Published on May 9, 2022
Regular, moderate sunshine exposure and higher levels of vitamin D are shown to decrease (not increase) the risk of melanoma, which is now being overdiagnosed
Key Points
- Though painful sunburns before the age of 20 seem to be a strong predictor of all types of skin cancer, chronic or lifetime sun exposure has been associated with an increased risk of squamous cell carcinoma but a decreased risk of basal cell carcinoma and melanoma
- Several publications have reported an overdiagnosis of melanoma, including Adamson et al., 2022, who stated “More than one-half of the melanomas diagnosed in White patients in 2014 were estimated to represent overdiagnosis;” other publications suggest that the prevalence of melanoma caused by UV exposure has also been grossly overestimated
- Vitamin D made in the skin upon UVB exposure may protect against melanoma due to its involvement in DNA repair, cell differentiation, cell death, cell adhesion, and oxidative stress; studies have found relationships between lower vitamin D levels and increased incidence of melanoma, melanoma mortality, and tumor thickness
 There are three primary types of skin cancer: basal cell carcinoma (BCC), squamous cell carcinoma (SCC), and melanoma. According to the American Cancer Society, a vast majority of skin cancers are non-melanoma skin cancers, with BCC accounting for approximately 80% of cases and SCC ~20%. These non-melanoma skin cancers usually grow slowly, rarely spread to other parts of the body, and are very treatable, with skin cancer and melanoma deaths making up only 0.4% of all deaths.
There are three primary types of skin cancer: basal cell carcinoma (BCC), squamous cell carcinoma (SCC), and melanoma. According to the American Cancer Society, a vast majority of skin cancers are non-melanoma skin cancers, with BCC accounting for approximately 80% of cases and SCC ~20%. These non-melanoma skin cancers usually grow slowly, rarely spread to other parts of the body, and are very treatable, with skin cancer and melanoma deaths making up only 0.4% of all deaths.
Despite public health messages to the contrary, not all skin cancers, particularly melanomas and basal cell carcinomas, are directly attributable to moderate sun exposure. Though painful sunburns before the age of 20 seem to be a strong predictor of all types of skin cancer, chronic or lifetime sun exposure has been associated with an increased risk of SCC but a decreased risk of BCC and melanoma (Rosso et al., 1996).
Overdiagnosis of both Melanoma and UV Exposure as its Cause
Melanoma accounts for approximately 1-7% of all skin cancers (depending on the country) and is more dangerous because it is more likely to spread to other parts of the body if not caught early. However, the overdiagnosis of melanoma has been reported in several recent publications, including Welch et al., 2021, Kerr et al., 2022, and Adamson et al., 2022 who stated “More than one-half of the melanomas diagnosed in White patients in 2014 were estimated to represent overdiagnosis.” To clarify, overdiagnosis is when a person receives a diagnosis for a disease that will not actually harm them during their lifetime, and it often leads to receiving and paying for unnecessary treatments, as well as a great deal of mental, emotional, and physical stress. For melanoma, this often happens when a skin abnormality is taken as a precursor for melanoma, when in fact it was and would have remained nothing more than an abnormality.
Other publications suggest that the prevalence of melanoma caused by UV exposure has also been grossly overestimated. A recent cross-sectional study by Mata et al., 2022, of 343,589 patients with solid tumors looked at UV mutational signatures as a biomarker for identifying cancers caused by genomic alterations due to UV exposure. They found that UV exposure accounts for 9 times less melanoma than what has previously been reported (11% vs 95%).
Regular, Moderate Sunshine Exposure is Good; Sun Burns and Intermittent, High-Intensity Exposure is Bad
Compared to regular, moderate, non-burning exposure to sunshine, intermittent, or sudden, drastic exposure to high intensity sunlight (which results in sunburn) is more likely to lead to unresolved local DNA damage which then increases the risk for melanoma. In fact, WHO’s International Agency for Research on Cancer (IARC) published a detailed analysis of studies on sun exposure and melanoma and found that continuous, regular sun exposure was not associated with melanoma, but rather, sunburn doubled the risk of developing melanoma and intermittent, high-intensity sun exposure proposed a 61% increased risk for melanoma. More specifically, painful sunburns before the age of 20 seem to be a strong predictor of all types of skin cancer, while chronic or lifetime sun exposure has been associated with an increased risk of SCC but a decreased risk of BCC and melanoma, according to Rosso et al..
Moreover, a comprehensive review by Gandini et al. on sun exposure and melanoma found a positive association between intermittent, high intensity sun exposure and increased risk for melanoma and an inverse association between high occupational sun exposure and risk for melanoma. In other words, chronic sun exposure, such as that among outdoor workers, reduced the risk of melanoma.
Decreased Incidence and Increased Melanoma Survival Rates are Related to Regular Sun Exposure and Higher Vitamin D Levels
Studies surrounding the synthesis of vitamin D in the skin and its effect on malignant melanoma have found that vitamin D may protect against melanoma due to its involvement in DNA repair, cell differentiation, cell death, cell adhesion, and oxidative stress – all mechanisms involved in cancer development. One such paper by Bolerazska et al. (2017) also emphasizes that the origin of malignant melanoma is due to sun burns in people who spend most of their time indoors, only getting sun exposure in excessive amounts over holidays (intermittent exposure).
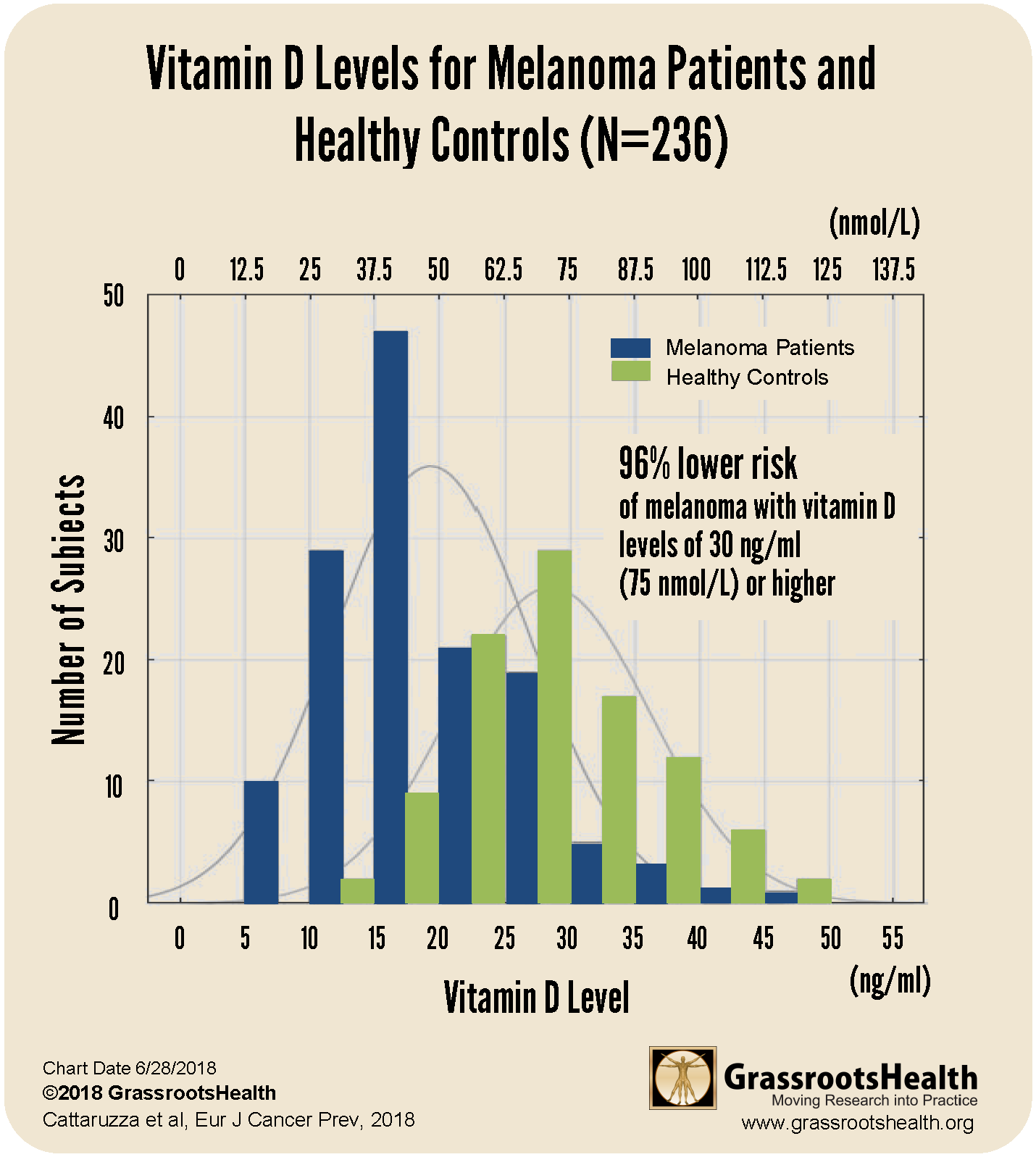
Results from a 2018 case-control study by Cattaruzza et al. showed a clear decrease in melanoma risk as vitamin D levels increased, as illustrated in the chart below.
This study included 137 melanoma patients and 99 healthy controls. The research team found that the average vitamin D level of melanoma patients was lower than the average level of the healthy controls by 10 ng/ml (25 nmol/L) and that the majority of melanoma patients had vitamin D levels at or below 20 ng/ml (50 nmol/L) compared to just 15% of the healthy controls. Furthermore, participants with vitamin D levels at or above 30 ng/ml (75 nmol/L) had a 96% lower risk of melanoma compared to participants with levels at or below 20 ng/ml (50 nmol/L) after adjusting for age, sex and BMI.
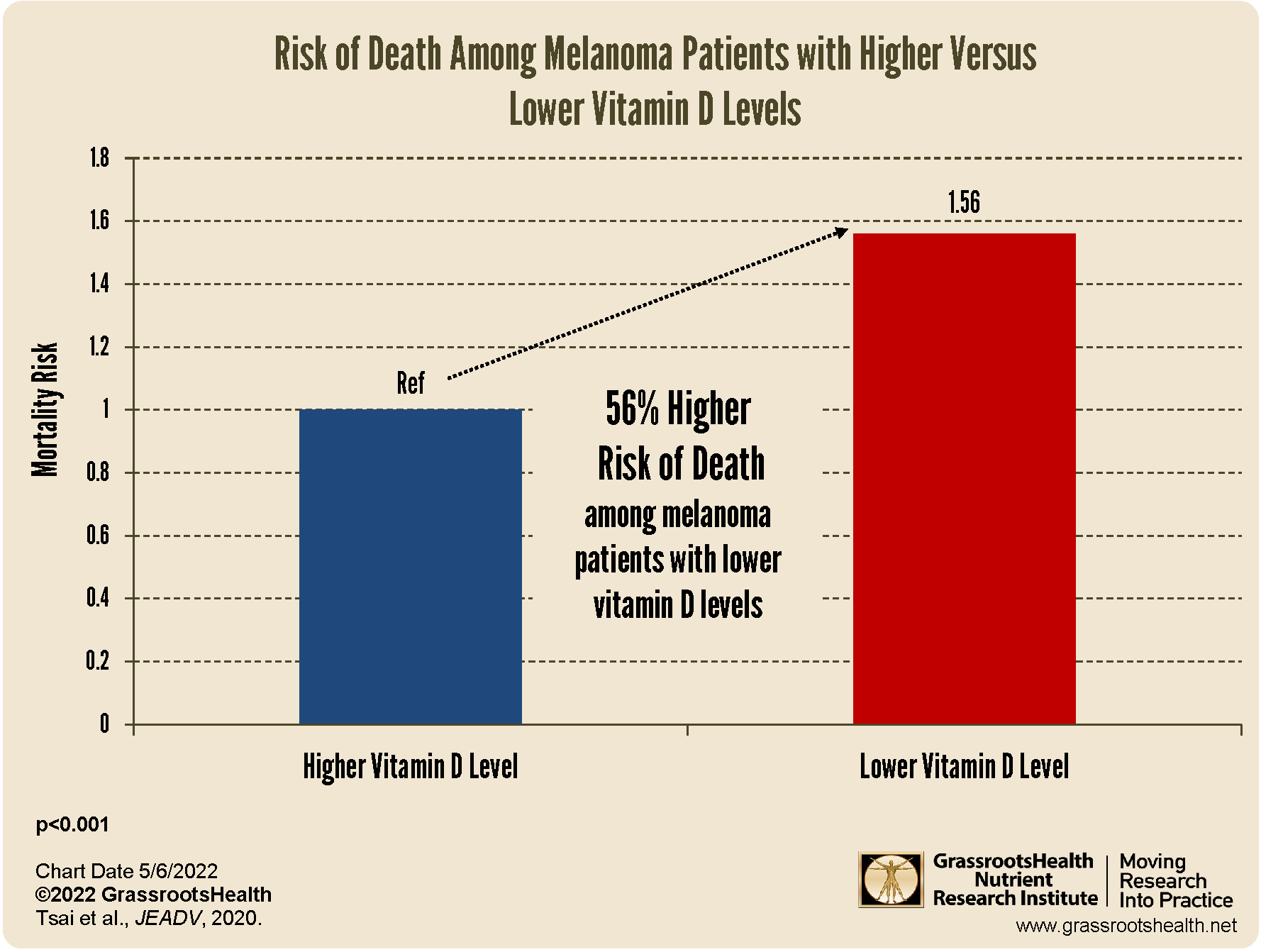
A meta-analysis by Tsai, Kuo et al. 2020 found that melanoma patients with lower vitamin D levels had a 56% higher mortality rate compared to those with higher vitamin D levels, as shown in the chart below.
The authors looked at 25 studies, with a total of 11,166 melanoma patients, to evaluate the relationship between melanoma risk and prognosis, and vitamin D levels. They found that vitamin D deficiency was more prevalent among melanoma patients compared to controls (P<0.001), and melanoma patients had a significantly higher mortality rate if they had lower vitamin D levels compared to higher vitamin D levels (P<0.001). They also found that tumor thickness was significantly related to vitamin D level, with a thickness of 1 millimeter (mm) or less related to a higher vitamin D level and a tumor thickness of greater than 1 mm much more likely with lower vitamin D levels (P<0.001).
Balance Your Risks with the Benefits of Sunshine Exposure and Vitamin D
The sunshine provides many health benefits beyond vitamin D. Exposure to the sun helps the body produce other important chemicals and nutrients, such as nitric oxide, melatonin, serotonin, and beta-endorphins; it helps regulate our circadian rhythm (or our body’s “master clock”) and it even has a positive effect on the microbes that live on our skin and in our gut. Implementing regular, safe, non-burning sun exposure can help individuals of all skin types maximize the health benefits from the sun while minimizing the risks associated with sun exposure, including that of melanoma. Ensuring adequate vitamin D levels while developing and maintaining a sunshine routine is essential to supporting the health of the skin and overall health, and checking to make sure levels are in the recommended 40-60 ng/ml (100-150 nmol/L) range is the first step.
Start by Making Sure You are Getting Enough Vitamin D TODAY!
 Having and maintaining healthy vitamin D levels and other nutrient levels can help improve your health now and for your future. Choose which additional nutrients to measure, such as your omega-3s and essential minerals including magnesium and zinc, by creating your custom home test kit today. Take steps to improve the status of each of these measurements to benefit your overall health. With measurement you can then determine how much is needed and steps to achieve your goals. You can also track your own intakes, symptoms and results to see what works best for YOU.
Having and maintaining healthy vitamin D levels and other nutrient levels can help improve your health now and for your future. Choose which additional nutrients to measure, such as your omega-3s and essential minerals including magnesium and zinc, by creating your custom home test kit today. Take steps to improve the status of each of these measurements to benefit your overall health. With measurement you can then determine how much is needed and steps to achieve your goals. You can also track your own intakes, symptoms and results to see what works best for YOU.
Enroll in D*action and Test Your Levels Today!