Published on May 22, 2023
Numerous studies have now confirmed a decreased risk of many different types of cancer with increased lifetime sunshine and UVB exposure
Key Points
- Studies describing the relationship between UVB exposure, sunlight, and vitamin D on the incidence of colon, breast, ovarian, and other cancers have been published by the Garland brothers and other authors, with a recurring theme of decreased cancer risk with increased UVB and vitamin D
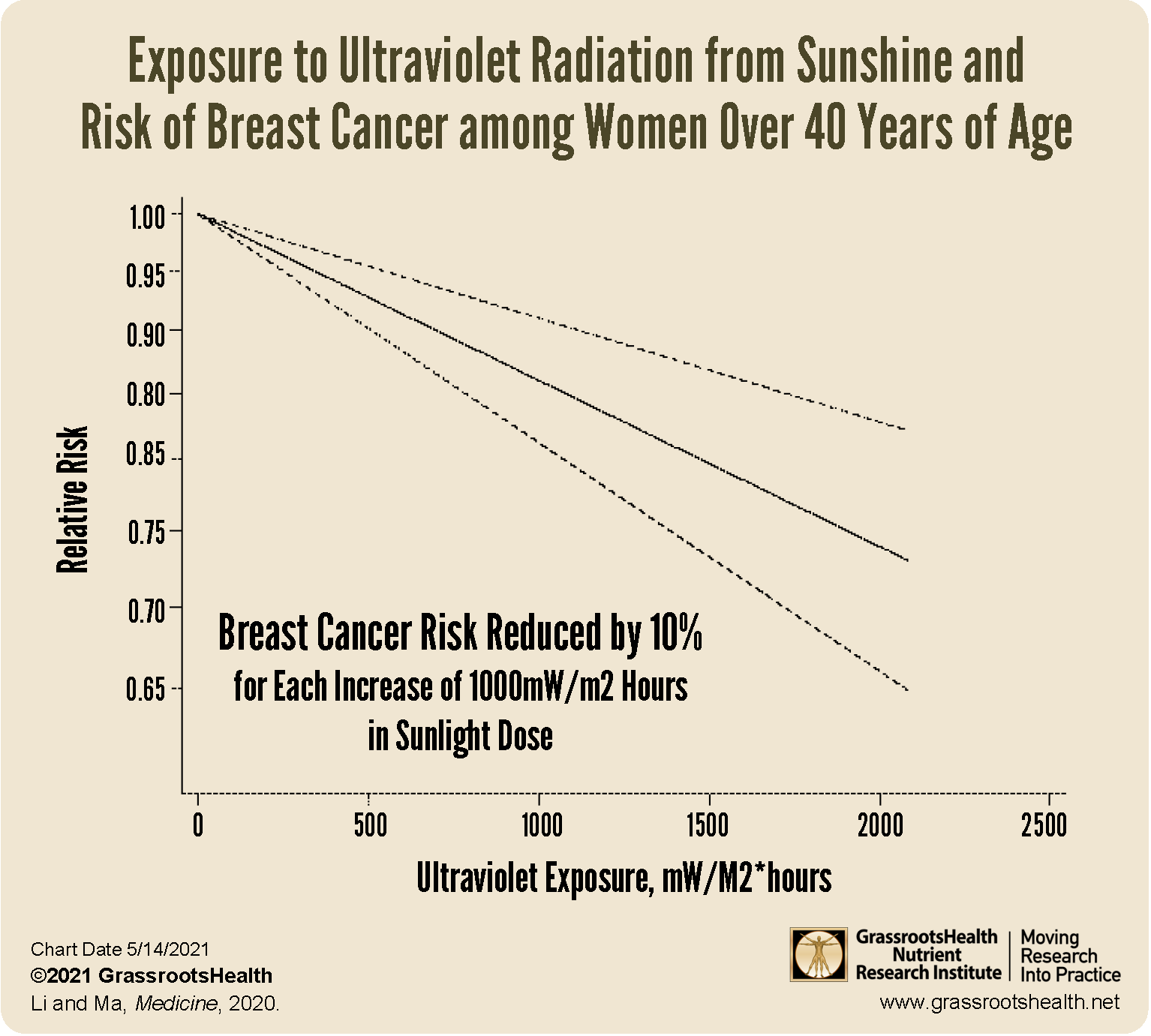
- A significant dose-response correlation between UV exposure and breast cancer risk was found in one study, such that women in the highest exposure groups had a 30% lower risk of breast cancer compared to women in the lowest exposure groups; overall, this study saw a negative correlation between UV exposure and breast cancer risk, especially among women over 40 years of age, and women who did not tan or who covered their arms and legs while in the sun also had a higher risk of breast cancer
- A detailed analysis of studies on sun exposure and melanoma and found that continuous, regular sun exposure was not associated with melanoma, but rather, sunburn doubled the risk of developing melanoma and intermittent, high-intensity sun exposure proposed a 61% increased risk for melanoma
Drs. Frank and Cedric Garland, both prominent figures in vitamin D and cancer research, were among the first to acknowledge the relationship between geographic location, sunshine exposure, and incidence of cancer. They, with their team of colleagues, published two now famous studies in The Lancet, a well-respected international medicine journal. Both studies showed markedly reduced incidence of colon cancer in populations with the highest intake of vitamin D and the highest serum concentrations of vitamin D. Additional studies describing the relationship between UVB exposure, sunlight, and vitamin D on the incidence of colon, breast, and ovarian cancer have also been published by the Garland brothers, with a recurring theme of decreased cancer risk with increased UVB and vitamin D.
Since then, research on the topic of sunshine exposure and cancer risk has exploded, with many new studies showing multiple health benefits to lifetime sensible sun and UVB exposure, including a decreased risk of melanoma and many other types of cancers. Several of these studies are highlighted below.
 Does sensible sun exposure cause melanoma?
Does sensible sun exposure cause melanoma?
Is there any evidence that regular, moderate, “sensible” sun exposure causes melanoma? Listen in to this snippet of an interview with Dr. Michael Holick as he explains.
 How do sunshine and vitamin D affect our health?
How do sunshine and vitamin D affect our health?
Humans were designed to be exposed to sunshine and to receive vitamin D from sun exposure. Watch this snippet of an interview with Dr. Michael Holick as he explains some of the unique health benefits of sunshine and vitamin D.
Decreased Risk of Breast Cancer
Research on breast cancer and vitamin D levels has shown that women with vitamin D levels at or above 60 ng/ml (150 nmol/L) had an 80% lower breast cancer risk compared to women with levels less than 20 ng/ml (50 nmol/L). Similar results have been found among women in the United Kingdom — an 83% lower breast cancer risk with vitamin D levels above 60 ng/ml. A 2019 meta-analysis by Song et al. analyzed data from 70 observational studies and found a 6% lower risk of developing breast cancer for every 2 ng/ml (5 nmol/L) increase in vitamin D blood levels.
In addition to higher vitamin D levels, long-term UV exposure has also been associated with a lower risk of breast cancer, especially among women diagnosed in older age. A study by Pedersen et al. found that long-term occupational UV exposure was associated with a reduced risk of late-onset breast cancer among Danish women, with longer durations and higher amounts of UV exposure contributing to a further decreased risk. This study found a 17% decreased risk for late-onset cancer with longer duration of UV exposure, and an 11% decreased risk with higher cumulative UV exposure. The researchers also found a 15% decreased risk overall associated with longer duration of UV exposure for all diagnosis ages combined.
A dose-response meta-analysis on UV exposure and breast cancer risk, by Yilun Li and Li Ma, aimed to quantify the relationship between the amount of UV exposure and breast cancer risk. They included six case-control studies and conducted a dose-response meta-analysis, with an additional analysis by age, sunscreen use, and limb coverage. A significant dose-response correlation between UV exposure and breast cancer risk was found, such that women in the highest exposure groups had a 30% lower risk of breast cancer compared to women in the lowest exposure groups. Overall, this study saw a negative correlation between UV exposure and breast cancer risk, especially among women over 40 years of age; women who did not tan or who covered their arms and legs while in the sun also had a higher risk of breast cancer.
Another study by Knight et al. included phone interviews from 972 women who had been diagnosed with invasive breast cancer and 1135 women without cancer. Questions about vitamin D intake, sun exposure, and other breast cancer risk factors were asked for each age group of 10 to 19, 20 to 29, and 45 to 54 years old. The authors found the strongest breast cancer risk reduction among the women with the highest amount of sun exposure and vitamin D intake during the ages of 10 to 19 years old, with a weaker association at 20 to 29 years old and no association for the oldest group. This study indicates that higher amounts of sunshine exposure and vitamin D during adolescence may help prevent the development of breast cancer later in life.
Decreased Risk of Colorectal Cancer
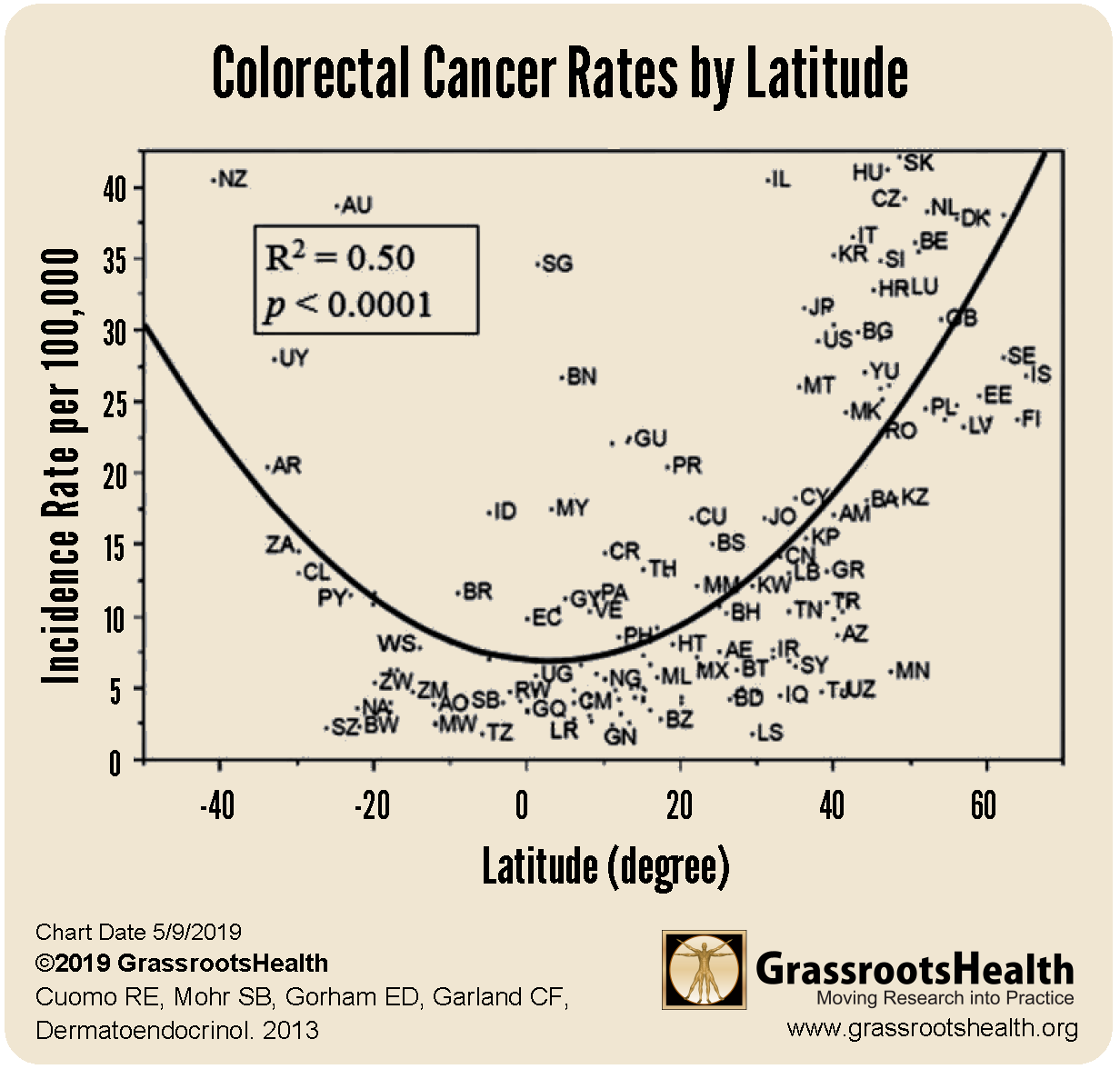
Rates of colorectal cancer, the third most common cancer worldwide and the second leading cause of cancer death, are higher further from the Equator across 173 countries (P<0.0001). Additionally, higher UVB irradiance was associated with lower colorectal cancer risk (P<0.0001) after adjusting for cloud cover and other relevant factors. The relationship is illustrated in the U-shaped “smiley” curve below, which shows higher disease rates in the far northern and southern latitudes – locations that have lower UVB irradiance from the sun. Countries that are closer to the Equator (presenting in the center of the horizontal axis around the 0 degree latitude) have higher UVB irradiance and tend to have lower disease rates.
Dr. Garland and his research team have also published similar results for lung and breast cancer, ovarian cancer, endometrial cancer, renal cancer, bladder cancer, pancreatic cancer, brain cancer, leukemia, and multiple myeloma.
“Colon cancer mortality rates are the highest in places where populations were exposed to the least amounts of natural light.” Dr. Cedric F. Garland
A study by Valles et al. found a 19% lower risk of colorectal cancer for participants who reported sun exposure of 2 or more hours per day compared to 1-2 hours per day in the prior summer, and that sun exposure and dietary vitamin D, both separately and together, could reduce colorectal cancer risk and be key to cancer prevention.
Decreased Risk of Gastric Cancer
A meta-analysis by Chen et al. looked at 11 different studies in total on gastric cancer to determine if there was a relationship between the incidence of gastric cancer and vitamin D intake, serum level, or solar UVB exposure. While the authors found that the risk of gastric cancer was not related to vitamin D intake or vitamin D level, they did conclude that there is a clear and significant decrease in the incidence of gastric cancer among those with higher amounts of UVB radiation. As stated by the authors, “Increasing evidence shows that UVB radiation could be a protective factor for gastric cancer. When considered in combination with vitamin D, sunlight, and cancer, the evidence is clear that exposure to UVB radiation could afford protection against cancer.”
Decreased Cancer Risk Overall
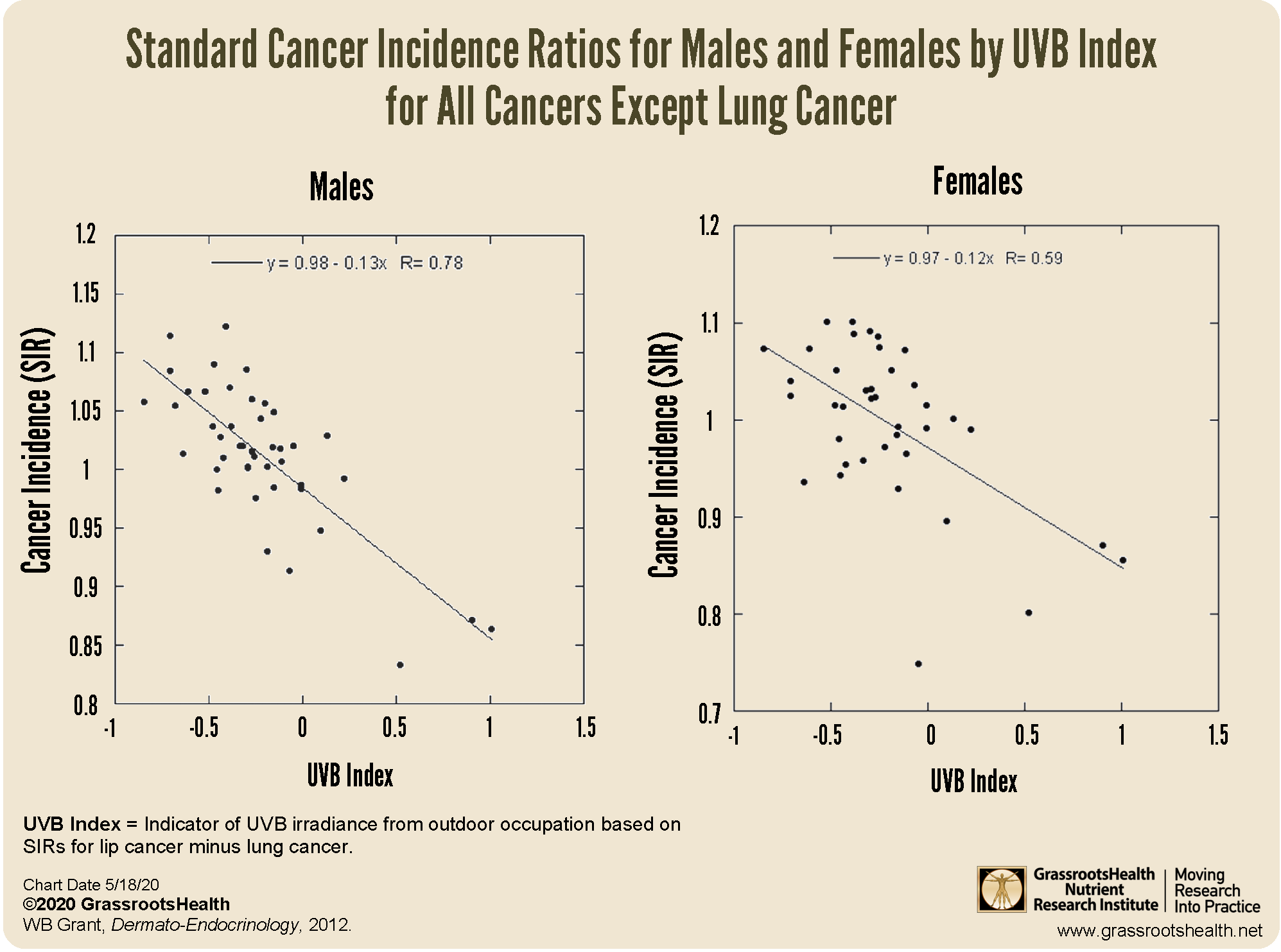
A 2012 study by Dr. William B. Grant looked at cancer data from five Nordic countries, between 1961 and 2005, to evaluate the relationship between solar UVB and cancer rates based on 54 different occupation categories. The occupation categories were further divided into those that were primarily outdoor versus those that were primarily indoor.
Findings differed among men and women, with a decreased incidence of several different types of cancer among those with higher UVB exposure. For men, 15 different cancers were significantly inversely correlated to UVB: bladder, breast, colon, gallbladder, kidney, laryngeal, liver, lung, oral, pancreatic, pharyngeal, prostate, rectal, small intestine cancer, and melanoma. For women, UVB was significantly inversely correlated to bladder, breast, colon and rectal cancer.
One of the most impressive studies on sunshine exposure and health outcomes by Lindqvist et al. found that the mortality rate for women who avoided sun exposure was two times higher than those with the highest sun exposure, with an intermediate mortality rate in those with moderate sun exposure. Key findings by Lindqvist et al. specific to cancer include
- Women with active sun exposure habits had a lower risk of death from cardiovascular disease, cancer, and causes of death other than cancer or heart disease, such as diabetes, multiple sclerosis and pulmonary disease
- A 40% higher risk of cancer-related death was seen among women with low sun exposure vs the greatest sun exposure
- Women who developed melanoma but had more life-time sun exposure were more likely to survive, with mortality rates of 36% among the low sun exposure group, 16% for moderate sun exposure, and 13% for those with the greatest sun exposure
- Compared to women with the highest sun exposure, life expectancy for women who avoided sun was shorter by 0.6 to 2.1 years
“Our study showed that there was a 40% higher risk of cancer related death in the group with low sun exposure as compared to those with greatest sun exposure. This can be attributed to the production of vitamin D or other beneficial health benefits from sun exposure.” Dr. Pelle Lindqvist
Decreased Risk of Melanoma
Regular, moderate, non-burning sunshine exposure and higher levels of vitamin D are shown to decrease (not increase) the risk of melanoma. In fact, WHO’s International Agency for Research on Cancer (IARC) published a detailed analysis of studies on sun exposure and melanoma and found that continuous, regular sun exposure was not associated with melanoma, but rather, sunburn doubled the risk of developing melanoma and intermittent, high-intensity sun exposure proposed a 61% increased risk for melanoma. More specifically, painful sunburns before the age of 20 seem to be a strong predictor of all types of skin cancer, while chronic or lifetime sun exposure has been associated with an increased risk of SCC but a decreased risk of BCC and melanoma, according to Rosso et al..
A comprehensive review by Gandini et al. on sun exposure and melanoma found a positive association between intermittent, high intensity sun exposure and increased risk for melanoma and an inverse association between high occupational sun exposure and risk for melanoma. In other words, chronic sun exposure, such as that among outdoor workers, reduced the risk of melanoma.
A paper by Bolerazska et al. emphasizes that the origin of malignant melanoma is due to sun burns in people who spend most of their time indoors, only getting sun exposure in excessive amounts over holidays (intermittent exposure). This is due to the finding that vitamin D synthesized in the skin can help protect against melanoma due to its involvement in DNA repair, cell differentiation, cell death, cell adhesion, and oxidative stress – all mechanisms involved in cancer development.
Are You Getting Enough Cancer-Fighting Vitamin D and Sensible Sunshine?
 Having and maintaining healthy vitamin D levels and other nutrient levels can help improve your health now and for your future. Choose which additional nutrients to measure, such as your omega-3s and essential minerals including magnesium and zinc, by creating your custom home test kit today. Take steps to improve the status of each of these measurements to benefit your overall health. With measurement you can then determine how much is needed and steps to achieve your goals. You can also track your own intakes, symptoms and results to see what works best for YOU.
Having and maintaining healthy vitamin D levels and other nutrient levels can help improve your health now and for your future. Choose which additional nutrients to measure, such as your omega-3s and essential minerals including magnesium and zinc, by creating your custom home test kit today. Take steps to improve the status of each of these measurements to benefit your overall health. With measurement you can then determine how much is needed and steps to achieve your goals. You can also track your own intakes, symptoms and results to see what works best for YOU.
Enroll in D*action and Test Your Levels Today!



 Does sensible sun exposure cause melanoma?
Does sensible sun exposure cause melanoma? How do sunshine and vitamin D affect our health?
How do sunshine and vitamin D affect our health?