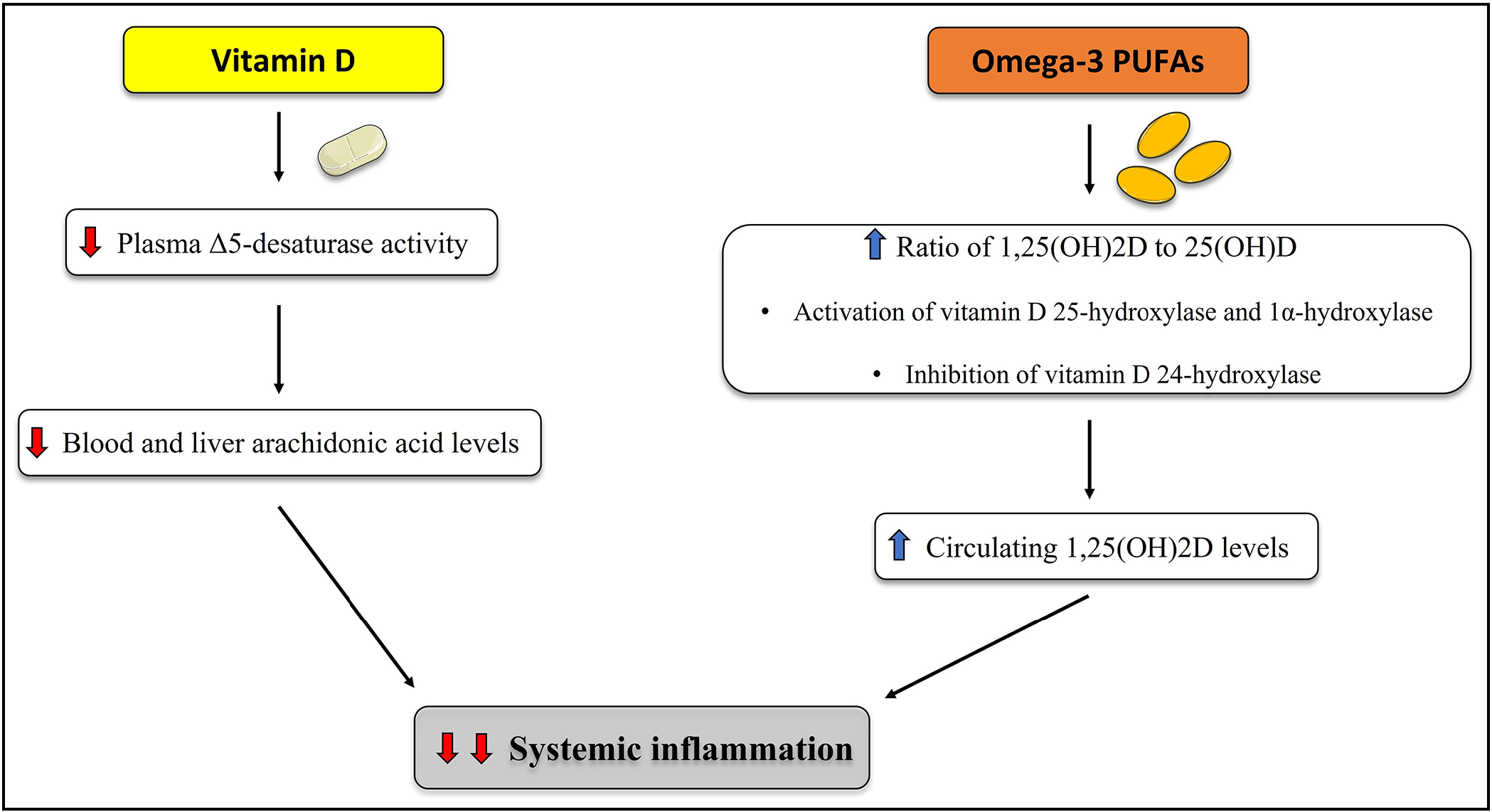
The following diagram illustrates how vitamin D and omega-3s influence one another, leading to enhanced anti-inflammatory and immunomodulatory effects.
While the findings from the VITAL trial demonstrated that vitamin D and omega-3 supplementation help prevent autoimmune disease, Infante et al. add the following:
“With regard to the VITAL study, it is also plausible that higher vitamin D and omega-3 PUFA doses (aimed to achieve optimal circulating 25-hydroxyvitamin D and AA/EPA ratio values) may have led to even better results.”
Measuring these Levels Can Help Determine Your Amount of Inflammation and Disease Risk
The AA:EPA Ratio measures the ratio of the amount of pro-inflammatory AA and anti-inflammatory EPA in the red blood cells, and can be an indication of the amount of cellular inflammation in the body. The above authors recommend an AA:EPA Ratio of 1.5 to 3 for the resolution of cellular inflammation.
Measuring vitamin D levels along with the AA:EPA Ratio and HbH1c (a marker of blood sugar health) can help individuals take more specific steps towards achieving lower overall inflammation levels, mainly by increasing vitamin D intake if necessary, and/or increasing omega-3 (EPA and DHA) intake while decreasing pro-inflammatory omega-6 intake (such as AA) and making dietary changes as indicated by the test results.
HbA1c is a measure of blood sugar health; higher levels can indicate blood sugar imbalance, pre-diabetes or metabolic disorder, which is often a combination of increasing insulin resistance and inflammation. Considering this result can give additional clues as to how diet may be affecting your levels of inflammation.
The Inflammation Panel test kit offered by GrassrootsHealth includes the above measurements along with hsCRP, a direct indicator of chronic inflammation in the body.
How Much Vitamin D and Omega-3s Do You Need? Find Out with Your Home Test Kit!
 Having and maintaining healthy vitamin D levels and other nutrient levels can help improve your health now and for your future. Choose which additional nutrients to measure, such as your omega-3s and essential minerals including magnesium and zinc, by creating your custom home test kit today. Take steps to improve the status of each of these measurements to benefit your overall health. With measurement you can then determine how much is needed and steps to achieve your goals. You can also track your own intakes, symptoms and results to see what works best for YOU.
Having and maintaining healthy vitamin D levels and other nutrient levels can help improve your health now and for your future. Choose which additional nutrients to measure, such as your omega-3s and essential minerals including magnesium and zinc, by creating your custom home test kit today. Take steps to improve the status of each of these measurements to benefit your overall health. With measurement you can then determine how much is needed and steps to achieve your goals. You can also track your own intakes, symptoms and results to see what works best for YOU.
Enroll in D*action and Test Your Levels Today!





