Published on September 6, 2022
Studies demonstrate that both vitamin D and magnesium levels can individually affect the risk of atrial fibrillation
Key Points
- Atrial fibrillation affects an estimated 2.7 million Americans or more, and can lead to serious complications such as blood clots, stroke, heart failure, and other cardiovascular diseases, which may be fatal; since some people have no apparent symptoms, it often goes un-diagnosed
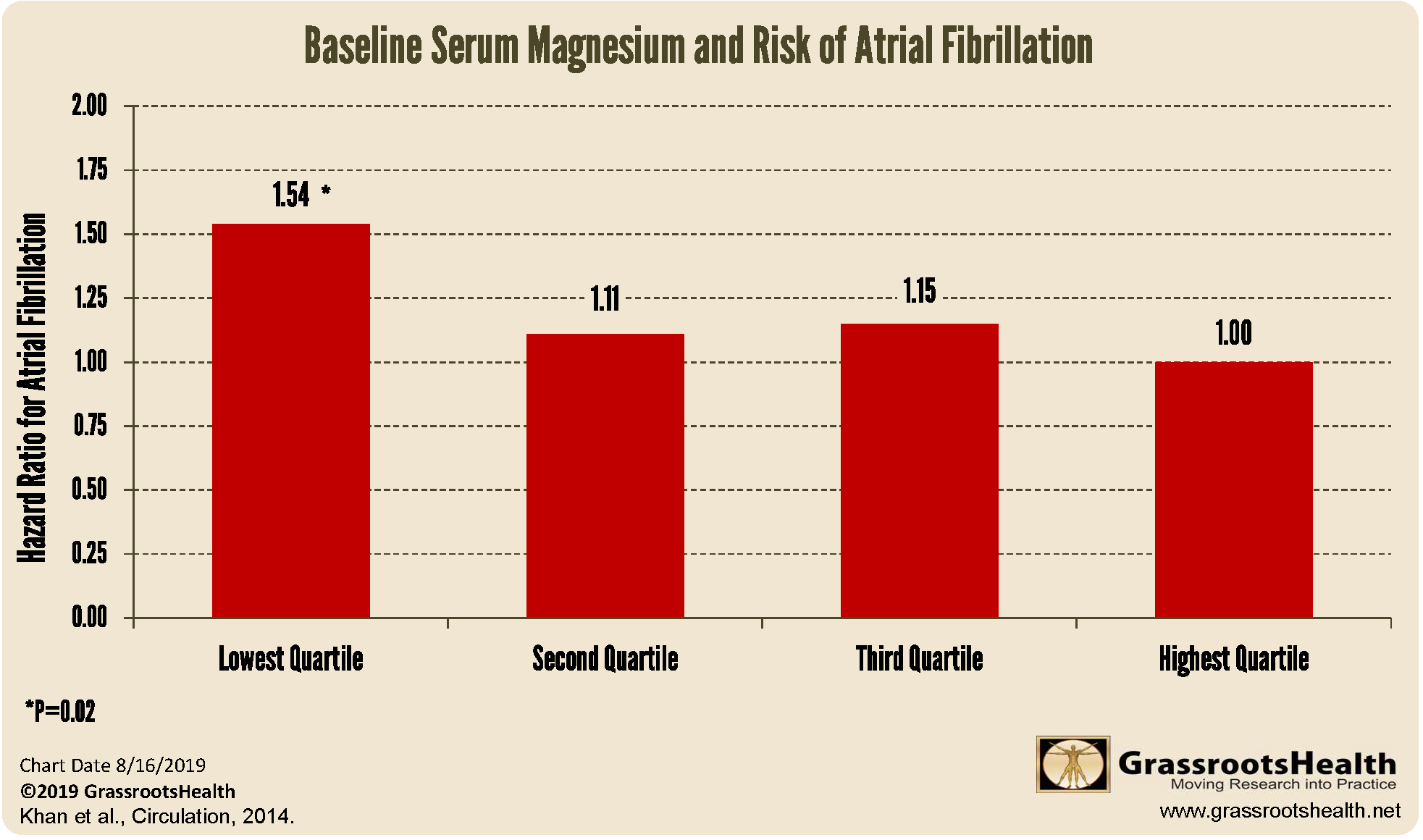
- Several studies have linked magnesium to the incidence and development of atrial fibrillation, with increased incidence seen among those having the lowest levels of serum magnesium
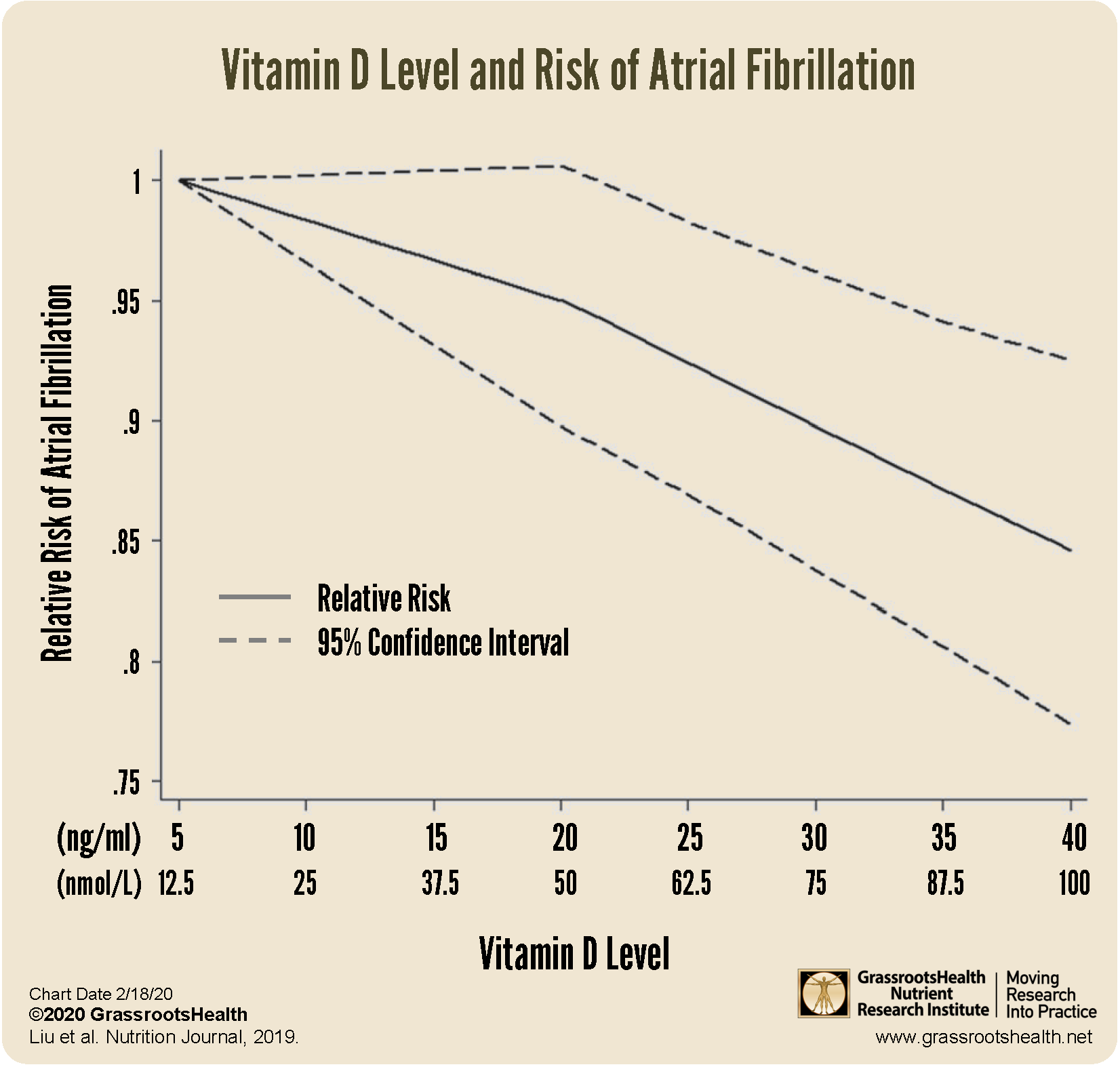
- A meta-analysis found that the risk of atrial fibrillation went down as vitamin D levels increased; in fact, for each 10 ng/ml (25 nmol/L) increase in vitamin D there was an additional risk reduction of 12%
 September is Atrial Fibrillation Awareness Month. Atrial fibrillation (also called Afib or AF), is an irregular, often rapid heart rate that can cause symptoms such as heart palpitations, shortness of breath, and weakness. It is associated with an increased risk of heart disease, and is the most commonly seen form of cardiac arrhythmia in clinical practice. Atrial fibrillation affects an estimated 2.7 million Americans or more, and can lead to serious complications such as blood clots, stroke, heart failure, and other cardiovascular diseases, which may be fatal. Since some people have no apparent symptoms, it often goes un-diagnosed.
September is Atrial Fibrillation Awareness Month. Atrial fibrillation (also called Afib or AF), is an irregular, often rapid heart rate that can cause symptoms such as heart palpitations, shortness of breath, and weakness. It is associated with an increased risk of heart disease, and is the most commonly seen form of cardiac arrhythmia in clinical practice. Atrial fibrillation affects an estimated 2.7 million Americans or more, and can lead to serious complications such as blood clots, stroke, heart failure, and other cardiovascular diseases, which may be fatal. Since some people have no apparent symptoms, it often goes un-diagnosed.
Magnesium Known to Affect Heart Rate
Magnesium plays several functional roles within cardiac muscle to regulate heart rate and contractions. It helps control the sodium-potassium pump within the cell membranes that causes the muscles of the heart to pump. It has been shown to extend the refractory period of the heart muscle, which is the relaxation time after the heart muscle pumps. In some studies, it has even been more effective at restoring the heart’s rhythm than standard pharmaceutical treatments.
Magnesium and Atrial Fibrillation
Several studies have linked magnesium to the incidence and development of AF. An analysis by Khan et al. used data from the Framingham Offspring Study, which involved more than two decades of data from a total of 3,530 participants, to look at the link between serum magnesium and the development of AF in those without existing cardiovascular disease. Over the time of the analysis, 5% of participants developed AF. The incidence of AF was highest in the quartile with the lowest magnesium level (P=0.02); no additional improvement was shown as serum magnesium rose beyond the level of the second quartile, suggesting there is a threshold serum magnesium level at which no further effect on AF can be seen.
The measurement for magnesium used in this study was the serum magnesium level, which is different than the RBC magnesium measurement in the Elements Panel, offered by GrassrootsHealth. Also note that the RBC magnesium test is a more accurate measurement of magnesium status than serum magnesium.
Similar Relationship found with Vitamin D Levels
A meta-analysis published by Liu et al. looked at 13 studies with 6519 cases of AF among 74,885 participants in total. The goal of the analysis was to identify a dose-specific relationship between vitamin D level and the risk of AF or postoperative atrial fibrillation (POAF).
The findings can be summarized as follows:
- Vitamin D deficiency (defined as <20 ng/ml or <50 nmol/L, p=0.008) and vitamin D insufficiency (21-29 ng/ml or 52.5-72.5 nmol/L, p=0.03) were both associated with an increased risk of AF
- For each 10 ng/ml (25 nmol/L) increase in vitamin D there was an additional risk reduction of 12% (p=0.03)
- Individuals aged 65 and older experienced a greater risk reduction in AF with higher vitamin D than younger individuals
- Increased vitamin D levels were also associated with a decreased incidence of POAF
As is clearly illustrated in the chart above, the relative risk of AF goes down as vitamin D levels go up.
Are you Getting Enough Vitamin D AND Magnesium for Your Heart?
Create your custom home blood spot kit by adding any of the following measurements, along with your vitamin D:
- Omega-3 Index (with or without Ratios AA:EPA and Omega-6:Omega-3)
- Magnesium (with or without additional Elements – copper, zinc, selenium, mercury, cadmium, lead)
- hsCRP as a marker of inflammation and HbA1c as a marker of blood sugar health
Having and maintaining healthy vitamin D levels and other nutrient levels can help improve your health, now and for the future. Enroll and test your levels today, learn what steps to take to improve your status of vitamin D (see below) and other nutrients and blood markers, and take action! By enrolling in the GrassrootsHealth projects, you are not only contributing valuable information to everyone, you are also gaining knowledge about how you could improve your own health through measuring and tracking your nutrient status, and educating yourself on how to improve it.