Published on May 22, 2025
Several studies conclude that regular, sensible, non-burning sun exposure throughout the lifetime, and higher vitamin D levels, are healthy for the skin and related to decreased incidence of melanoma and increased melanoma survival rates
Key Points
- Two important distinctions about the relationship between sunshine exposure and skin cancer should be made: 1) intermittent, or sudden, drastic exposure to high intensity sunlight (resulting in sunburn) does increase the risk of skin cancer, and 2) regular, moderate, non-burning exposure to sunshine (sensible sunshine exposure) has been associated with lower risk of skin cancer
- Moderate, non-burning sunshine exposure initiates specific repair mechanisms within skin cells, including DNA repair enzymes and the production of local vitamin D, which work to prevent damage accumulation; vitamin D synthesized in the skin has several anti-cancer properties, including roles in cell differentiation, cell death, cell adhesion, and oxidative stress, all of which can help protect against the development of cancer
- Several studies are reviewed to demonstrate how increased, sensible sunshine exposure and increased vitamin D levels are related to decreased melanoma incidence and mortality, decreased tumor size, and improved response to melanoma treatment

The sun has gotten a bad reputation because of the association between ultraviolet (UV) exposure and skin cancers. However, two important distinctions should be made: 1) intermittent, or sudden, drastic exposure to high intensity sunlight (resulting in sunburn) does increase the risk of skin cancer, and 2) regular, moderate, non-burning exposure to sunshine (sensible sunshine exposure) has been associated with lower risk of skin cancer.
The three primary types of skin cancer to distinguish between are basal cell carcinoma (BCC), squamous cell carcinoma (SCC), and melanoma. According to the American Cancer Society, a vast majority of skin cancers are non-melanoma skin cancers, with BCC accounting for approximately 80% of cases and SCC ~20%. These non-melanoma skin cancers usually grow slowly, rarely spread to other parts of the body, and are very treatable.
Melanoma itself accounts for approximately 1-7% of all skin cancers (depending on the country) and is more dangerous than other skin cancers because it is more likely to spread to other parts of the body if not caught early. The sun has been to blame for an increased risk of melanoma, however, studies are now clearly showing that the incidence of melanoma and the risk of death due to melanoma are decreased with increased, regular, non-burning sun exposure and higher vitamin D levels.
Watch the Videos
 Does sensible sun exposure cause melanoma?
Does sensible sun exposure cause melanoma?
Is there any evidence that regular, moderate, “sensible” sun exposure causes melanoma? Listen in to this snippet of an interview with Dr. Michael Holick as he explains. Watch Now
 What is Sensible Sun Exposure?
What is Sensible Sun Exposure?
“Sensible” sunshine exposure has many benefits for health and can reduce the risks associated with sunburn and over-exposure. But, what is “sensible” sun exposure? Dr. Michael Holick, Ph.D, MD explains. Watch Now
 Can sensible sunshine exposure help repair UV damage from the sun?
Can sensible sunshine exposure help repair UV damage from the sun?
When used sensibly and safely (as in, Don’t Burn!), sunlight induces several processes to repair the DNA damage caused by UV rays. Learn more in this interview snippet with Dr. Michael Holick.
How Does Skin Cancer Develop… or Not?
Exposure to UV radiation from the sun induces DNA damage within skin cells. Moderate, non-burning sunshine exposure also initiates specific repair mechanisms within these same skin cells, including DNA repair enzymes and the production of local vitamin D, which work to prevent damage accumulation. Vitamin D synthesized in the skin has several anti-cancer properties, including roles in cell differentiation, cell death, cell adhesion, and oxidative stress, all of which can help protect against the development of cancer. It is for these reasons that moderate, regular, non-burning exposure to sunshine (sensible sunshine exposure) can decrease the risk of skin cancer.
Unfortunately, some of the negative effects of chronic, prolonged UV radiation (the kind that leads to acute sunburn) includes sustained accumulation of damage to the skin cell DNA, inflammation, and photo-aging, which can lead to the initiation and development of skin cancer. More specifically, according to Rosso et al., painful sunburns before the age of 20 seem to be a strong predictor of all types of skin cancer, while chronic or lifetime sun exposure has been associated with an increased risk of SCC but a decreased risk of BCC and melanoma.
UVB Exposure on the Skin Generates Protective Molecules that Help Fight & Prevent Skin Cancer
Hot Off the Press! New 2025 Featured Paper: Illuminating the Connection: Cutaneous Vitamin D3 Synthesis and Its Role in Skin Cancer Prevention
Non-melanoma skin cancers, including basal cell carcinoma and squamous cell carcinoma, are strongly linked to chronic sun exposure, particularly in frequently exposed areas like the face and hands. Meanwhile, melanoma has a more nuanced relationship with sun exposure. While intense, intermittent UV exposure and childhood sunburns significantly increase melanoma risk, chronic occupational sun exposure appears to be protective in some studies, as explained in more detail below.
Vitamin D3 synthesized in the skin via UVB radiation plays a protective role in the skin by reducing inflammation, supporting DNA repair, and decreasing oxidative stress. The active form of vitamin D3, 1,25-dihydroxyvitamin D3, along with other photoproducts like lumisterol derivatives, demonstrates anti-proliferative and immune-modulating effects that may inhibit the initiation and progression of skin cancers. Studies in animal models have shown these compounds to significantly reduce the development of UV-induced skin tumors, suggesting that vitamin D3 and its metabolites counteract some of the harmful effects of UV exposure.
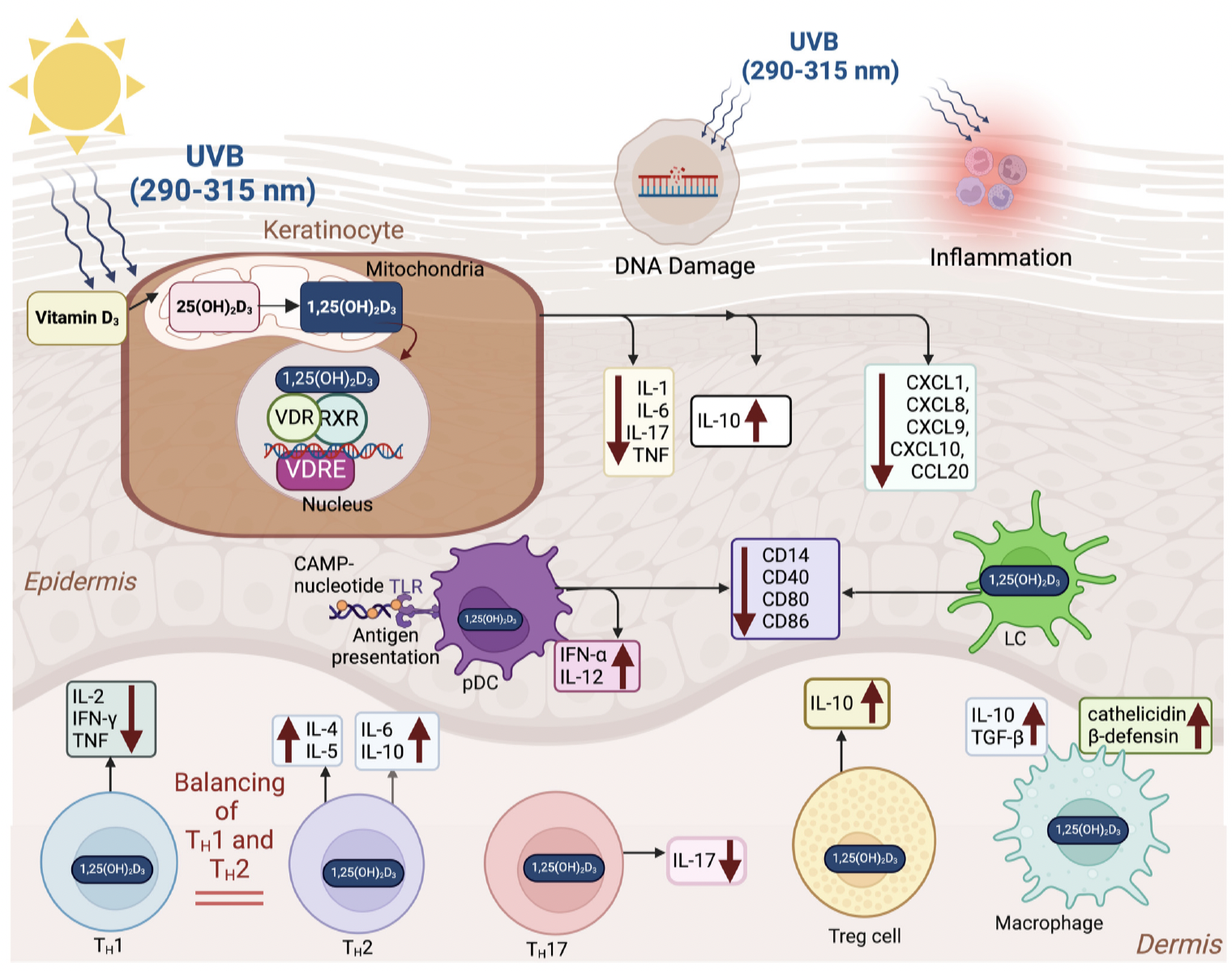
The diagram above illustrates how UVB exposure leads to vitamin D3 production in the skin, which is then converted to its active form, 1,25(OH)₂D₃, within keratinocytes. This active form binds to the vitamin D receptor (VDR) and modulates immune responses by reducing pro-inflammatory cytokines and enhancing anti-inflammatory and antimicrobial activity. It also shifts immune cell behavior toward a more regulated, anti-inflammatory state, supporting skin protection and homeostasis.
Remember, excessive exposure increases skin cancer risk – and balance is always key. Therefore, brief, controlled exposure to sunlight, particularly on larger body surfaces such as the torso and limbs, is recommended, while the face should be protected due to its high risk of chronic UV damage and minimal contribution to vitamin D3 production. For individuals at high risk for skin cancer or those living in areas with limited sun exposure, dietary sources such as oily fish, fortified foods, and supplements offer effective alternatives for maintaining vitamin D status.
As a reminder, vitamin D cannot be produced from morning sunlight. The paper cautions against over-exposure to early morning or late afternoon sun, which contains mostly UVA radiation that contributes to DNA damage without supporting vitamin D3 production. Midday sun, though more intense, is necessary for effective vitamin D synthesis and, if exposure is limited and controlled, can be a safe and beneficial health practice.
Lower Melanoma Risk with Regular, Sensible Sunshine Exposure
Several studies have confirmed an inverse relationship between increased occupational or regular, sensible sunshine exposure and the risk of melanoma. A meta-analysis of 57 studies on sun exposure and melanoma risk by Gandini et al. found a positive association between intermittent, high intensity sun exposure and increased risk for melanoma, and an inverse association between high occupational sun exposure and risk for melanoma. This means that as occupational sun exposure increased, the risk of melanoma decreased. As stated by the authors, “Intermittent sun exposure and sunburn history were shown to play considerable roles as risk factors for melanoma, whereas a high occupational sun exposure seemed to be inversely associated to melanoma.”
In 2012, the World Health Organization’s (WHO) International Agency for Research on Cancer (IARC) published a detailed analysis of studies on sun exposure and melanoma and found that continuous, regular sun exposure was not associated with melanoma, but rather, sunburn doubled the risk of developing melanoma and intermittent, high-intensity sun exposure proposed a 61% increased risk for melanoma.
Other publications have even suggested that the prevalence of melanoma caused by UV exposure has been grossly overestimated. A 2022 cross-sectional study by Mata et al. of 343,589 patients with solid tumors looked at UV mutational signatures as a biomarker for identifying cancers caused by genomic alterations due to UV exposure. They found that UV exposure accounts for 9 times less melanoma than what has previously been reported (11% vs 95%).
Lower Vitamin D Levels Associated with Increased Melanoma Incidence, Mortality, and Tumor Thickness
Many studies have shown that higher vitamin D levels are protective of many cancers; this includes melanoma. A 2022 study by Kanasuo et al. looked at data from 498 adults who were at risk for skin cancer for an association between skin cancer incidence and vitamin D supplement use. Those who regularly took vitamin D supplements had significantly less skin cancers of any type compared to those who did not take vitamin D supplements, although further analysis showed this effect to be more associated with melanoma and SCC, while cases of BCC were evenly distributed among all groups. In fact, the study found a 55% decreased risk of past or present melanoma among those who regularly took vitamin D supplements compared to those who did not. Overall, this study indicated a protective effect of vitamin D on melanoma and SCC.
A 2023 study by Shellenberger et al. had similar findings; the authors found that having vitamin D levels below 20 ng/ml (50 nmol/L) was significantly related to an increased risk of melanoma, demonstrating a protective effect of vitamin D and/or ultraviolet exposure against the development of melanoma.
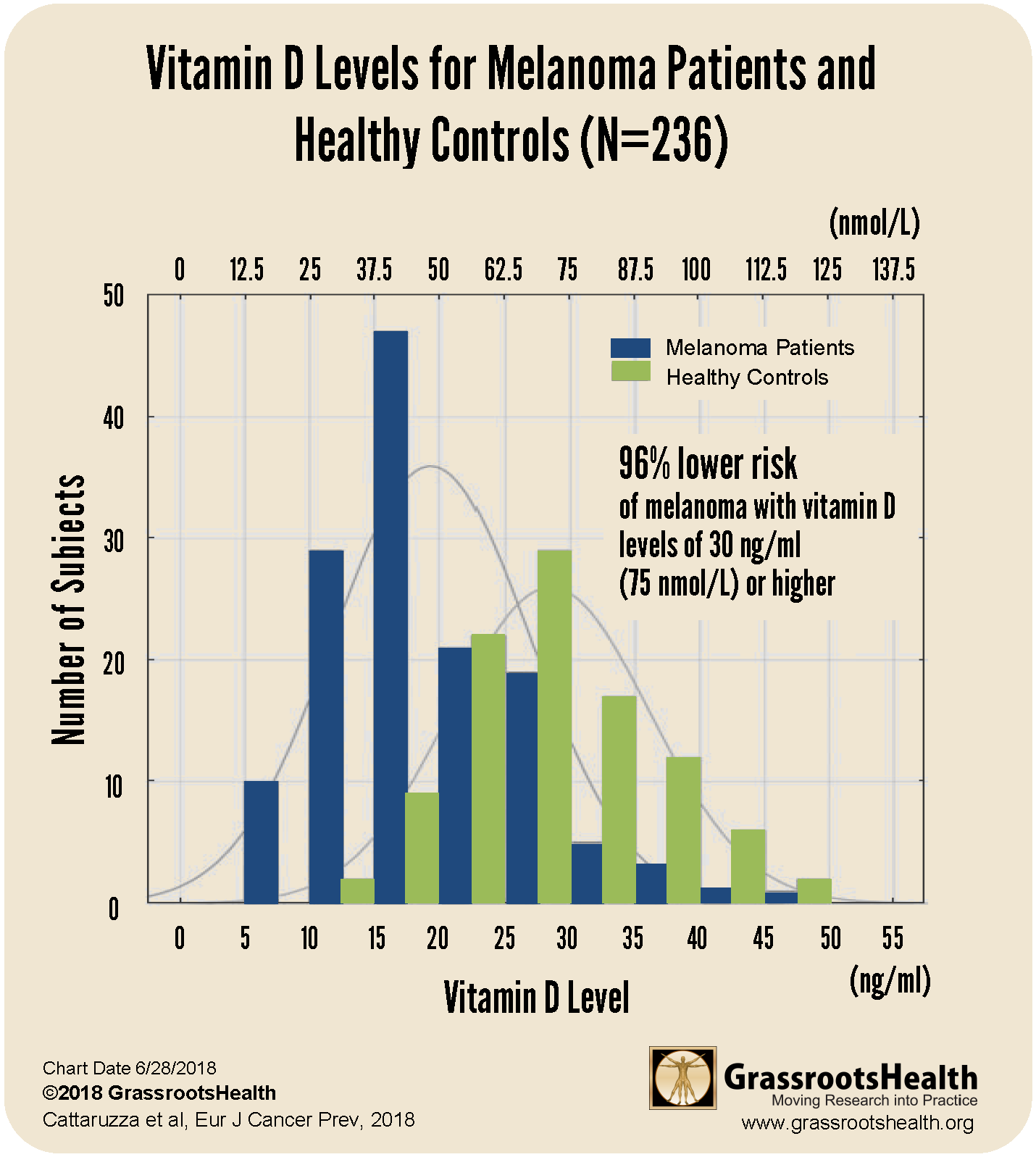
Results from a 2018 case-control study by Cattaruzza et al. showed a clear decrease in melanoma risk as vitamin D levels increased, as illustrated in the chart below.
This study included 137 melanoma patients and 99 healthy controls. The research team found that the average vitamin D level of melanoma patients was lower than the average level of the healthy controls by 10 ng/ml (25 nmol/L) and that the majority of melanoma patients had vitamin D levels at or below 20 ng/ml (50 nmol/L) compared to just 15% of the healthy controls. Furthermore, participants with vitamin D levels at or above 30 ng/ml (75 nmol/L) had a 96% lower risk of melanoma compared to participants with levels at or below 20 ng/ml (50 nmol/L) after adjusting for age, sex and BMI.
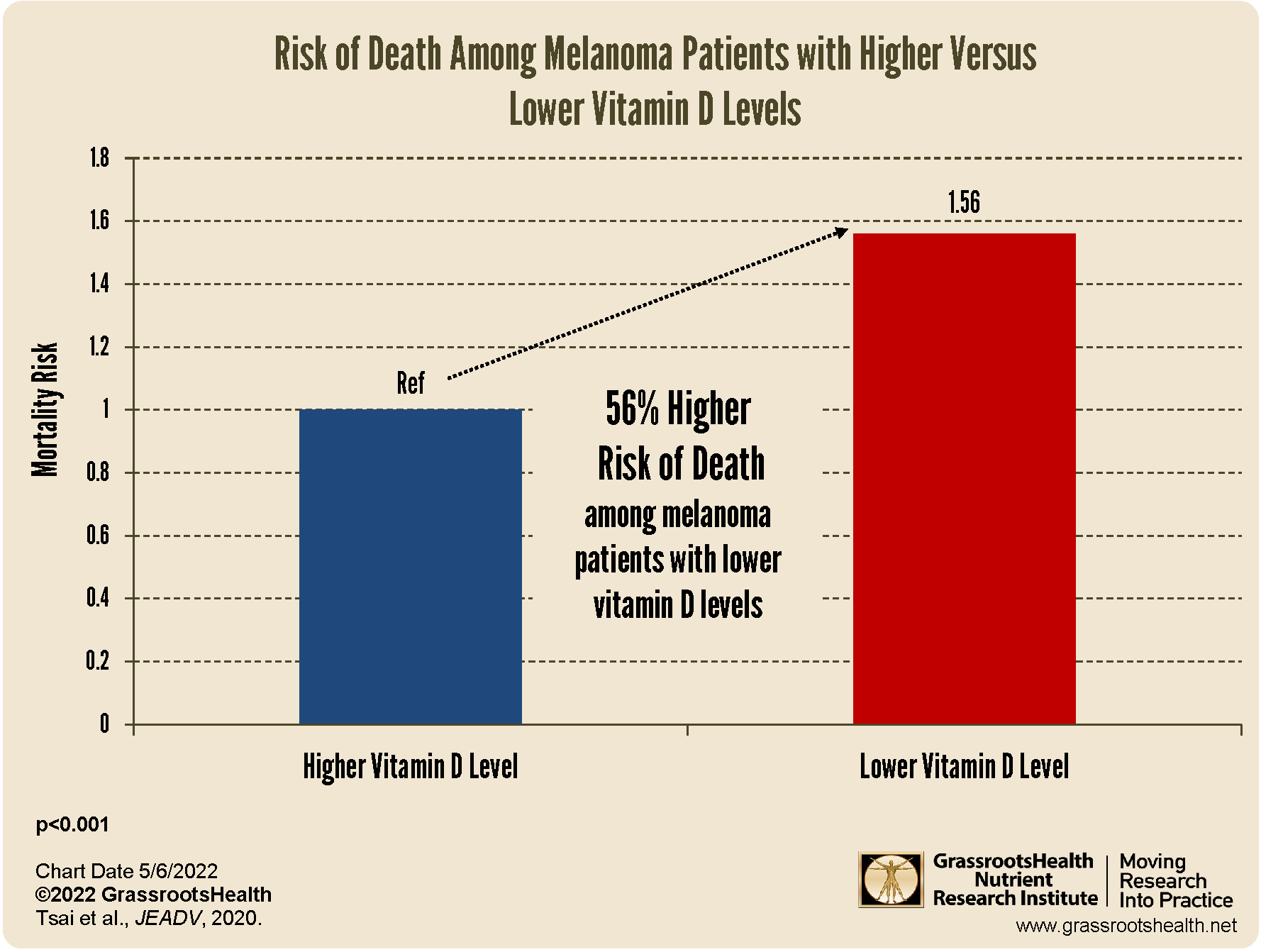
A meta-analysis by Tsai, Kuo et al. 2020 found that melanoma patients with lower vitamin D levels had a 56% higher mortality rate compared to those with higher vitamin D levels, as shown in the chart below.
The authors looked at 25 studies, with a total of 11,166 melanoma patients, and found that vitamin D deficiency was more prevalent among melanoma patients compared to controls (P<0.001), and melanoma patients had a significantly higher mortality rate if they had lower vitamin D levels compared to higher vitamin D levels (P<0.001). They also found that tumor thickness was significantly related to vitamin D level, with a thickness of 1 millimeter (mm) or less related to a higher vitamin D level and a tumor thickness of greater than 1 mm much more likely with lower vitamin D levels (P<0.001).
Vitamin D levels have even been associated with improved success of melanoma treatments. A study by Galus et al. followed 200 patients with advanced melanoma who were receiving immunotherapy treatment for their cancer to see if vitamin D levels and supplementation affected disease progression. They found that those with vitamin D levels above 30 ng/ml (75 nmol/L), either at baseline or achieved with supplementation, had a much better response rate to treatment (56% vs 35%) along with increased progression-free survival times (11.25 months vs 7.9 months) compared to those with vitamin D levels below 30 ng/ml who did not supplement.
Make Sure You Are Getting Enough of Both Sunshine & Vitamin D
It is important to incorporate safe, sensible sun exposure into a regular routine, just as it is important to make sure you are getting enough vitamin D. Because the sun produces many health-benefiting molecules in addition to vitamin D, sunshine exposure cannot be replaced with taking a supplement.
It is also important not to stop supplementing with vitamin D during the summer. Most people do not make enough vitamin D from sunshine alone, due to their lifestyle and other factors, and therefore must rely on supplementation to maintain optimal vitamin D levels of 40-60 ng/ml (100-150 nmol/L).
This Sunshine Month, get 10% off your home blood spot test kits PLUS the free Sunshine eBook when using the code SUNMONTH25 at checkout. Or, save on 2 Vitamin D test kits (for before and after summer sun) plus the Sunshine eBook with our Sunshine Month Bundle here!
Measure Your Vitamin D Level Today
 Having and maintaining healthy vitamin D levels and other nutrient levels can help improve your health now and for your future. Choose which additional nutrients to measure, such as your omega-3s and essential minerals including magnesium and zinc, by creating your custom home test kit today. Take steps to improve the status of each of these measurements to benefit your overall health. With measurement you can then determine how much is needed and steps to achieve your goals. You can also track your own intakes, symptoms and results to see what works best for YOU.
Having and maintaining healthy vitamin D levels and other nutrient levels can help improve your health now and for your future. Choose which additional nutrients to measure, such as your omega-3s and essential minerals including magnesium and zinc, by creating your custom home test kit today. Take steps to improve the status of each of these measurements to benefit your overall health. With measurement you can then determine how much is needed and steps to achieve your goals. You can also track your own intakes, symptoms and results to see what works best for YOU.
Enroll in D*action and Test Your Levels Today!


 Does sensible sun exposure cause melanoma?
Does sensible sun exposure cause melanoma? What is Sensible Sun Exposure?
What is Sensible Sun Exposure? Can sensible sunshine exposure help repair UV damage from the sun?
Can sensible sunshine exposure help repair UV damage from the sun?