Published on January 23, 2023
Some of the most compelling evidence of the need for a minimum vitamin D level of 40 ng/ml (100 nmol/L)… How fulfilling the unique need for vitamin D during pregnancy can impact prenatal, newborn & lifelong health
Key Points
- During pregnancy, conversion of 25(OH)D to the hormonal form, 1,25(OH)2D, increases so that by 12 weeks, levels in the blood are triple that of normal, non-pregnant female and normal male subjects; in a non-pregnant person, these levels would result in toxicity and potential death, but these are perfectly normal levels during pregnancy that are only allowed to optimize with a minimum 25(OH)D vitamin D level of 40 ng/ml
- When there is enough vitamin D3 available during pregnancy, 25(OH) vitamin D levels are allowed to rise and peak towards the end of pregnancy; this peak is prevented when vitamin D3 is limited and vitamin D levels are too low
- Globally, there is a high prevalence of deficiency among pregnant women; one study found 10% of all, 51% of women born in Africa, and 46% of women born in Asia were severely deficient (<12 ng/ml or <30 nmol/L)
Did you know? By week 12, a pregnant woman’s body converts more vitamin D than ‘normal,’ so that the level of the hormonal form of vitamin D [1,25(OH)2D] would be considered toxic and potentially fatal to a non-pregnant person. And, this conversion is optimized when she has enough vitamin D3 to sustain a serum 25(OH)D of 40 ng/ml (100 nmol/L)…
There are many physiological processes that occur during pregnancy and at no other time in the life cycle. One of these processes is a specific rate of vitamin D conversion that is allowed to optimize only in situations where there is enough vitamin D3 available. While vitamin D is necessary for all stages of the life-cycle, numerous studies have found that higher vitamin D levels during (and even before) pregnancy reduce the risk of adverse maternal and infant outcomes, and can even have a life-long effect on the baby.
Pregnancy’s Unique Need of Vitamin D
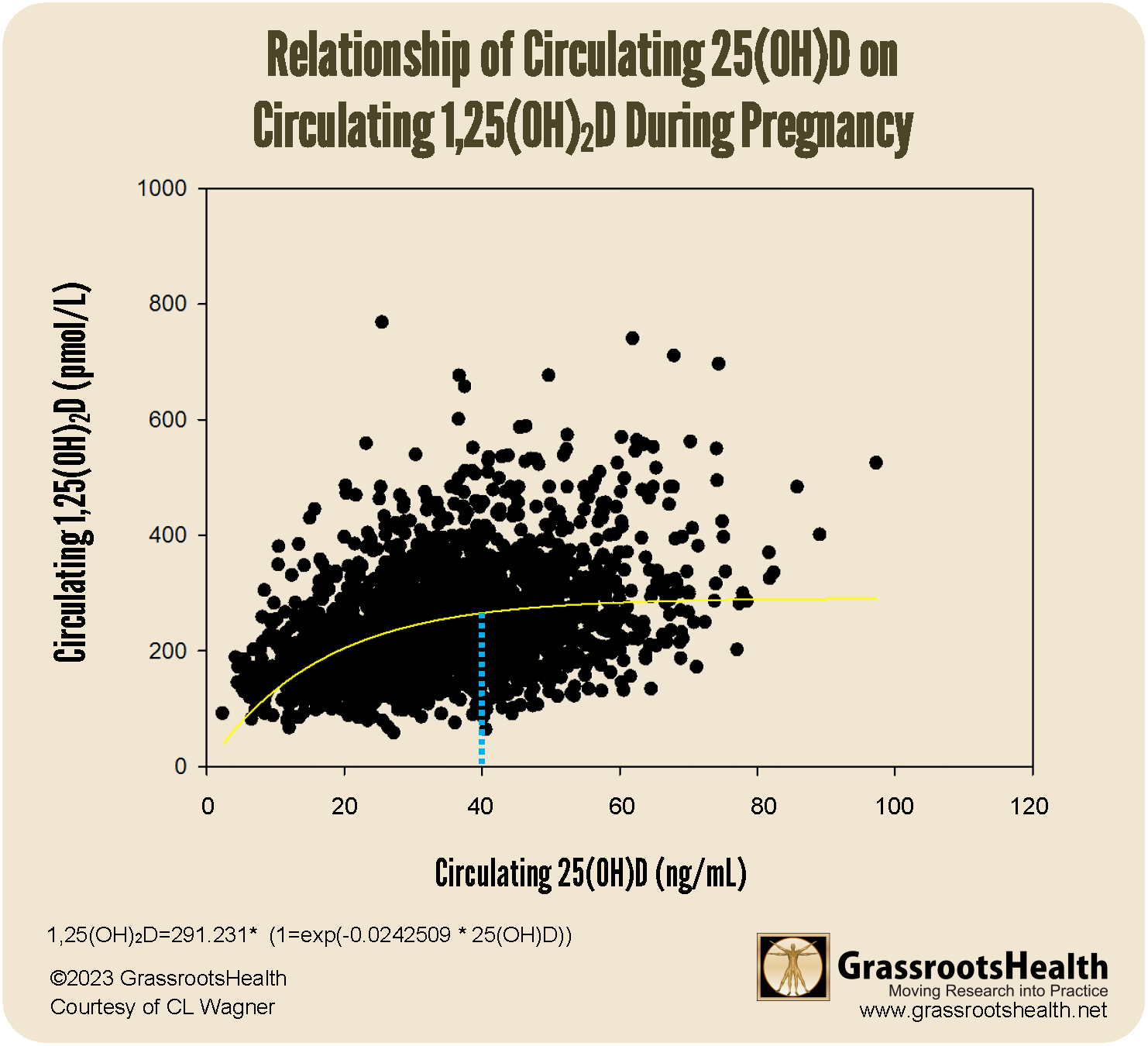
During pregnancy, conversion of 25(OH)D to the hormonal form, 1,25(OH)2D, increases so that by 12 weeks, levels in the blood are triple that of normal, non-pregnant female and normal male subjects. In a non-pregnant person, these levels would alter calcium concentrations in the blood and result in toxicity and potential death, but these are perfectly normal levels during pregnancy. Furthermore, the rise in 1,25(OH)2D is independent of the calcium system, nor is it controlled by parathyroid hormone, which is the only time in the lifecycle that this un-coupling occurs. Further observation has revealed that the direct influence of 25(OH)D (up to ~40 ng/ml) on 1,25(OH)2D levels is also unique to pregnant women.
The chart below illustrates the conversion of 25(OH)D to 1,25(OH)2 observed during pregnancy. The inflection point, where conversion switches from first order to zero order kinetics, can be seen at 40 ng/ml (100 nmol/L) 25(OH)D. This is the point at which conversion of 25(OH)D into 1,25(OH)2 becomes independent of 25(OH)D concentration and 1,25(OH)2 production is optimized, indicating a specific need for serum levels of at least 40 ng/ml in pregnant women.
What Happens When Vitamin D3 is Plentiful in Pregnancy?
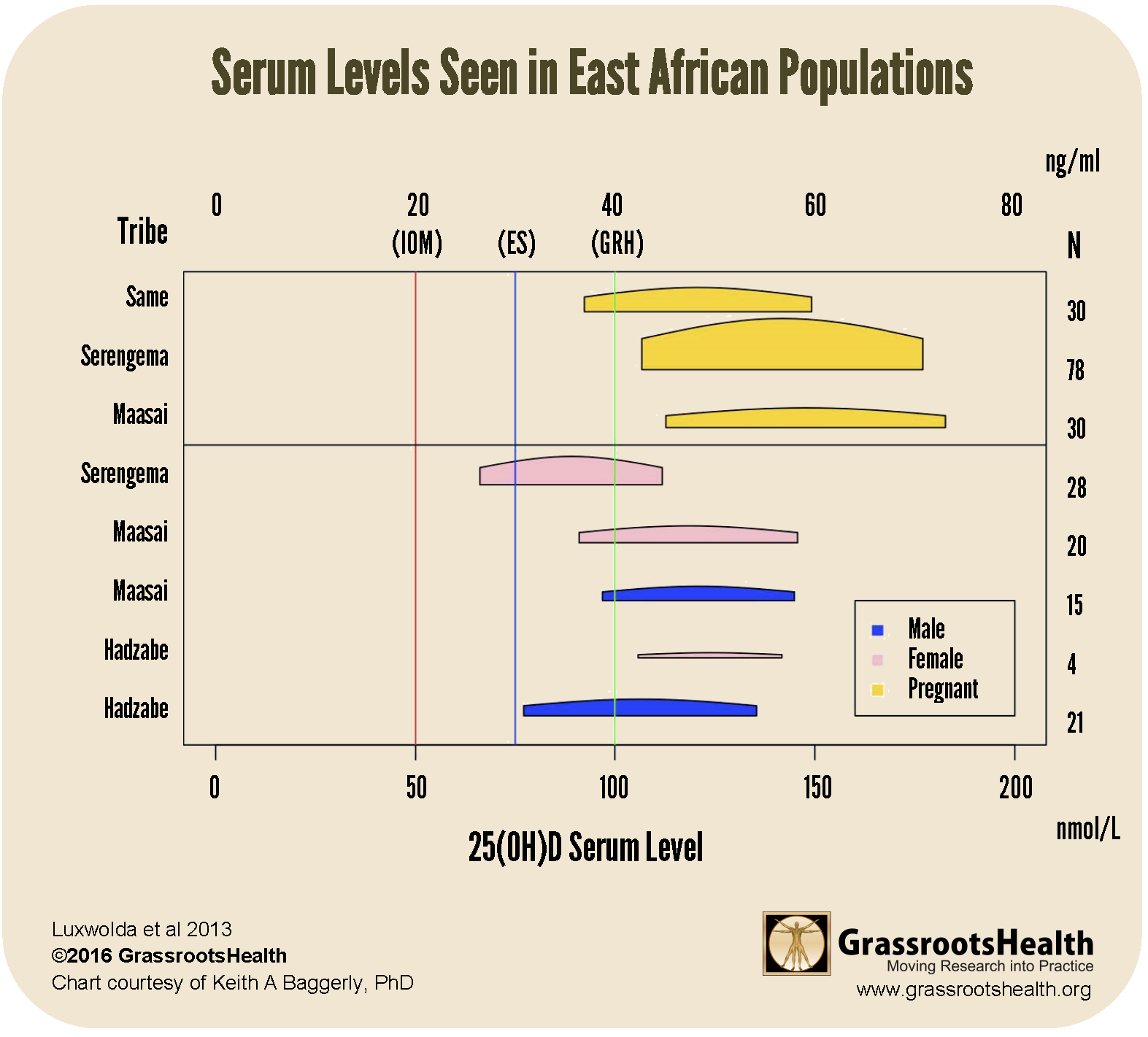
A study by Luxwolda et al. perfectly illustrates what vitamin D levels naturally occur in pregnant women, compared to the rest of the population, when there is plentiful vitamin D3. The study investigated the vitamin D status across the life cycle in various East African populations to determine what serum 25(OH)D level represents sufficient status among populations whose lifestyle closely matches that of our ancestors; notice the average serum 25(OH)D level of this population as a whole is at least 40 ng/ml. The chart below illustrates the levels Luxwolda found in these African tribes, which are much higher than what is currently accepted by the National Academy of Sciences (previously the IOM) and most medical institutions (and are very close to GrassrootsHealth’s recommended 40-60 ng/ml). Further, 25(OH)D levels in pregnancy (shown in yellow) are far higher than in non-pregnant individuals, indicating the higher vitamin D need for the mother during pregnancy.
What Happens when Vitamin D3 is Lacking? (What is Meant to Happen CAN’T Without Enough Vitamin D)
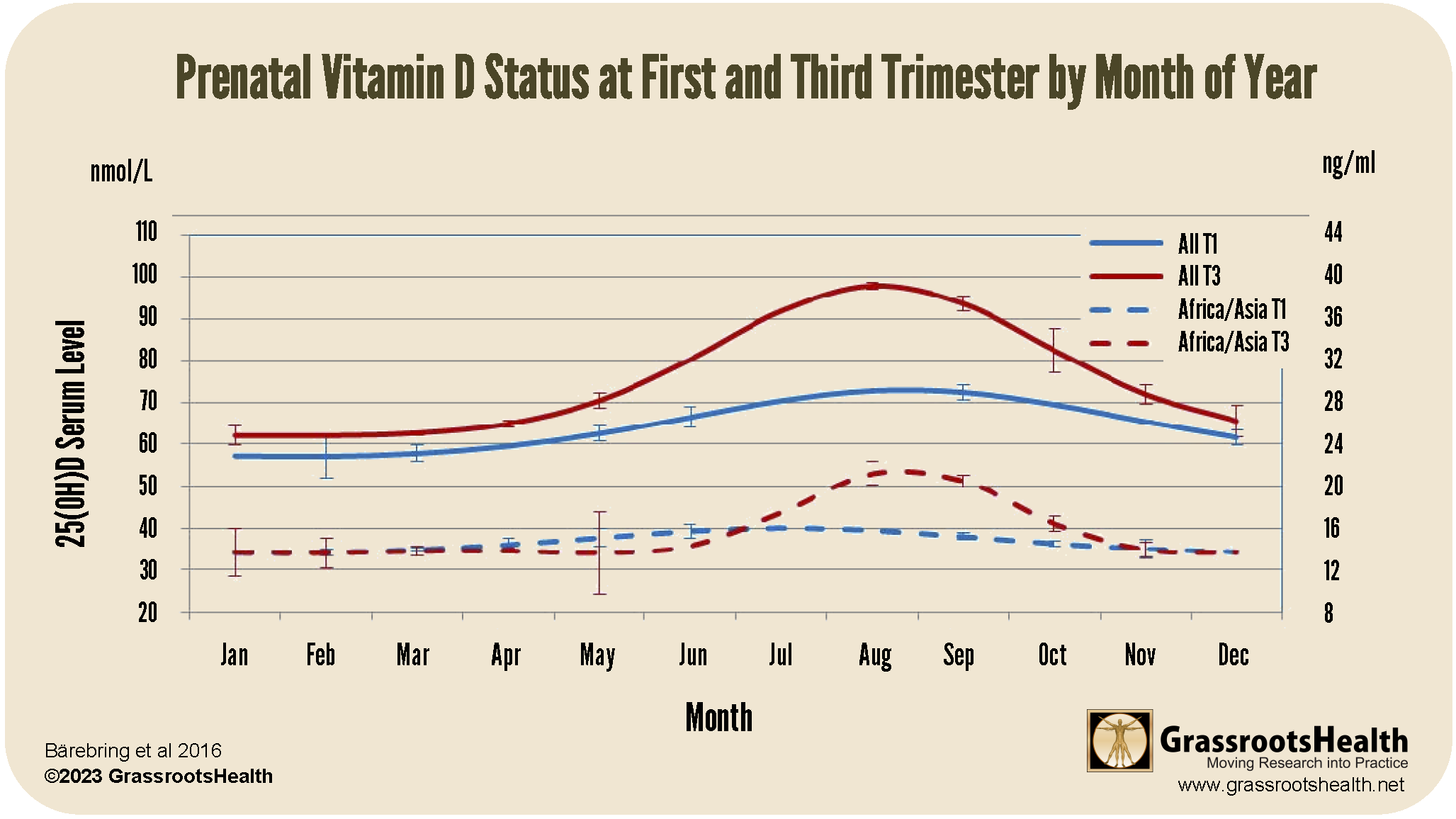
A study by Bärebring et al. measured the vitamin D status of pregnant women in Sweden during their first (T1) and third (T3) trimesters, and compared T1 and T3 vitamin D status by month of year. Two blood samples were collected from each participant – T1 before 17 weeks gestation, and T3 after 31 weeks gestation.
The chart from this study, seen below, illustrates that the rise in 25(OH) vitamin D concentrations, especially during the third trimester of pregnancy, peaked in the summer months, when vitamin D3 from sunshine was more plentiful. Also, the rise was more pronounced in T3 than T1, indicating increased conversion and a greater need for vitamin D towards the end of pregnancy.
This chart clearly shows how 25(OH)D was limited during the non-summer months, especially in the third trimester, when vitamin D3 was less available to the women.
These differences raise the question — if the women in this study had more availability to vitamin D3 throughout the seasons of their pregnancy (such as through supplementation), especially in the third trimester, would seasonal variability in vitamin D levels have been as great, or would all pregnant woman have experienced peak T3 serum levels?
Another important finding from this study was that the resulting 25(OH) vitamin D levels confirmed the high prevalence of deficiency among pregnant women; 10% of all, 51% of women born in Africa, and 46% of women born in Asia were severely deficient (<12 ng/ml or <30 nmol/L). How are these low levels of vitamin D affecting their resulting 1,25(OH)2D levels, which we previously showed is meant to increase substantially in pregnancy? How is this lack of prenatal vitamin D3 affecting the health of the pregnancy and baby?
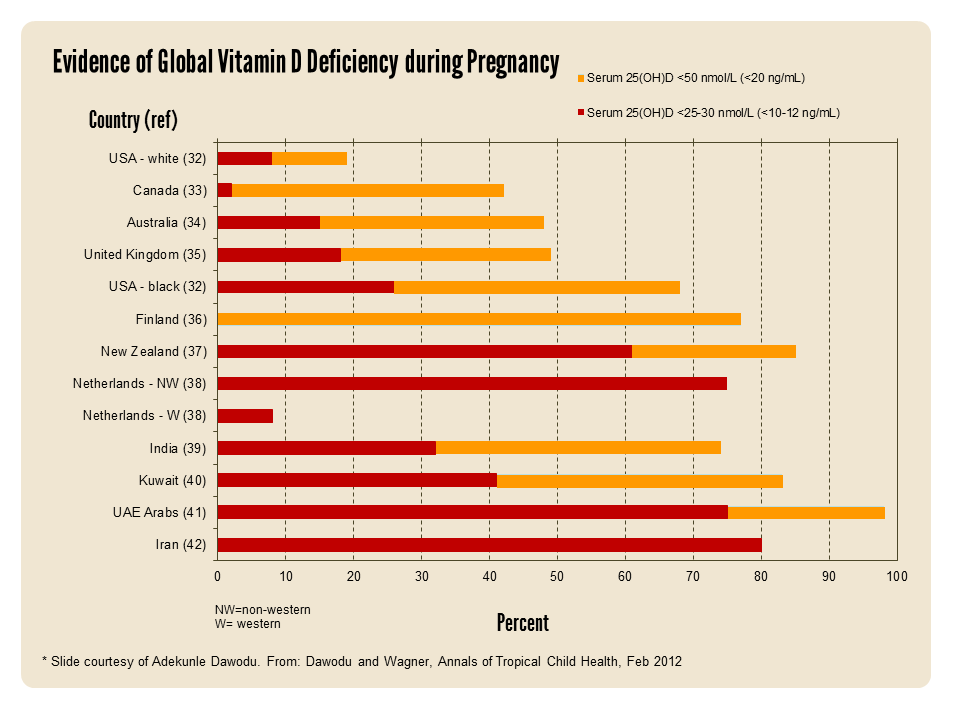
Unfortunately, vitamin D deficiency among pregnant women is common world-wide. The chart below displays the incidence of vitamin D deficiency (below 20 ng/ml) and severe vitamin D deficiency (less than 10-12 ng/ml) in pregnant women world-wide. Countries most affected include the United Arab Emirates, Iran, the Netherlands (NW) and New Zealand.
How Did We Get Here? A Major Problem with a Simple Solution
In an editorial titled “Substantial Vitamin D Supplementation Is Required during the Prenatal Period to Improve Birth Outcomes,” Hollis and Wagner state
“The amount of vitamin D supplemented during pregnancy has long been a contentious subject due to the false association of vitamin D being a teratogen leading to Williams Syndrome. This association, which is now known to be false, has caused generations of obstetricians and healthcare providers to fear vitamin D. Several studies have now clearly demonstrated vitamin D is safe at doses up to and exceeding 4400 IU/day. In all of these studies, NOT A SINGLE ADVERSE EVENT has been associated with vitamin D supplementation. Thus, it is now known that this dose of vitamin D can be safely administered during pregnancy. In fact, this level of supplementation is required during pregnancy to maintain a circulating level of 25(OH)D at a minimum of 40 ng/mL, which is required to support the optimal production of 1,25(OH)2D during pregnancy.”
Correct Vitamin D Deficiency Before Pregnancy Occurs
48 international vitamin D scientists and researchers have agreed on the importance of having a vitamin D serum level between 40-60 ng/ml (100-150 nmol/L) to prevent disease and promote health, as issued in our Scientists’ Call to D*action. This recommendation is higher than that of the National Academy of Sciences (previously the Institute of Medicine), who defines vitamin D deficiency as a serum level of less than 20 ng/ml (50 nmol/L). Even based on this lower recommendation, vitamin D deficiency remains a global epidemic – one that especially affects pregnant women and their unborn children – to be discussed further in an upcoming post.
Measure Vitamin D Levels NOW!
Measuring our levels of vitamin D and other important nutrients and health markers can be considered one way to check-in with our health status and guide us towards the steps to take next in improving and supporting our health.
 Having and maintaining healthy vitamin D levels and other nutrient levels can help improve your health now and for your future. Choose which to measure, such as your vitamin D, omega-3s, and essential minerals including magnesium and zinc, by creating your custom home test kit today. Take steps to improve the status of each of these measurements to benefit your overall health. You can also track your own intakes, symptoms and results to see what works best for YOU.
Having and maintaining healthy vitamin D levels and other nutrient levels can help improve your health now and for your future. Choose which to measure, such as your vitamin D, omega-3s, and essential minerals including magnesium and zinc, by creating your custom home test kit today. Take steps to improve the status of each of these measurements to benefit your overall health. You can also track your own intakes, symptoms and results to see what works best for YOU.
Enroll and test your levels today, learn what steps to take to improve your status of vitamin D (see below) and other nutrients and blood markers, and take action! By enrolling in the GrassrootsHealth projects, you are not only contributing valuable information to everyone, you are also gaining knowledge about how you could improve your own health through measuring and tracking your nutrient status, and educating yourself on how to improve it.

 Did you know? By week 12, a pregnant woman’s body converts more vitamin D than ‘normal,’ so that the level of the hormonal form of vitamin D [1,25(OH)2D] would be considered toxic and potentially fatal to a non-pregnant person. And, this conversion is optimized when she has enough vitamin D3 to sustain a serum 25(OH)D of 40 ng/ml (100 nmol/L)…
Did you know? By week 12, a pregnant woman’s body converts more vitamin D than ‘normal,’ so that the level of the hormonal form of vitamin D [1,25(OH)2D] would be considered toxic and potentially fatal to a non-pregnant person. And, this conversion is optimized when she has enough vitamin D3 to sustain a serum 25(OH)D of 40 ng/ml (100 nmol/L)…