Published on May 11, 2020
Skin damage and skin cancer are usually the top concerns associated with sun exposure. Contrary to public health opinion, research shows that not all skin cancers are directly attributed to sun exposure. Skin type, UV index, and duration of time spent in the sun are all important factors to consider when talking about sun exposure and increased risk for skin cancer, such as melanoma.
Skin type, DNA damage, and melanoma
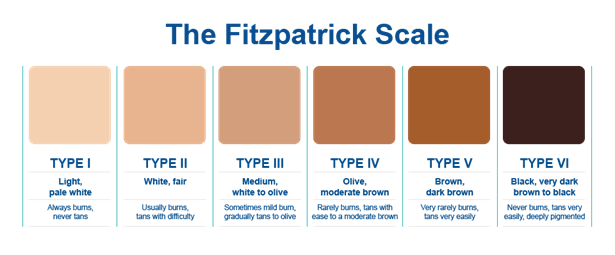
 The differences in risk for developing melanoma are strongly associated with skin phenotype, or pigment of the skin. Individuals with fair complexion have the greatest risk for developing melanoma because they burn easily, whereas individuals with darker complexion are less likely to burn. This is because darker skin contains more melanin – a pigment that acts as natural sunscreen. While the amount of melanin in your skin is primarily genetic, it can also gradually increase through sensible sun exposure.
The differences in risk for developing melanoma are strongly associated with skin phenotype, or pigment of the skin. Individuals with fair complexion have the greatest risk for developing melanoma because they burn easily, whereas individuals with darker complexion are less likely to burn. This is because darker skin contains more melanin – a pigment that acts as natural sunscreen. While the amount of melanin in your skin is primarily genetic, it can also gradually increase through sensible sun exposure.
A study which aimed to identify the levels of sun exposure that generate vitamin D with minimal skin damage found that both vitamin D and DNA damage were produced across all skin types. They also found that the depth of DNA damage within the skin differed by skin type. Those with the darkest skin had DNA damage only in the surface layers of the skin whereas those with the lightest skin had DNA damage across all skin layers. The DNA damage in the deeper layers of the skin may explain why those with a fair phenotype have higher skin cancer rates. Studies, including those highlighted in this review article, have shown that vitamin D produced in the skin can decrease DNA damage in the skin cells and facilitate DNA repair directly upon any UV damage, and help prevent cell death.
Since skin type influences sunburns and sunburns are associated with increased risk for melanoma, it is important to know your skin type to personalize your sun exposure. The Fitzpatrick scale below classifies six skin types based on the response of different skin types to UV radiation.
Higher vitamin D levels are associated with decreased melanoma risk
There are three primary types of skin cancer: basal cell carcinoma (BCC), squamous cell carcinoma (SCC), and melanoma. According to the American Cancer Society, a vast majority of skin cancers are non-melanoma skin cancers, with BCC accounting for approximately ~80% of cases and SCC ~20%. These non-melanoma skin cancers usually grow slowly, rarely spread to other parts of the body, and are very treatable.
Melanoma accounts for approximately 1-7% of all skin cancers (depending on the country) and is more dangerous because it is more likely to spread to other parts of the body if not caught early. Despite public health messages to the contrary, not all skin cancers, particularly melanomas and basal cell carcinomas, are directly attributable to moderate sun exposure. Though painful sunburns before the age of 20 seem to be a strong predictor of all types of skin cancer, chronic or lifetime sun exposure has been associated with an increased risk of SCC but a decreased risk of BCC and melanoma.
Bolerazska et al. (2017) reported the current knowledge surrounding the synthesis of vitamin D in the skin and its effect on malignant melanoma and found that vitamin D may protect against melanoma due to its involvement in DNA repair, cell differentiation, cell death, cell adhesion, and oxidative stress – all mechanisms involved in cancer development. The paper emphasizes that the origin of malignant melanoma is due to sun burns in people who spend most of their time indoors, only getting sun exposure in excessive amounts over holidays (intermittent exposure).
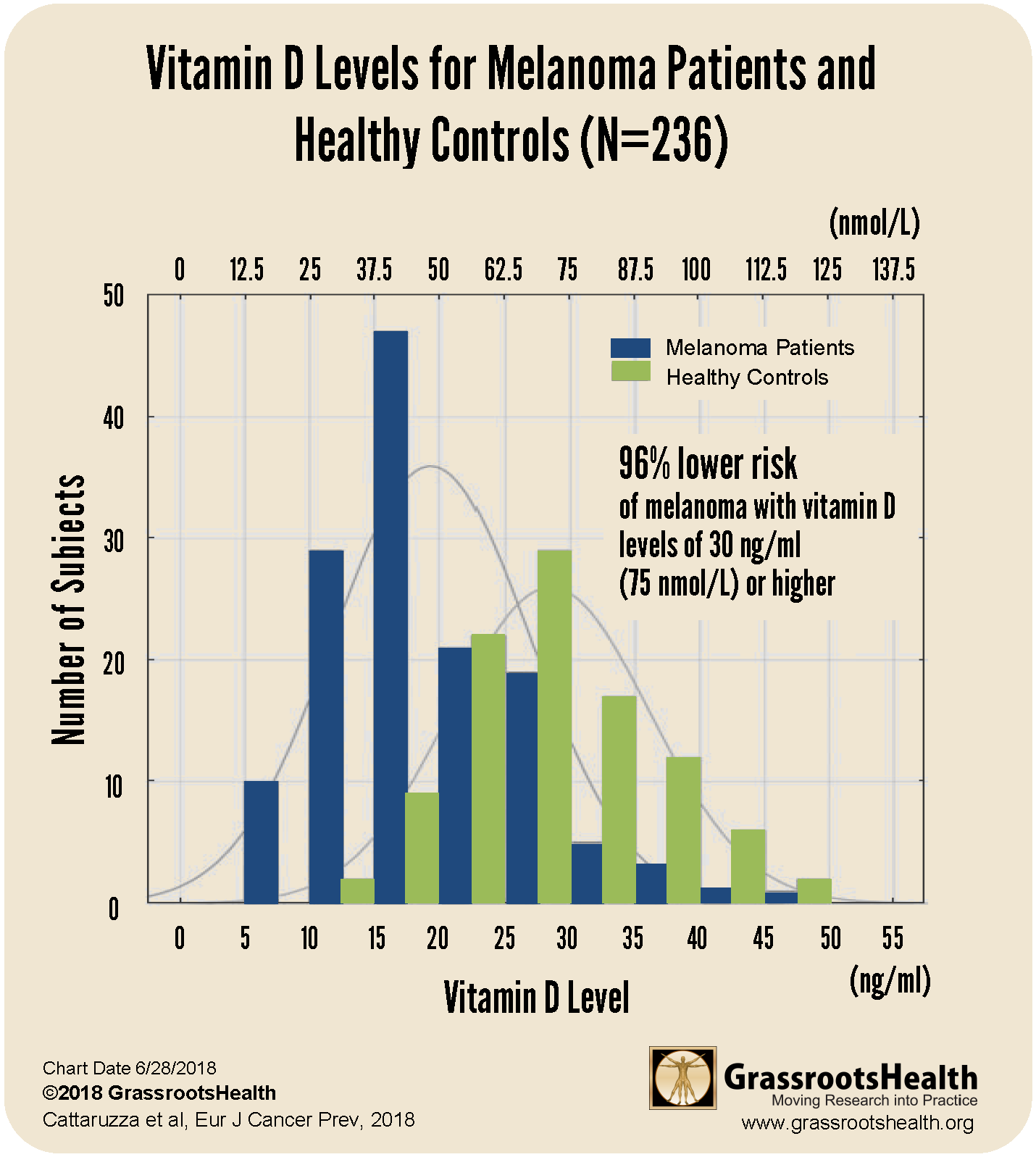
Results from a case-control study by Cattaruzza et al. showed a clear decrease in melanoma risk as vitamin D levels increased, as illustrated in the chart above. The study included 137 melanoma patients and 99 healthy controls. The research team found that the average vitamin D level of melanoma patients was lower than the average level of the healthy controls by 10 ng/ml (25 nmol/L) and that the majority of melanoma patients had vitamin D levels at or below 20 ng/ml (50 nmol/L) compared to just 15% of the healthy controls. Furthermore, participants with vitamin D levels at or above 30 ng/ml (75 nmol/L) had a 96% lower risk of melanoma compared to participants with levels at or below 20 ng/ml (50 nmol/L) after adjusting for age, sex and BMI.
Sun burns and intermittent, high-intensity sun exposure increase risk for melanoma
WHO International Agency for Research on Cancer (IARC) published a detailed analysis of studies on sun exposure and melanoma and found that continuous, regular sun exposure was not associated with melanoma, but rather, sunburn doubled the risk of developing melanoma and intermittent, high-intensity sun exposure proposed a 61% increased risk for melanoma. Moreover, a comprehensive review by Gandini et al. on sun exposure and melanoma found a positive association between intermittent, high intensity sun exposure and increased risk for melanoma and an inverse association between high occupational sun exposure and risk for melanoma.
Intermittent, or sudden, drastic exposure to high intensity sunlight, is more likely to result in local DNA damage which can increase risk for melanoma over time, compared to regular, moderate, non-burning exposure to sunshine.
Do You Have Enough Vitamin D to Support a Healthy Immune System?
We’re in a time of great crisis that could be greatly affected by making sure you and everyone you know has a serum level of at least 40 ng/ml. Help us help you.
Do you know what your vitamin D level is? Be sure to test today to find out, and take steps to keep it within a target of 40-60 ng/ml or 100-150 nmol/L! Give your immune system the nutrients it needs to support a healthy you and protect yourself from unnecessary diseases.
GrassrootsHealth is prepared to move forward by using science to drive global action, with using either clinical trials with our key researchers or by doing community Field Trials with individuals or other organizations. Please let us know if you are interested and how we can quickly setup your projects.
Through GrassrootsHealth Nutrient Research Institute, you can also test your essential elements magnesium, copper, zinc and selenium, toxins such as lead, mercury and cadmium, as well as your omega-3 levels, inflammation levels and thyroid stimulating hormone (TSH) level. Find out your levels today! Log on to the test selection page (click the link below) to get your tests and see for yourself if your levels can be improved.
Make sure you track your results before and after, about every 6 months!
Click Here to Access the Test Page
How can I track my nutrient intake and levels over time?
To help you track your supplement use and nutrient levels, GrassrootsHealth has created the Personal Health Nutrient Decision System called
For each specific supplement, you can track what days you take it, how much, and many other details. This will help you know your true supplemental intake and what patterns of use work for you to reach and maintain optimum nutrient levels. Check it out today!