Published on March 28, 2024
Learn how to assess the validity of conclusions made from published vitamin D research using the Heaney Nutrient Study Criteria
Key Points
- While randomized controlled trials (RCTs) are efficient ways to evaluate the effects of a drug (something that is not present in the human body unless taken), the RCT design is often not the best-suited study for nutrients; the fact is that many RCTs of nutrient effects, specifically with vitamin D, are poorly designed, a reason they can tend to lead to a finding of “no effect,” or a “null” result, when in fact, with a different design, the findings could have told a much different story
- Robert Heaney, MD, who spent much of his career doing research on vitamin D and other nutrients, developed and published a paper outlining specific criteria nutrient studies should follow in order to produce the most accurate and reliable study results, which are especially important when it comes to vitamin D
- We know, beyond a doubt, that vitamin D is essential for our health; the “Totality of Evidence” provides the “whole-picture proof” that vitamin D can benefit our musculoskeletal, immune, cardiovascular, cognitive, and overall health, and reduces the risk of many diseases
Negative news featuring findings from poorly designed studies on vitamin D continues to pop into the media spotlight, concluding that vitamin D supplements are useless and ineffective. The issue has gotten so bad that funding for vitamin D research has become majorly affected, as reported in detail by the Townsend Letter article, “Vitamin D: Scientific American Chimes in on ‘VITAL’ as Research Money Vanishes.” However, we know, beyond a doubt, that getting enough vitamin D is essential for our health. How can you tell what to believe?
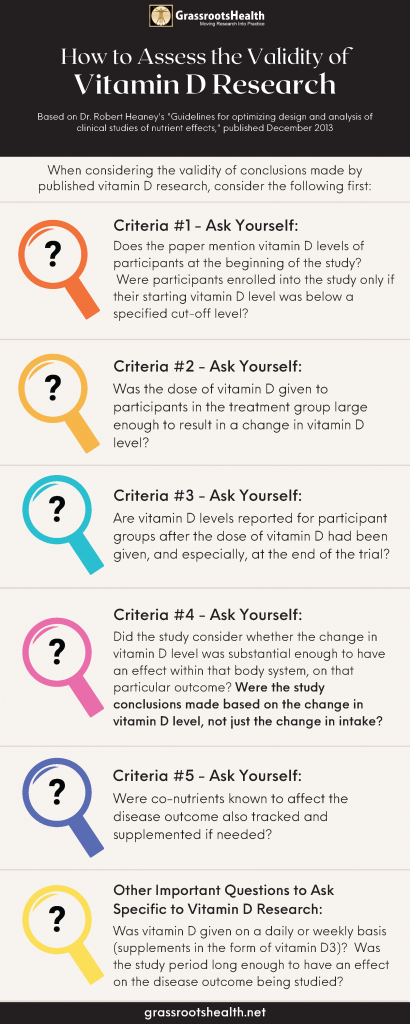
Below we describe, in detail, how to use Dr. Robert Heaney’s nutrient study criteria when approaching published nutrient research to determine what amount of validity the study conclusions hold. While there is a bit more to consider along with these criteria specific to vitamin D research, they can serve as an excellent starting guide on how to assess vitamin D research, each of which are summarized in the infographic here.
Download and Share on Social Media! (7 Images Total)
How Randomized Controlled Trials (such as the VITAL Trial) Fit into the Vitamin D Picture
In the medical science world, randomized controlled trials (RCTs) are considered the “gold-standard” study design to provide solid evidence that “something works.” Since there has been so much evidence and research supporting the role of vitamin D in health, researchers took what they thought was the next logical step to further clarify if and how vitamin D did have an effect on certain health outcomes – they designed and executed RCTs for vitamin D. Unfortunately, while RCTs are efficient ways to evaluate the effects of a drug (something that is not present in the human body unless taken), the RCT design is often not the best-suited study for nutrients. The fact is that many randomized controlled trials of nutrient effects are poorly designed, a reason vitamin D RCTs can tend to lead to a finding of “no effect,” or a “null” result, when in fact, with a different design, the findings could have told a much different story.
Using Dr. Heaney’s Nutrient Study Criteria for Implementing and Analyzing Vitamin D RCTs
To address issues arising from research such as this, Robert Heaney, MD, who spent much of his career doing research on vitamin D and other nutrients, developed and published a paper, “Guidelines for optimizing design and analysis of clinical studies of nutrient effects.” Each of the guidelines can be translated as follows to make them specific to vitamin D; ask yourself along the way if the vitamin D study you are questioning (such as the VITAL analysis on fracture risk) met the following criteria:
Criteria #1: Basal nutrient status must be measured, used as an inclusion criterion for entry into study, and recorded in the report of the trial.
What does this mean for vitamin D studies?
a) Measure vitamin D levels [as 25(OH)D] for all participants at the beginning of the trial (this is the baseline level or basal nutrient status)
b) Baseline levels should be an inclusion criterion for participating in the study, so that the study enrolls only those with beginning vitamin D levels below the response range for the disease outcome to be observed (typically below 20 ng/ml or 50 nmol/L for most diseases)
Measuring vitamin D levels at the beginning of a study is essential to defining a starting point, telling the researchers how much vitamin D participants are already getting (from supplements as well as sun/UVB and food), and whether they might already be getting enough to fulfill certain needs within the body. Baseline vitamin D status should therefore be an inclusion criterion, with the study enrolling only participants with deficient vitamin D levels, or levels below a known response range for the desired outcome (typically below 20 ng/ml or 50 nmol/L for bone health).
Criteria #2: The intervention (i.e. change in nutrient exposure or intake) must be large enough to change nutrient status and must be quantified by suitable analyses.
What does this mean for vitamin D studies?
The intervention (whether it is supplementation, UVB exposure, or other) should include a sufficient dose of vitamin D to raise vitamin D levels among most treatment group participants into the therapeutic range (40-60 ng/ml or 100-150 nmol/L for many conditions)
To determine if an intervention (dose of vitamin D) is great enough to have a specific effect (change in vitamin D level), baseline and follow-up levels must be measured.
How much is enough? Remember, one dose does not fit for all. Everyone responds differently to vitamin D… by up to 6 times for the same supplement amount.
Certain factors can influence how an individual’s vitamin D level responds to their vitamin D supplementation amount (called the dose-response). These factors can cause a wide range of serum level responses that can be produced when looking at any specific supplementation amount. For example, it is possible for a supplemental intake of 4000 IU/day to result in a serum level of 25 ng/ml (62.5 nmol/L) in one individual, and 60 ng/ml (150 nmol/L) in another – making measuring the resulting vitamin D level (Criteria #3) essential to knowing whether an individual is getting an appropriate dose or if that dose needs to be adjusted.
Criteria #3: The change in nutrient status produced in those enrolled in the trials must be measured and recorded in the report of the trial.
What does this mean for vitamin D studies?
Vitamin D levels must continue to be measured and recorded at time points during the trial, and at the end of the trial
Follow-up or achieved vitamin D levels must be measured among all participants. Skipping this step makes determining a change in nutrient status impossible.
Criteria #4: The hypothesis to be tested must be that a change in nutrient status (not just a change in intake) produces the sought-for-effect.
What does this mean for vitamin D studies?
a) The hypothesis should be that increased vitamin D levels into the therapeutic range (40-60 ng/ml for many conditions) will produce the specified effect (less disease, reduced symptoms, etc.)
b) The vitamin D level, not just the vitamin D dose, must be considered in the analysis
The hypothesis should be that increased vitamin D levels into the therapeutic range, not the dose amount, will produce the specified effect (less disease, reduced symptoms, etc.). This premise is often the core problem; since vitamin D synthesis varies greatly for each person, the hypothesis cannot be by treatment amount (supplement intake) but instead needs to be investigated around achieving a certain serum level.
We have seen this mistake made over and over again with trials that associate findings with a dose instead of an achieved vitamin D level. An example of the difference in findings is the Wagner et al. study on preterm birth, which when re-evaluated by serum level instead of dose, found a much different, positive benefit for vitamin D.
Criteria #5: Co-nutrient status must be optimized in order to ensure that the test nutrient is the only nutrition-related, limiting factor in the response.
What does this mean for vitamin D studies?
Co-nutrients affecting the study outcome should also be optimized; for vitamin D studies, these could include calcium, vitamin K2, and magnesium among others. (Calcium levels and urine calcium/creatinine levels can also be measured at the same time points as vitamin D levels for safety.)
Co-nutrients are nutrients that work together for some process. If one co-nutrient is limited, either missing or not plentiful enough, then the process might also be limited or not able to take place at all. While this criteria is not a reason to throw out a study, it would be best to optimize co-nutrients to more clearly define the effect of the nutrient in question.
The charts included in the blog here illustrate how co-nutrient status can affect a target outcome such as bone status. When any or all nutrients are below the optimal level, bone status is impaired at the level of the lowest, or most limited, nutrient (even if vitamin D itself has been optimized).
Other Important Questions to Ask Specific to Vitamin D Studies
Dosing Frequency
Vitamin D RCTs should avoid bolus dosing (doses given monthly or longer). Vitamin D given on a daily or weekly basis (and in the form of vitamin D3) in doses the body can make from the sunshine (not much more than 25,000 – 50,000 IU at any given time) would better match how vitamin D is intended to be ‘received’ in our bodies. It is not possible to make 100,000 IU of vitamin D in a single day, and studies doing so are more likely to have negative findings.
Length of Study
It takes time to change nutrient levels within the body, and for that change to have an effect on disease status. For example, it can take up to 20 years for precancerous cells to develop into detectable cancer. A study that lasts only 3-5 years cannot conclusively determine that vitamin D supplementation does not prevent cancer. A study period less than or equal to 6 months of testing for chronic conditions and disease prevention could basically be considered useless.
Picking Apart Vitamin D Research – Does ‘This’ Study Meet the Criteria?
As you consider the validity of findings from vitamin D research, remember to analyze it according to the nutrient study criteria above. What do you think after applying the Heaney nutrient study criteria to the research study in question? Take a look at research with the criteria in mind and ask yourself: Did this study meet the Heaney nutrient study criteria?
Also remember, the “Totality of Evidence” provides the “whole-picture proof” that vitamin D is essential to our musculoskeletal, immune, cardiovascular, cognitive, and overall health, and reduces the risk of many diseases. Knowledge of human physiology has proven there is a demand for vitamin D within our cells for a multitude of every-day processes. Mechanistic studies have demonstrated how vitamin D works within the cells, tissues, organs, and the body as a whole to directly influence health and the development or regression of many skeletal and non-skeletal diseases. We see the effects of vitamin D demonstrated in observational and epidemiological studies over and over, with disease risk, prevalence, and outcome consistently related to vitamin D levels for many different types of diseases.
Vitamin D is an Easily Modifiable Factor to Help Improve Disease Outcomes – What Vitamin D Level do YOU Have?
Don’t ever consider a situation too late to take steps for correcting or avoiding vitamin D deficiency. Measuring your vitamin D level and calculating a supplementation amount to help reach and maintain a target level, or taking loading doses to correct deficiency faster, could possibly make all the difference in how a current disease situation progresses.
 Create your custom home blood spot kit by adding any of the following measurements, along with your vitamin D:
Create your custom home blood spot kit by adding any of the following measurements, along with your vitamin D:
- Magnesium PLUS Elements
- Omega-3 Fatty Acids
- hsCRP (for Inflammation)
- HbA1c (for Blood Sugar)
- and more
Having and maintaining healthy vitamin D levels and other nutrient levels can help improve your health and the health of your baby, now and for the future. Enroll and test your levels today, learn what steps to take to improve your status of vitamin D (see below) and other nutrients and blood markers, and take action! By enrolling in the GrassrootsHealth projects, you are not only contributing valuable information to everyone, you are also gaining knowledge about how you could improve your own health through measuring and tracking your nutrient status, and educating yourself on how to improve it.